Creatinine
| Structural formula | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|

|
|||||||||||||||||||
| General | |||||||||||||||||||
| Surname | Creatinine | ||||||||||||||||||
| other names | |||||||||||||||||||
| Molecular formula | C 4 H 7 N 3 O | ||||||||||||||||||
| Brief description |
white solid |
||||||||||||||||||
| External identifiers / databases | |||||||||||||||||||
|
|||||||||||||||||||
| properties | |||||||||||||||||||
| Molar mass | 113.12 g mol −1 | ||||||||||||||||||
| Physical state |
firmly |
||||||||||||||||||
| Melting point |
305 ° C (decomposition) |
||||||||||||||||||
| solubility |
|
||||||||||||||||||
| safety instructions | |||||||||||||||||||
|
|||||||||||||||||||
| Thermodynamic properties | |||||||||||||||||||
| ΔH f 0 |
−238.5 kJ / mol |
||||||||||||||||||
| As far as possible and customary, SI units are used. Unless otherwise noted, the data given apply to standard conditions . | |||||||||||||||||||
Creatinine - in the internationalized notation creatinine - is a metabolic product . It is formed as a strongly basic amide ( lactam ) from the acid creatine in aqueous solution and irreversibly in muscle tissue . In the body, it is a metabolite that must be passed through urine , so it has to be excreted through the kidneys and urine.
Creatinine as a metabolic parameter
Creatinine is an important kidney retention parameter in laboratory medicine . It is excreted with the urine at a relatively constant rate of 1.0 to 1.5 g per 24 h, mostly in the glomerular manner, and sometimes actively tubular in the case of high plasma values (of serum creatinine ) . The excretion rate, however, is an individual constant that depends in particular on muscle mass and age and is therefore medically more suitable for monitoring the progression. Typical values for the excretion rate are 21 to 27 mg / kg / 24 h for an age between 20 and 30 years, 6 to 13 mg / kg / 24 h for an age over 90 years, for children the formula 15.4 applies approximately + 0.46 × age (mg / kg / 24h).
Numerous parameters determined in the urine are related to the amount of creatinine excreted. However, this creatinine reference is not suitable for all substances.
The blood plasma level is around 0.7 mg / 100 ml (50 to 120 μmol / l), but it also depends on factors such as muscle mass, physical activity, age, gender and kidney function. When assessing kidney function, it is important that the creatinine value only rises above 50% when the glomerular filtration rate (GFR) is restricted , or only then becomes significant. A “normal” creatinine level does not rule out the onset of renal insufficiency.
In laboratory medicine one makes the determination of the creatinine clearance , i. H. the creatinine excretion via the kidneys ( renal clearance ), and thus a more reliable parameter for assessing kidney function, to be able to calculate the GFR. Creatinine is not reabsorbed tubularly, i.e. practically every filtered molecule ultimately appears in the urine . Since the plasma concentration of creatinine is not constant (see above), a venous blood sample is required in addition to the 24-hour urine collection in order to be able to make precise statements about the GFR.
A simpler but less precise estimate of the GFR is given by determining the plasma creatinine concentration alone. A non-linear relationship between GFR and the concentration in the blood plasma is used here. Both the formula by Donald W. Cockcroft and Henry Gault ( Cockcroft-Gault formula ) and the more recent ones by Mawer, Björnsson, Hull and Martin also include gender, age and body weight. The MDRD formula developed in 1999 by the Modification of Diet in Renal Disease Study Group (MDRD) does not include body weight. The Schwartz formula is well suited for determining the GFR in children .
Medicines can also influence the creatinine level; this is increased, for example, by opiates and diuretics . In contrast to creatine , creatinine is completely meaningless for muscle building.
Creatinine excretion
Creatinine is excreted via the kidneys. Renal clearance is a measure of excretion via the kidneys ( Latin ren ) . When determined using urine collection , the creatinine clearance is calculated as follows:
With
- : Creatinine clearance in ml / min
- : Urine creatinine in mg / dl
- : Urine volume in ml
- : Serum creatinine in mg / dl
- Time: collection time, usually given in minutes.
The Cockcroft-Gault formula provides an estimate of creatinine clearance:
With
- , : see above
- Age: Age in years
- Weight: body weight in kg.
Creatinine clearance may be too low in the following cases:
- Kidney disease
- Kidney damage due to fluid loss (diarrhea, vomiting, thirst, shock)
- Excessive meat intake
- Prolonged physical work before blood draw
And too high in these:
- In the early phase of diabetes mellitus
- During pregnancy
quantification
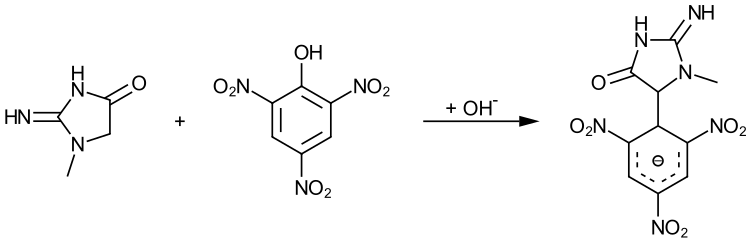
The determination of the creatinine content in foods with a lean meat content can be done photometrically. For this purpose, the sample is first processed in an acidic manner in order to cyclize any creatine into creatinine. The Maillard products (e.g. hydroxymethylfurfural ) formed in side reactions interfere with the photometric determination and are therefore separated off by means of column chromatography and ether extraction. The creatinine is then reacted with picric acid in an alkaline environment, creating a Meisenheimer complex that can be determined photometrically.
Individual evidence
- ↑ Entry on 1-METHYLHYDANTOIN-2-IMIDE in the CosIng database of the EU Commission, accessed on March 4, 2020.
- ↑ a b c d e Creatinine data sheet (PDF) from Merck , accessed on January 19, 2011.
- ↑ a b entry on creatinine. In: Römpp Online . Georg Thieme Verlag, accessed on November 11, 2014.
- ↑ David R. Lide (Ed.): CRC Handbook of Chemistry and Physics . 90th edition. (Internet version: 2010), CRC Press / Taylor and Francis, Boca Raton, FL, Standard Thermodynamic Properties of Chemical Substances, pp. 5-26.
- ↑ JP Kampmann, JM Hansen: Glomerular filtration rate and creatinine clearance. In: British journal of clinical pharmacology. Volume 12, Number 1, July 1981, pp. 7-14, PMID 6788057 , PMC 1401744 (free full text).
- ↑ This is why creatinine is one of the so-called non-threshold substances. Source: Franz Volhard : The bilateral haematogenic kidney diseases . In: Gustav von Bergmann , Rudolf Staehelin (Ed.): Handbook of internal medicine. 2nd Edition. Published by Julius Springer, Berlin / Heidelberg 1931, Volume 6, Part 1, p. 5. There it is forgotten that in compensatory oliguria or anuria, all filtered substances are completely or partially reabsorbed in a tubular manner and do not appear in the urine.
- ^ DW Cockcroft, MH Gault: Prediction of creatinine clearance from serum creatinine. In: Nephron. Volume 16, Number 1, 1976, pp. 31-41, PMID 1244564 . (Review article: PDF file )
- ^ MH Gault, DW Cockcroft: Letter: Creatinine clearance and age. In: The Lancet . Volume 2, Number 7935, September 1975, pp. 612-613, PMID 51444 .
- ↑ HL Kim, SK Shah u. a .: Estimation and prediction of renal function in patients with renal tumor. In: The Journal of Urology . 181, 2009, pp. 2451-2460. doi : 10.1016 / j.juro.2009.01.112 . PMID 19371883 .
- ^ AS Levey, JP Bosch et al. a .: A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. In: Annals of internal medicine . Volume 130, Number 6, March 1999, pp. 461-470, PMID 10075613 .
- ↑ GJ Schwartz, A. Muñoz et al. a .: New equations to estimate GFR in children with CKD. In: Journal of the American Society of Nephrology . Volume 20, number 3, March 2009, pp. 629-637, doi : 10.1681 / ASN.2008030287 . PMID 19158356 . PMC 2653687 (free full text).
- ^ WE Haefeli: Drug therapy for renal insufficiency. (PDF; 2.9 MB) Heidelberg University, accessed on August 6, 2012
- ↑ R. Matissek, G. Steiner, M. Fischer: Lebensmittelanalytik . 5th, completely revised edition. Springer Spectrum, Berlin / Heidelberg 2014, ISBN 978-3-642-34828-0 , p. 387-390 .
Web links
- Laborlexikon Trade journal for laboratory medicine: Creatinine in serum
- Universitätsklinikum Heidelberg - Dose adjustment in case of renal insufficiency - Calculation of drug dosage based on creatinine values