Hypothyroidism

Under hypothyroidism or hypothyroidism refers to a lack of supply of the body with the thyroid hormones triiodothyronine (T 3 ) and thyroxine (T 4 ). Usually an underactive thyroid ( hypothyroidism ) is responsible for this. With this hormonal situation, numerous metabolic functions of the body take place more slowly than normal. The consequences are reduced physical and mental performance. The disease is usually detected by blood tests and is easily treatable. The opposite, an oversupply of thyroid hormones, is called hyperthyroidism .
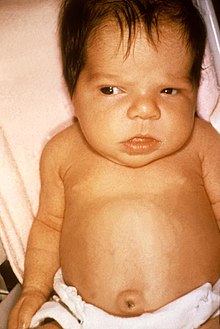
In children, hypothyroidism, acquired very early or congenitally, can lead to physical and mental development delays, the full picture of which, if not treated, is known as cretinism .
Definitions
There are two different definitions of hypothyroidism , although only one of the two is usually given in the specialist literature. After the first, the thyroid produces too few hormones (hypothyroidism), after the second, the body has an insufficient supply of thyroid hormones. The first is based on the function of the thyroid gland. The second, on the other hand, is oriented towards the supply of body cells.
The same applies to the English equivalent of hypothyroidism : A. Thyroid gland produces too few hormones - or B. Insufficient influence of hormones on body cells. However, both definitions are given as alternative definitions in at least one textbook:
"Hypothyroidism is the result of inadequate production of thyroid hormone or inadequate action of thyroid hormone in target tissues."
history
The understanding of the function of the thyroid gland developed slowly. Until the second half of the 19th century, it was regarded as the "secondary gland of the respiratory organs ", the function of which was unclear. In 1896 Eugen Baumann found organically bound iodine in the thyroid gland, the so-called iodothyrin (or thyreoiodine) and characterized it as the active component of the thyroid gland. Little was known about its effect in 1898 ( Robert Hutchison ); it was used for experimental purposes until the 20th century. In 1911, Harry E. Alderson described the development of myxedema in hypothyroidism as the subcutaneous infiltration of a mucus-like substance, which is subsequently replaced by an excessive formation of connective tissue . In addition, he found that ichthyosis is associated with it and successfully used thyroid extracts and iodothyrin for therapy.
The discovery of the thyroid hormone thyroxine is attributed to Edward Calvin Kendall in 1914. He had crystallized an active component out of iodothyrin and named it thyroxin. The best way to determine hypothyroidism by examining the blood during this time is considered to be accelerated blood coagulation as well as a decrease in neutrophils and an increase in lymphocytes . The direct measurement of thyroxine in the blood has been possible since the 1960s.
François-Emmanuel Fodéré (1764–1835) assumed that low-iodine air was the cause of childhood hypothyroidism, the untreated course of which is known as cretinism . Emil Theodor Kocher (1841–1917) described in 1883 the occurrence of a "cretin-like change" during the follow-up examination of patients who had undergone thyroid surgery. In the 1890s, Julius Wagner-Jauregg (1857–1940) carried out fundamental studies on cretinism in Styria and treated it with thyroid extracts. The since 1918 in Nikolaital by Otto Bayard (1881-1957) and then in 1922 in Appenzell Outer Rhodes by Hans Eggenberger (1881-1946), and later throughout Switzerland enforced prevention with iodized salt had global pioneer character. As a result, no more cretins were born in Switzerland .
Basics
In healthy people, the thyroid releases the thyroid hormones - thyroxine (T 4 ) and triiodothyronine (T 3 ) - into the blood as required. The production of these hormones is controlled by the thyrotropic control loop . In the thyroid gland of a reduction in the pituitary gland (causes pituitary hormone formed) thyrotropin (TSH) a reduction in the production of thyroid hormones.
The thyroid gland needs iodine to build up thyroxine and triiodothyronine . The adult requirement is around 200 μg per day. A sufficient intake with the normal diet is not always guaranteed in Germany.
The amount of hormones produced fluctuates considerably within the group of people with healthy thyroid gland (normal population), which means that the reference range of the laboratory results is relatively large. The fluctuations in measurements with the same person are much smaller.
The thyroid hormones (T 3 and T 4 ) released from the thyroid gland into the blood are mostly bound to different proteins (mainly TBG , TBPA and albumin ) and are biologically inactive. Only about 1 ‰ of the thyroid hormones in the blood circulate freely (fT 3 and fT 4 ). Only the free thyroid hormones are biologically active.
The thyroid hormones physiologically increase the basal metabolic rate , the sensitivity of the heart to catecholamines , calcium and phosphate metabolism as well as the excitability of muscle and nerve cells and inhibit the formation of new proteins and glycogen .
Classification and causes
| Classification according to ICD-10 | |
|---|---|
| E00 | Congenital iodine deficiency syndrome |
| E00.0 | Congenital iodine deficiency syndrome, neurological type |
| E00.1 | Congenital iodine deficiency syndrome, myxedematous type |
| E00.2 | Congenital iodine deficiency syndrome, mixed type |
| E00.9 | Congenital iodine deficiency syndrome, unspecified |
| E03 | Other hypothyroidism |
| E03.0 | Congenital hypothyroidism with diffuse goiter |
| E03.1 | Congenital hypothyroidism without goiter |
| E89.0 | Hypothyroidism after medical measures |
| ICD-10 online (WHO version 2019) | |
A congenital hypothyroidism - statistically are about 0.2 ‰ of all newborns affected - is caused by a missing or insufficient thyroid-scale ( aplasia or dysplasia very rare), insufficient hormone biosynthesis or -ausschüttung, by a hormone resistance due to T 3 -Rezeptordefekten. Temporary hypothyroidism in the newborn child can be iatrogenic due to increased iodine exposure after birth (e.g. due to disinfectants such as povidone iodine ) or iodine deficiency in the mother. In the latter case, an accompanying goiter (or goiter) is typical.
The acquired hypothyroidism can occur even in childhood. Their incidence in Germany is around 0.25–1% and increases with age. A distinction is also made between the primary, secondary and tertiary forms. From the primary hypothyroidism is, generally speaking, when the thyroid is the cause of hypothyroidism even, d. H. when the secretion capacity of the thyroid gland is too low for the demands of the organism. This form includes hypothyroidism that develops after a thyroid operation or radioiodine therapy . Furthermore, it can be iatrogenic through drugs that inhibit the function of the thyroid gland ( thyreostatics ) or extreme selenium or iodine deficiency (the most common preventable cause of retardation in children worldwide) and through atrophic thyroiditis (e.g. autoimmune thyroiditis , type Hashimoto's disease ). In the rare secondary hypothyroidism there is a lack of the thyroid-stimulating hormone TSH , which is produced in the pituitary gland ( hypopituitarism ). Tertiary hypothyroidism is a rarity and is characterized either by a lack of thyrotropin releasing hormone ( TRH ) or by an interruption of the portal vascular system between the hypothalamus and pituitary gland ( Pickardt's syndrome ).
Clinical picture
As with hyperthyroidism, there are different degrees of severity of hypothyroidism: They range from latent or compensated (thyroid hormone level normal, but TSH level increased) to subclinical (thyroid hormone level, although decreased, but without symptoms) and manifest (decreased thyroid hormone level accompanied by corresponding symptoms) to towards life-threatening deficiency.
Congenital hypothyroidism
- → Main article Congenital hypothyroidism
At birth, the children are usually clinically normal because the children still have the mother's thyroid hormones in their bloodstream. In the first few weeks of life they fall e.g. B. by increasing drinking weakness, sedentary lifestyle , constipation and a large, visible tongue. Prolonged neonatal jaundice (jaundice neonatorum prolongatus) is also typical. The children appear “very good”, don't scream and sleep a lot. A slower heart rate (bradycardia), doughy skin, persistence of the hair on the head of the newborn and a large belly with an umbilical hernia are also other signs, as well as a typical facial expression with a sunken nose and a balloon forehead. Last but not least, newborns can have attacks of suffocation or impaired muscle development. If a child grows up without the hypothyroidism being recognized, mental and physical development disorders (e.g. impaired speech, hearing loss, delayed puberty) together with reduced growth in height are to be expected.
Acquired hypothyroidism
Initially, the symptoms are often not noticeable (subclinical), as the clinical picture in adults usually develops slowly. Symptoms consist of decreased performance, poor concentration, weakness, listlessness , tiredness, constipation and increased sensitivity to cold. An underactive thyroid can also cause depression . Affected patients complain of depressive moods, memory loss and loss of appetite. Therefore, psychotherapists should have the thyroid function clarified in depressed patients. In addition, the typical myxedema - an edematous-pasty thickening of the skin - can often be observed. Dry or rough skin, rough voice, slow speech, sluggishness , chronic constipation , swelling of the eyelids and face, slowing of the pulse and reflexes, and low blood pressure and weight gain can be observed. Menstrual cycle disorders and fibro-cystic mastopathy can occur in women, and libido and erectile dysfunction in men . If children are affected, more or less pronounced development delays occur.
The most severe and life-threatening form is the hypothyroid coma ( myxedema coma ) , which is typically accompanied by very quiet heart sounds, slow heartbeat and low blood pressure, diffuse myxedema , reduced body temperature , weakened or extinguished reflexes and shallow breathing.
Hypothyroid myopathy
Changes in the muscles (myopathy) are found in 30–80% of cases of hypothyroidism, especially in the case of long-standing and untreated disease.
Four different forms of myopathy can be distinguished:
- Hoffmann Syndrome
- Kocher-Debré-Semelaigne syndrome
- Atrophic shape
- Myasthenic form
diagnosis
- → Main article Examination of the thyroid gland
Congenital hypothyroidism is looked for in newborn screening on the 4th to 5th day of life by measuring the thyrotropin level (TSH level).
Since hypothyroidism in children and adults is defined by a deficiency in thyroid hormones, laboratory diagnostics play a decisive role in addition to anamnesis , clinical symptoms and imaging procedures (particularly sonography and scintigraphy ). Clinical symptoms in adults do not always correlate with evidence of laboratory changes. In children, they are a definite indicator of impending developmental disorders.

As a rule, the thyroid gland produces insufficient amounts of thyroid hormones in hypothyroidism, as already explained above. The thyrotropic control loop then leads to an increase in the release of TSH, which in turn is the signal for the thyroid gland to increase the production of thyroid hormones. The sole determination of the basal TSH level in the blood is therefore suitable as a screening parameter. If this is normal, a further determination of the thyroid hormones can be dispensed with in a clinically normal patient. According to the guidelines of relevant medical societies (as of March 2016), the normal range (reference range) of the TSH level in healthy adults is 0.4 - 4.5 mU / l, but during pregnancy with lower upper values of 2.5 in the first Third, 3.0 in the 2nd third and 3.5 in the 3rd third. The need for thyroid hormones usually increases during pregnancy, so that in the case of hypothyroidism (in around 0.4% of pregnant women) the values should be checked regularly during and after pregnancy.
The latent (asymptomatic) or subclinical hypothyroidism is defined by a fT 4 is value in the normal range and TSH above 4.5 mU / l, the latter provided twice within 3 to 6 months increased. The prevalence of latent hypothyroidism in the general population is estimated to be between 3 and 10%. However, there is no sufficiently proven, increased risk of disease - in connection with an advantage in treatment - as long as TSH is below 10.0 mU / l. The most common cause of latent hypothyroidism is autoimmune thyroiditis. For aetiological clarification, an antibody determination can therefore be carried out once in latent hypothyroidism (antibodies against thyroid peroxidase, "anti-TPO"; in special situations also anti-thyroglobulin antibodies). However, knowledge of the presence of autoantibodies has little clinical relevance and the detection of these autoantibodies is usually of no relevance for further treatment. A thyroid sonography can be dispensed with in the case of latent hypothyroidism, provided that no thyroid nodules can be felt.
It should also be noted that the upper value of the TSH normal range in adults increases steadily with age, namely - according to an analysis of an extensive data collection in the USA - between the age groups 20-29 and 80+ from 3.5 to 7, 5 mU / l. If this age dependency is not taken into account, there is a considerable risk that a diagnosis of "latent hypothyroidism" is not justified in patients aged 50 and over .
The classic case of manifest (clearly visible) hypothyroidism is a decrease in fT 3 and fT 4 below their normal range together with an increase in the TSH level (> 4.0 mU / l) and the corresponding clinical symptoms. However, the determination of TSH and fT 4 are sufficient laboratory parameters for the detection of hypothyroidism .
In congenital hypothyroidism , the concentration of thyroglobulin in the blood and the iodine content in the urine are also determined and a thyroid scintigraphy with iodine 123 is carried out.
In acquired hypothyroidism , measurements of TPO-AK ( antibodies against thyroid peroxidase ) and antibodies against thyroglobulin (Tg-AK), as well as sonography as an imaging method, are recommended to clarify the cause of the hypothyroidism. Further investigation options only play a role in special cases and are presented there in the respective main article.
therapy
In congenital hypothyroidism , thyroxine must be given for life. It should be started as early as possible.
The acquired hypothyroidism , whether subclinical or manifest is also usually come with a lifetime replacement therapy (substitution) with T 4 treatment. However, the benefit of a therapy for subclinical hypofunction of the thyroid has not yet been sufficiently proven (as of March 2016) and is only recommended in justified individual cases.
The dose must be adjusted individually in all cases. It starts with a low dose of thyroid hormone and then gradually increases. This procedure has proven itself in terms of avoiding side effects . Long-term substitution treatment (usually between 50 and 150 µg per day) is considered to be well adjusted when the patient feels comfortable and the basal TSH level (after six to eight weeks at the earliest) is in the normal range (see diagnosis). The further course is usually checked every six months and then annually if the attitude is good. In children, the control cycle is age-dependent. In addition, close controls of growth, weight and psycho- and somatomotor development are indicated. In the case of acquired hypothyroidism, a four to six week elimination attempt can be made in the child after about 2 years .
When Myxoedema coma (coma hypothyreotes) is an acute, life-threatening, emergency medical disease. Therefore, therapy begins immediately, without waiting for the result of hormone laboratory tests. Even patients with the clinical signs of a myxedema coma should be admitted to an intensive care unit and treated immediately . In both cases, therapy includes safeguarding vital functions , administering glucocorticoids , glucose , monitoring and, if necessary, balancing the electrolyte balance, normalizing body temperature (often hypothermia ) and intravenous administration of thyroxine.
Over-treatment
Unnecessary or overdosed treatment with thyroxine (T 4 ) is a common problem. It affects around 15–20% of the patients treated with it. In addition to a lack of medical control, a frequent cause is also the unauthorized change of the dose by the patient according to his feelings and without considering their blood values. Risks of overdose are an increased likelihood of atrial fibrillation ( irregular heartbeat ), angina pectoris (disturbance of the blood flow to the heart), heart failure , nervousness , palpitation (heartbeat), decrease in bone mineral density and bone fracture .
The magnitude of the problem of widespread unnecessary or overdosed treatment with thyroxine (T 4 ) in Germany was documented in the 2014 Drug Ordinance Report . Thereafter, at least 4.1 million people were permanently supplied with thyroid hormones.
prophylaxis
A sufficient supply of iodine through diet has a prophylactic effect in the forms of hypothyroidism caused by iodine deficiency . The recommended daily amount of iodine for adults is around 200 μg. During pregnancy, the mother's body needs more iodine (up to 300 μg per day). Sea fish and iodized table salt in particular contain a lot of iodine, which is why secondary hypothyroidism is rare near the sea. In iodine deficiency areas such as B. in the Alps , a corresponding dietary supplement is recommended (in Germany) or regulated by the state. In Switzerland and Austria, but also in the USA, there have been laws regulating the supply of iodine since 1920, e.g. B. by prescribing the iodine content in table salt. The decrease in hypofunction was bought at the cost of a short-term increase in hyperthyroidism. Long-term studies have shown, however, that these are comparatively low.
The scientific evaluation of the state salt iodination in China from 1985 to 2014 showed, in addition to the known positive effects, also significant negative effects on the thyroid gland in the event of a local excess of iodine, which also includes an increased risk of hypothyroidism.
Hypothyroidism in animals
In veterinary medicine, hypothyroidism is of greater importance , especially in dogs . In contrast, the frequency of hypothyroidism caused by iodine deficiency has decreased significantly in recent decades, especially due to the addition of iodine in commercial feed.
In principle, the same causes can be responsible in dogs as in humans, but 95% of the cases are acquired primary hypothyroidism. They are caused by (presumably autoimmune ) inflammation of the thyroid gland or by atrophy of the organ for no apparent cause ( idiopathic hypothyroidism ). Dogs of large breeds are particularly affected. The symptoms usually appear insidious and consist of increasing sluggishness as well as skin and coat changes, in bitches also a lack of heat . The diagnosis is the same as in human medicine, although it should be noted that gray and deerhounds have physiologically lower T4 levels than other dog breeds. In addition, some drugs ( glucocorticoids , anticonvulsants , quinidine , salicylates , phenylbutazone , sulfonamides and X-ray contrast media ) and other diseases can lead to decreased T4 values. The treatment is carried out by giving thyroid hormones.
Sows with hypothyroidism give birth to "naked pigs" with myxedema. "Tonguing" is observed in calves. The cause of this hypothyroidism is a secondary iodine deficiency caused by mustard oil glycosides or feed containing nitrates.
In birds - especially budgies - hypothyroidism caused by iodine deficiency still plays a role in some cases. Clinically, they manifest themselves in shortness of breath, as the enlarged thyroid gland presses on the windpipe, as well as fletching disorders. In parrots , hypothyroidism is discussed in connection with the development of obesity and fletching disorders, as occurs above all in the pink cockatoo. Although these symptoms respond to the intake of thyroxine, thyroid hormone diagnostics in birds are not ready for practice, so that a causal relationship can only be assumed. Hypothyroidism is also more common in turtles in areas with low iodine levels in their drinking water. They are expressed in the formation of myxedema at the base of the neck.
Web links
literature
Guidelines
- O. Okosieme, J. Gilbert, P. Abraham, K. Boelaert, C. Dayan, M. Gurnell, G. Leese, C. McCabe, P. Perros, V. Smith, G. Williams, M. Vanderpump: Management of primary hypothyroidism: statement by the British Thyroid Association Executive Committee. In: Clinical endocrinology. [electronic publication before printing] May 2015, doi: 10.1111 / cen.12824 , PMID 26010808 , (Review), PDF (accessed March 21, 2016).
- JR Garber, RH Cobin, H. Gharib, JV Hennessey, I. Klein, JI Mechanick, R. Pessah-Pollack, PA Singer, KA Woeber: Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. In: Thyroid: official journal of the American Thyroid Association. Volume 22, number 12, December 2012, pp. 1200–1235, doi: 10.1089 / thy.2012.0205 , PMID 22954017 , (free full text).
- Association of Clinical Biochemistry, British Thyroid Association and British Thyroid Foundation: UK guidelines for the use of thyroid function tests (2006) , PDF (accessed March 21, 2016).
- DEGAM guideline No. 18: Increased TSH levels in general practitioners , 2016, PDF
Information for patients and relatives
- American Thyroid Association (ATA): Hypothyroidism - A Booklet for Patients and their Families , 2013, PDF (accessed March 21, 2016).
- DEGAM patient information "Increased TSH value in the family doctor's practice", 2016, PDF (accessed on December 6, 2017).
Individual evidence
- ↑ a b Gerd Herold: Internal Medicine. 2007.
- ^ Hans Bankl: Workbook Pathology III. maudrich, 1998, ISBN 3-85076-536-9 , p. 361. Restricted preview in Google Book Search
- ↑ Andreae, Susanne (contributors): Lexicon of Diseases and Examinations , Georg Thieme Verlag, Stuttgart 2008, ISBN 978-3-13-142962-9 , p. 475.
- ↑ Heiner Greten, Tim Greten, Franz Rinninger (Eds.): Internal Medicine , Georg Thieme Verlag, Stuttgart 2010, ISBN 9783131621832 , p. 510.
- ↑ Baenkler, Hanns-Wolf (contributor): Internal medicine: 299 synopses, 611 tables , Georg Thieme Verlag, Stuttgart 2001, ISBN 978-3-13-128751-9 , p. 804.
- ↑ GK Stalla (Ed.): Therapielexikon Endokrinologie und Metabolic Diseases , Springer-Verlag, Heidelberg 2007, ISBN 9783540300335 , p. 541.
- ^ Walter Siegenthaler (ed.): Siegenthaler's differential diagnosis: internal diseases - from symptom to diagnosis , Georg Thieme Verlag, Stuttgart 2005, ISBN 9783133448192 , p. 493.
- ^ Waltraut Kruse, Gotthard Schettler (Ed.): General Medicine , Walter de Gruyter, Berlin 1995, ISBN 9783110879155 , p. 209.
- ↑ Jürgen Floege, Richard J Johnson, John Feehally: Comprehensive clinical nephrology , Saunders / Elsevier, Philadelphia (USA) 2010, ISBN 9780323081337 , p. 484.
- ^ Pauline M Camacho; Hossein Gharib; Glen W Sizemore: Evidence-based endocrinology , Lippincott Williams & Wilkins, Philadelphia 2007, ISBN 9780781771542 , p. 37.
- ^ Fabrizio Monaco: Thyroid Diseases , CRC Press, Boca Raton (USA) 2012, ISBN 9781439868393 , p. 172.
- ^ Pauline Camacho: Clinical Endocrinology and Metabolism , Manson Publishing, London 2011, ISBN 9781840765854 , p. 20.
- ^ William D. Carey (Ed.): Current Clinical Medicine E-Book. Expert Consult - Online , Elsevier Health Sciences, Philadelphia 2010, ISBN 9781437735710 , p. 416.
- ↑ Anthony P. Weetman (Ed.): Autoimmune Diseases in Endocrinology , Springer Science & Business Media, 2007, ISBN 9781597455176 , p. 137.
- ↑ Kenneth Burman (Ed): Thyroid Disorders and Diseases, An Issue of Medical Clinics - E-Book Elsevier Health Sciences, Philadelphia 2012, ISBN 9781455744152 , p. 203.
- ↑ Albert Kölliker: Handbook of human tissue theory. 1867, p. 480.
- ^ J. Hyrtl: Textbook of anatomy the people. Braumüller court bookseller, Vienna 1863, p. 666.
- ↑ E. Baumann: About the thyroiodine. In: Münchn Med Wschr. Volume 43, 1896, p. 309.
- ^ R. Hutchison: Further Observations on the Chemistry and Action of the Thyroid Gland. In: J Physiol . 1898 July 26; 23 (3), pp. 178-189.
- ↑ Otto v. Fürth, Karl Schwarz: About the effect of iodothyrin on the circulation apparatus. In: Archives for the entire physiology of humans and animals . Volume 124, Numbers 3-5 / August 1908, Verlag Springer Berlin / Heidelberg; ISSN 0031-6768
- ^ HE Alderson: The Skin as Influenced by the Thyroid Gland. In: Cal State J Med. Volume 9, Number 6, 1911, pp. 240-243.
- ^ RB Welbourn: The History of Endocrine Surgery. Greenwood Publishing Group, 1990, ISBN 0-275-92586-2 , p. 36.
- ↑ TO EPITOME OF CURRENT MEDICAL LITERATURE. In: Br Med J. 1914 June 20; 1 (2790), pp. E97-E100.
- ↑ Patent specification of the United States Patent Office 3,414,383 pdf
- ↑ E. Werner among others: Encyclopedia Medical History. Walter de Gruyter, 2004, ISBN 3-11-015714-4 , p. 407.
- ↑ Th. Kocher: About goiter extirpation and its consequences. In: Arch Klin Chir. Volume 29, 1883, p. 2541.
- ↑ Julius Wagner-Jauregg on the website of the Institute for the History of Medicine at the University of Vienna ( Memento from June 28, 2009 in the Internet Archive )
- ↑ E. Werner among others: Encyclopedia Medical History. Walter de Gruyter, 2004, ISBN 3-11-015714-4 , p. 1463.
- ↑ Jürg Rageth: Cretinism. In: Historical Lexicon of Switzerland . November 4, 2008 , accessed June 5, 2019 .
- ↑ A. Gottschalk: Thyroid. In: Frank Wappler, Hartmut Bürkle, Peter Tonner (eds.): Anesthesia and accompanying diseases. Georg Thieme Verlag, 2011, ISBN 978-3-13-159522-5 , p. 219. Restricted preview in the Google book search
- ↑ K. Miehle, R. Paschke: Are TSH receptor polymorphisms a possible cause for the interindividually different normal ranges of TSH, fT3 and fT4 values in a normal population? ( Memento from June 10, 2008 in the Internet Archive ) In: Universität Leipzig, Research Report 2004.
- ↑ Saarland University Hospital: Thyroid diseases in childhood; last viewed on Feb. 12, 2008
- ↑ K. Middendorf: Obstetrics Basics. Springer, Berlin / Heidelberg 2006, pp. 79–82.
- ↑ a b A. Grüter-Kieslich: Congenital hypothyroidism and goiter. In: Differential Diagnosis of Pediatrics. Elsevier, 2004, ISBN 3-437-22530-8 .
- ↑ Guideline-based thyroid therapy. In: Journal Med. Of April 7, 2002.
- ↑ a b Hypothyroidism: Symptoms and Treatment . In: Hypothyroidism Symptoms: Children . Retrieved on February 20, 2018: "Choking attacks, disturbed muscle development"
- ↑ Helmut Madjar, Ellen B. Mendelson: Practice of Breast Ultrasound: Techniques, Findings, Differential Diagnosis. Thieme, 2011, ISBN 978-1-60406-088-1 , p. 97.
- ↑ N. Udayakumar, AC Rameshkumar, AV Srinivasan: Hoffmann syndrome: presentation in hypothyroidism. In: Journal of postgraduate medicine. Volume 51, Number 4, 2005 Oct-Dec, pp. 332-333, ISSN 0022-3859 . PMID 16388183 .
- ↑ O. Okosieme, J. Gilbert, P. Abraham, K. Boelaert, C. Dayan, M. Gurnell, G. Leese, C. McCabe, P. Perros, V. Smith, G. Williams, M. Vanderpump: Management of primary hypothyroidism: statement by the British Thyroid Association Executive Committee. In: Clinical endocrinology. [electronic publication before printing] May 2015, doi: 10.1111 / cen.12824 , PMID 26010808 , (Review), PDF ( memento of March 25, 2016 in the Internet Archive ) (accessed on March 21, 2016).
- ↑ JR Garber, RH Cobin, H. Gharib, JV Hennessey, I. Klein, JI Mechanick, R. Pessah-Pollack, PA Singer, KA Woeber: Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. In: Thyroid: official journal of the American Thyroid Association. Volume 22, number 12, December 2012, pp. 1200–1235, doi: 10.1089 / thy.2012.0205 , PMID 22954017 , (free full text).
- ^ Association of Clinical Biochemistry, British Thyroid Association and British Thyroid Foundation: UK guidelines for the use of thyroid function tests (2006) , PDF ( Memento of November 17, 2013 in the Internet Archive ) (accessed on March 21, 2016).
- ↑ Embryotox - drug safety during pregnancy and lactation ( Memento of March 30, 2018 in the Internet Archive )
- ↑ a b J. Schübelweiher, J. Feldkamp, A. Bergmann, W. Drossard, K. Voigt: latent Hypothyroidism in Adults. In: Deutsches Arzteblatt international. Volume 114, number 25, June 2017, pp. 430–438, doi: 10.3238 / arztebl.2017.0430 , PMID 28683860 (review) ( free full text in German: PDF ).
- ^ A b C. Baumgartner, MR Blum, N. Rodondi: Subclinical hypothyroidism: summary of evidence in 2014. In: Swiss medical weekly. Volume 144, 2014, p. W14058, doi: 10.4414 / smw.2014.14058 , PMID 25536449 (review) (free full text).
- ↑ MI Surks, JG Hollowell: Age-specific distribution of serum thyrotropin and antithyroid antibodies in the US population: implications for the prevalence of subclinical hypothyroidism. In: The Journal of clinical endocrinology and metabolism. Volume 92, number 12, December 2007, pp. 4575-4582, doi: 10.1210 / jc.2007-1499 , PMID 17911171 (free full text).
- ↑ N. Aggarwal, S. Razvi: Thyroid and aging or the aging thyroid? An evidence-based analysis of the literature. In: Journal of thyroid research. Volume 2013, 2013, p. 481287, doi: 10.1155 / 2013/481287 , PMID 24106641 , PMC 3782841 (free full text) (review).
- ↑ JV Hennessey, R. Espaillat: Diagnosis and Management of Subclinical Hypothyroidism in Elderly Adults: A Review of the Literature. In: Journal of the American Geriatrics Society. Volume 63, number 8, August 2015, pp. 1663–1673, doi: 10.1111 / jgs.13532 , PMID 26200184 (review) ( free full text: PDF ).
- ↑ Matthias Schott, Jochen Seißler, Werner A. Scherbaum: Diagnostik bei autoimmune thyroid diseases / Diagnostic testing for autoimmune thyroid diseases. In: LaboratoriumsMedizin. 30, 2006, p. 254, doi: 10.1515 / JLM.2006.033 .
- ↑ Karin Götsch: General and special disease theory, Georg Thieme Verlag, 2007, ISBN 978-3-13-152211-5 , p. 164. Restricted preview in the Google book search
- ↑ Z. Javed, T. Sathyapalan: Levothyroxine treatment of mild subclinical hypothyroidism: a review of potential risks and benefits. In: Therapeutic advances in endocrinology and metabolism. Volume 7, number 1, February 2016, pp. 12-23, doi: 10.1177 / 2042018815616543 , PMID 26885359 , PMC 4740939 (free full text) (review).
- ↑ O. Okosieme, J. Gilbert, P. Abraham, K. Boelaert, C. Dayan, M. Gurnell, G. Leese, C. McCabe, P. Perros, V. Smith, G. Williams, M. Vanderpump: Management of primary hypothyroidism: statement by the British Thyroid Association Executive Committee. In: Clinical endocrinology. [electronic publication before printing] May 2015, doi: 10.1111 / cen.12824 , PMID 26010808 , (Review), PDF ( memento of March 25, 2016 in the Internet Archive ) (accessed on March 21, 2016).
- ↑ W. Hecker: Endocrinology. In: Clinic Guide Pediatrics. Jungjohann Verlag, Stuttgart, ISBN 3-8243-1214-X .
- ^ PN Taylor, A. Iqbal, C. Minassian, A. Sayers, MS Draman, R. Greenwood, W. Hamilton, O. Okosieme, V. Panicker, SL Thomas, C. Dayan: Falling threshold for treatment of borderline elevated thyrotropin Levels-balancing benefits and risks: evidence from a large community-based study. In: JAMA internal medicine. Volume 174, number 1, January 2014, pp. 32-39, doi: 10.1001 / jamainternmed.2013.11312 , PMID 24100714 (free full text).
- ↑ LF Michaelsson, BB Medici, JL la Cour, C. Selmer, M. Røder, H. Perrild, N. Knudsen, J. Faber, B. Nygaard: Treating Hypothyroidism with Thyroxine / Triiodothyronine Combination Therapy in Denmark: Following Guidelines or Following Trends? In: European thyroid journal. Volume 4, number 3, September 2015, pp. 174–180, doi: 10.1159 / 000437262 , PMID 26558234 , PMC 4637515 (free full text).
- ↑ DEGAM guideline No. 18: Increased TSH value in the family doctor's practice , 2016, PDF , p. 9f.
- ^ Health lexicon of the Association of Internists ( Memento from May 10, 2008 in the Internet Archive )
- ^ R. Hörmann: Thyroid Diseases: Guide for Practice and Clinic. 4th edition. 2005, p. 160.
- ^ W. Zhao, C. Han, X. Shi, C. Xiong, J. Sun, Z. Shan, W. Teng: Prevalence of goiter and thyroid nodules before and after implementation of the universal salt iodization program in mainland China from 1985 to 2014: a systematic review and meta-analysis. In: PloS one. Volume 9, number 10, 2014, p. E109549, doi: 10.1371 / journal.pone.0109549 , PMID 25313993 , PMC 4196906 (free full text) (review).
- ^ X. Sun, Z. Shan, W. Teng: Effects of increased iodine intake on thyroid disorders. In: Endocrinology and metabolism (Seoul, Korea). Volume 29, number 3, September 2014, pp. 240-247, doi: 10.3803 / EnM.2014.29.3.240 , PMID 25309781 , PMC 4192807 (free full text) (review).
- ↑ A. Prete, RM Paragliola, SM Corsello: Iodine supplementation: Usage "with a Grain of Salt". In: International journal of endocrinology. Volume 2015, 2015, p. 312305, doi: 10.1155 / 2015/312305 , PMID 25873950 , PMC 4383497 (free full text) (review).
- ↑ Claudia Reusch: Hypothyroidism. In: Peter F. Suter, Hans G. Nobody (Hrsg.): Internship at the dog clinic. 10th edition. Paul-Parey-Verlag, 2006, ISBN 3-8304-4141-X , pp. 922-925.
- ↑ Ulbrich, Hoffmann, Drochner: Feeding and animal health . Eugen Ulmer Verlag Stuttgart 2004.
- ↑ K. Gabrisch, P. Zwart: Diseases of the domestic animals. 6th edition. Schlütersche Verlagsgesellschaft, Hanover 2005, ISBN 3-89993-010-X .