Congenital hypothyroidism
| Classification according to ICD-10 | |
|---|---|
| E03.0 | Congenital hypothyroidism with diffuse goiter |
| E03.1 | Congenital hypothyroidism without goiter |
| ICD-10 online (WHO version 2019) | |
The congenital ( congenital , also Connatal ) Hypothyroidism is a special form of hypothyroidism . It relates to the patient in a development phase, is particularly sensitive in its entire nervous system and by the lack of thyroid hormones can be permanently damaged. If the disorder is not recognized and treated immediately after birth, it leads to the full picture of cretinism .
frequency
The screening report of the German Society for Newborn Screening (DGNS) shows a total prevalence of 1: 3270 newborns for 2004 (prevalence 2013: 1: 3233). The frequency within the individual screening centers fluctuates between 1: 2143 and 1: 5239. These numbers are roughly the same as those reported for North America, where an incidence of approximately 1: 3000 to 1: 4000 newborns is reported with a slightly higher incidence among Hispanic and lower rates among African American children. This means that congenital hypothyroidism is roughly twice as common as phenylketonuria , the first congenital metabolic disease for which screening was introduced. Girls are affected about twice as often as boys.
Congenital hypothyroidism can be an essential characteristic in the context of rare syndromes , such as the brain-lung-thyroid syndrome .
causes
Depending on the cause, a distinction can be made between:
-
Disturbed organ development
- In most cases, the underactive thyroid is caused by a disruption in its organ development during embryonic development ( agenesis or dysgenesis). This results in no or insufficiently functional thyroid tissue. The reason for these deficiencies is not known. Mutations in genes that play a role in thyroid development could only be detected in rare individual cases , including in the FOXE1 gene, which codes for thyroid transcription factor 2 (TTF-2), and in the PAX8 gene, which is paired - Box protein 8 (PAX-8).
-
Impaired thyroid function
- In addition, there are disorders of hormone formation in an otherwise normally established thyroid gland. Inborn errors of thyroxine synthesis follow an autosomal - recessive inheritance , defects in the receptor for thyroid hormone are autosomal dominant inherited. Overall, around 85% of all congenital hypothyroidism occurs sporadically, the remaining 15% are hereditary.
-
Transient hypothyroidism
- Less often, the underfunction is of a temporary nature. This is the case when it is caused by the transfer of maternal drugs or blocking antibodies to the child via the placenta, by iodine deficiency or excessive iodine exposure.
-
Central hypothyroidism
- Disorders of the hypothalamus - pituitary axis - so-called central, secondary or tertiary sub-functions - with reduced production of thyroid stimulating hormone (TSH) or thyrotropin releasing hormone (TRH) are extremely rare, for example, when IGSF1 deficiency syndrome , but missed the usual screening tests.
Clinical manifestations
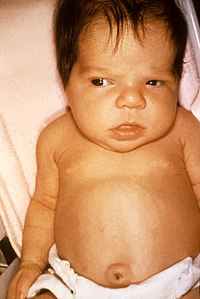
Although the thyroid hormone is extremely important for the development of almost all organ systems, most children are initially normal at birth. Maternal thyroid hormone, which is transmitted through the placenta , protects even those fetuses that are completely lacking thyroid gland, at least partially. The concentration of thyroxine (T 4 ) in the umbilical cord blood of these children is about one third to one half of that of healthy children. The 5% most severely affected children can be noticed early on with large fontanelles , wide gaping skull sutures , large tongue, distended abdominal wall and umbilical hernia. With increasing breakdown of maternal thyroxine, further symptoms appear. The infants drink poorly, become constipated, listless, and sleep a lot. They often need to be woken up at mealtimes. The voice can be rough and hoarse, the skin feels cool, the tension in the muscles is slack (hypotension) and the reflexes are weak. A neonatal jaundice (icterus neonatorum) which may be extended (icterus prolongatus) due to the delayed maturation of the liver. An enlargement of the thyroid gland (goiter, goiter ) is found in about 5–10% of children, mostly with congenital disorders of thyroxine synthesis.
If the disease is not recognized and treated, there is a delay in growth from the second to third month of life. The decrease in intelligence also increases the later the treatment begins. If it begins in the first three months, the mean IQ is 89 (range 64–107), if it begins between the fourth and sixth months of life it is 71 (range 35–96) and does not begin until after the first half year of life at 54 (range 25-80). Other long-term effects are disorders in the gross and fine motor coordination, balance disorders ( ataxias ), muscle weakness and spasticity , speech disorders, attention disorders and strabismus.
Investigation methods
Since an early diagnosis is so enormously important for the normal development of children as possible, the diagnosis is made in most developed countries via a serial examination in the newborn age (newborn screening). In Germany, the content of thyrotropin (TSH), which increases significantly in the absence of thyroid hormone production, is determined in so-called dry blood. However, the rare cases of central, secondary or tertiary hypothyroidism are overlooked. In the United States of America, most screening programs first measure the T 4 concentration and only also measure thyrotropin for values below the tenth percentile . Sampling should be done on the third day of life. If the newborn is discharged or relocated beforehand, it can also take place earlier, but then usually has to be repeated. In the positive case, a confirmation test with a determination of thyrotropin, free T 4 and free T 3 must then be carried out immediately . If the findings of an underactive thyroid are confirmed, further examinations can be carried out to clarify the cause. In addition to the determination of thyroglobulin for the detection of thyroid tissue and a hormone production disorder, this includes imaging measures such as sonography or thyroid scintigraphy . However, since the results of these examinations have no influence on the treatment, they are not absolutely necessary. If there is evidence of maternal thyroid disease, testing for thyroid autoantibodies in mother and child can reveal those forms that are likely to be temporary. If there is a suspicion of an iodine excess or deficiency as the cause of hypothyroidism, this can be confirmed by determining the iodine excretion with the urine .
treatment
Because of the irreversible damage to the nervous system, congenital hypothyroidism must be treated as early as possible. It must not be delayed unnecessarily by waiting for the results of the examination and should be carried out immediately after the blood sample has been taken for confirmatory diagnostics if the screening results are positive. The aim of the treatment is to normalize the T 4 content as quickly as possible with a subsequent normalization of the TSH content in the blood. For this purpose, the hormone deficit is compensated for by giving levothyroxine in a relatively high initial dose. After two weeks, the dose can be reduced depending on the results of a check of the values for TSH and T 4 in the blood. According to the growth of the child, it must be adapted to the increased needs in further life. If there are doubts about the diagnosis of permanent hypothyroidism, an attempt at elimination can be made after the first birthday at the earliest, according to American sources it is better not until after the third birthday. Otherwise, the substitution must be lifelong. If iodine deficiency is proven to be the cause of the underactive thyroid, this is treated with iodine substitution.
Prospect of healing
Depending on when the diagnosis was made, the prognosis for the affected children is very good. If the underfunction is recognized and consistently treated within the first two weeks of life, there are only minor differences in the level of intelligence, school performance and neurophysiological tests compared to healthy classmates or siblings in adulthood. However, if treatment does not start until later, physical development can still normalize, but intelligence remains limited.
Individual evidence
- ↑ Screening report 2004 of the German Society for Newborn Screening ( Memento from September 2, 2007 in the Internet Archive )
- ↑ a b c d e f American Academy of Pediatrics, American Thyroid Association, Lawson Wilkins Pediatric Endocrine Society: Update of Newborn Screening an Therapy for Congenital Hypthyroidism. In: Pediatrics. 2006, 117, pp. 2290-2303.
- ↑ a b c d e f g h C. I. Kaye and the Committee on Genetics: Newborn Screening Fact Sheet. In: Pediatrics. 2006; 118, pp. E934-e963, PMID 16950973 .
- ↑ a b Guideline of the GNPI ( Memento of February 24, 2008 in the Internet Archive )