Meningococci
| Meningococci | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Neisseria meningitidis |
||||||||||||
| Systematics | ||||||||||||
|
||||||||||||
| Scientific name | ||||||||||||
| Neisseria meningitidis | ||||||||||||
| ( Albrecht & Ghon 1901) Murray 1929 |
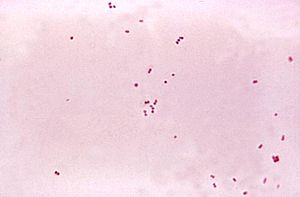
Meningococci ( Neisseria meningitidis , formerly Meningococcus meningitis ) are gram-negative intracellular bacteria that occur as diplococci . They colonize the nasopharynx in humans and can cause serious diseases. Around ten percent of the European population carry these bacteria in the nasopharynx without developing any signs of disease.
features
Meningococci are bacteria of the species Neisseria meningitidis , which belongs to the aerobically and facultatively anaerobically growing, Gram-negative cocci. The bacteria can adjust their sugar metabolism to the anaerobic conditions in the infected tissue through the upregulation of nitrate-dependent instead of oxygen-dependent enzymes. In liquid nutrient media (as well as in the cerebral and spinal fluid) the bacteria accumulate in pairs with the longitudinal axes of the two bacteria lying next to each other. The ends of the bacteria are rounded, so that a single bacterium resembles a coffee bean, and a pair resembles a bread roll (hence the description as a bun-shaped gram-negative diplococcus). In meningitis caused by these bacteria, numerous white blood cells ( granulocytes ) are almost always found in the cerebrospinal fluid ( liquor cerebrospinalis ).
Meningococci grow in the laboratory on rich nutrient media such as B. cooking blood agar or Columbia blood agar and, due to their resistance to colistin, also on special culture media for growing pathogenic Neisseria species such. B. Thayer-Martin agar . The culture works best in an atmosphere that has an increased carbon dioxide content (approx. 5%). The colonies after 24 hours of growth, small (about 1 mm diameter), smooth, round and of greyish color. They form cytochrome c oxidase and therefore react positively in the oxidase test .
13 different serogroups are known within the species Neisseria meningitidis (A, B, C, D, 29E, H, I, K, L, W-135, X, Y and Z). In sick people, only serogroups A (especially in the African "meningitis belt"), B, C, W-135, Y and rarely X (also mainly in Africa) are detected. In meningococcal infections in Germany, serogroup B is most frequently detected, followed by C. The serogroups differ due to their surface structure, which among other things consists of special sugar molecules . These and other molecules form a thick capsule around the bacteria, which protects them from the attacks of the immune system .
Transmission routes
Meningococci are transmitted from person to person through droplet infection, for example when coughing , sneezing or kissing . With the help of small appendages (pili), they attach themselves to the mucous membranes of the nasopharynx, where they can remain for weeks or months. Especially when the immune system is weakened, for example by other infections , the bacteria multiply, penetrate the mucous membranes and cause meningitis and blood poisoning .
Meningococcal infections
| Classification according to ICD-10 | |
|---|---|
| A39 | Meningococcal infection |
| ICD-10 online (WHO version 2019) | |
More than 90 percent of meningococcal infections worldwide are caused by certain serotypes , types A, B, C, W135 and Y. In Germany fall ill each year about 700 to 800 people at a meningococcal meningitis (also called cerebrospinal meningitis epidemic and communicable stiff neck ), to about 70 percent by the serotype B is caused. Some cases are brought in by travelers from other European countries. 40 percent of all patients are children under four years of age, by far the most common babies are in their first year of life. Around ten percent of patients still die today.
From December to June, meningococcal epidemics occur increasingly in the African "meningitis belt" (south of the Sahara from Sudan to Gambia ). From November to May they also occur more frequently in India, especially northern India, and Nepal . In principle, any country with poor hygiene conditions can be viewed as a possible area of meningitis. Diseases of group A or C are generally seen here.
Since 2012 at the latest, the group of men who have sex with men has been found to have an increased risk of infection in metropolises such as New York and Berlin .
Clinical picture (symptoms)
The incubation time is usually 3-4 days on average, shorter and longer incubation times (2-10 days) are also observed.
The spectrum of the disease ranges from mild courses with spontaneous healing to a highly acute outbreak which, despite treatment, leads to death within a few hours. The Meningitis begins with severe malaise such as fatigue, high fever , vomiting, chills , joint and muscle pain, cramps or consciousness disturbances . Neck stiffness occurs as a typical sign of meningitis ; this then causes the so-called pillow drilling : when the patient lies down, an overstretched hollow back appears and the head presses into the pillow ( opisthotonus ). About half of the patients have petechiae .
In the case of infants, in addition to the almost always occurring fever, the symptoms may initially be ambiguous: apathy or restlessness, refusal to eat and sensitivity to touch. Sensitivity to light is a possible accompanying symptom.
Clouding of consciousness, punctiform skin bleeding and circulatory collapse are indications of a life-threatening course of the disease ( Waterhouse-Friderichsen syndrome ). In severe cases, death occurs within a few hours. If the bacteria enter the bloodstream and flood the body with their toxins, the doctor speaks of sepsis . It is life threatening. With rapid progression to sepsis, the "meningitic" symptoms do not have to occur; the shock and toxicity-related symptoms are then in the foreground. If treatment is not taken promptly, sepsis can lead to loss of limbs.
Treatment with antibiotics as early as possible is crucial . Despite treatment, complications and long-term effects such as hearing loss, blindness , paralysis or convulsions can occur and any help comes too late for every tenth patient. This is why preventive vaccination is particularly important for people at risk.
Close contacts should receive preventive therapy with an antibiotic (such as rifampicin ).
therapy
If meningococci have been detected as the pathogen, the antibiotic of choice is penicillin G or a cephalosporin of the 3a generation ( ceftriaxone ). The advantage of ceftriaxone is that it can detect other bacterial meningitis pathogens . Early therapy is important. It is therefore customary in practice to administer 3rd generation cephalosporins immediately if purulent meningitis is suspected, even before the pathogen is detected; In addition, the administration of ampicillin should be considered in order to cover Listeria meningitis with antibiotics.
Chemoprophylaxis
To prevent meningococcal meningitis, chemoprophylaxis is carried out by eradicating the pathogens (especially from the nasopharynx) as quickly as possible (but within ten days) in close contact persons, the last seven days of infected people. Chemotherapeutic agents that can be used here are rifampicin and its alternatives ciprofloxacin or ceftriaxone. If the patient had not received a third-generation cephalosporin intravenously for treatment, the patient should also receive prophylaxis with rifampicin after completing his therapy.
Vaccination (immunoprophylaxis)
Vaccinations against meningococci are indicated for people with immunodeficiencies, with asplenia , at risk laboratory personnel and travelers to epidemic areas. For prevention, for example before a planned spleen removal , vaccines are available for meningococcal vaccination against serotype C, which occurs frequently in England, Spain or some regions of Germany, and against types A, Y and W135. So far, a total of four vaccines are available in Germany, which essentially contain purified fragments ( polysaccharides or oligosaccharides ) of the bacterium Neisseria meningitidis .
A recombinant adsorbate vaccine ( Bexsero , GlaxoSmithKline ) effective against serotype B , which can be used from the age of 2 months, was approved by the EU Commission in January 2013. A vaccine against type B meningococci was used in Cuba as early as 1988.
Polysaccharide Vaccines
The two available polysaccharide vaccines (abbreviation: PS ) provide protection against serotypes A and C ( AC vaccine , such as meningococcal vaccine A + C Mérieux ) or against serotypes A, C, W135 and Y ( ACWY- Vaccine , such as Mencevax ACWY ). Both protect best from the age of two, as T-cell-independent B-cell activation is only possible from this age.
Polysaccharide vaccines are injected under the skin. The vaccination protection lasts for at least three years. A single injection is sufficient for adults and children. The AC vaccine can be used from 18 months of age. The ACWY vaccine is effective from two years of age. For younger children, protection against groups C, W 135 and Y is not guaranteed and vaccination protection lasts for a maximum of two years. In order to achieve better vaccination protection, children under two years of age can also be vaccinated a second time every three months. The protective effect of the vaccination sets in after about two weeks. If there is a risk of infection, a revaccination is advisable after three years .
Conjugate vaccines
C-conjugate vaccines have been specially developed for children between the ages of two months and two years . If necessary, they can also be used with older children, adolescents or adults. They protect against infections of the meningococcal type C, which causes about every fifth disease in Germany. In a conjugate vaccine , the parts of the bacterial envelope, in addition to a protein ( protein bound), thereby achieving a better immune response. Vaccination with the conjugate vaccine ( e.g. Meningitec , Menjugae or NeisVac-C ) can be supplemented with a polysaccharide vaccine from the age of three if necessary.
A tetravalent conjugate vaccine against A, C, W135 and Y has been available in Europe since October 2010, which can not only be used earlier than the corresponding polysaccharide vaccine, but can also be refreshed because - unlike polysaccharide vaccines - an immunological memory is formed here. In addition, the T-cell aid allows a class change so that IgA can also be formed (polysaccharide vaccines only IgM) and thus the carrier status should be reduced.
The meningococcal vaccination can usually be done at the same time as other vaccinations. Time intervals to other vaccinations are not to be observed.
A vaccine (Bexsero®) against serotype B has been approved in Europe since January 2013. This is not based on capsule antigens as in serotypes A, C, W135 and Y, since the capsule of serotype B is similar to a human protein, but on four surface antigens.
Vaccination recommendations
The Standing Vaccination Commission (STIKO) recommends vaccination against meningococci of serogroup C with the C-conjugate vaccine as standard for all children from 12 months. The reduction of the morbidity of invasive meningococcal diseases caused by this serogroup and the resulting consequences such as hospitalization, severe complications, disability and death are seen as the primary goal. For children and adolescents who have not yet been vaccinated, it is recommended that they have the vaccination up to the age of 18.
Vaccination is also recommended for all people with an increased risk of infection, for example if there is an increased risk at work or individually, or as a travel vaccination. People with immunodeficiencies or a missing or non-functional spleen , for example, are particularly at risk . Travelers to areas where meningococcal infections occur frequently are also at an increased risk of infection if they stay there for a longer period or if they are in close contact with the population. A vaccination schedule with one of the polysaccharide vaccines, the conjugate vaccine, or both, is used as required.
Since July 2013 , the Berlin Vaccination Council has recommended men who have sex with men (MSM) to be vaccinated with a vaccine that contains a component against group C meningococci and is approved for adults. The reason for the vaccination recommendation are the frequent outbreaks of disease in the MSM group with severe, even fatal courses, as recently described in New York and Paris.
Saudi Arabia calls during the Mecca - pilgrimages of pilgrims must not have been and visitors a vaccination, the maximum of three years and a minimum of ten days before the arrival in Saudi Arabia issued. The quadruple vaccine A, C, W135, Y is mandatory . Pilgrims arriving from endemic areas are examined and observed if meningitis is suspected. All other travelers do not need to be vaccinated.
Protection is only built up against the serogroups mentioned in each case . Vaccination against the meningitis caused by meningococci of group B, which occurs more frequently in Central Europe and Brazil, is currently not generally recommended by the Standing Vaccination Commission, as the available study data are not yet sufficient. The STIKO points out, however, that a vaccination "can be useful for people with an increased risk of disease after weighing up the individual benefit-risk".
Reporting requirement
In Germany, meningococcal meningitis is a reportable disease according to Section 6, Paragraph 1, Number 1 of the Infection Protection Act (IfSG). You are required to report by name in the event of suspicion, illness or death. The diagnosing doctors, etc., are obliged to report the illness ( Section 8 IfSG). In addition, the direct evidence of Neisseria meningitidis is notifiable by name according to § 7 IfSG. The reporting requirement only applies to direct evidence from CSF, blood, hemorrhagic skin infiltrates or other normally sterile substrates. The laboratories etc. are obliged to report with regard to the detection of the pathogen (§ 8 IfSG).
In Switzerland, the positive laboratory analysis of Neisseria meningitidis must be reported to laboratories in accordance with the Epidemics Act (EpG) in conjunction with the Epidemics Ordinance and Annex 3 of the EDI Ordinance on the reporting of observations of communicable diseases in humans . In addition, an invasive meningococcal disease is notifiable for doctors, hospitals, etc. The standards and Appendix 1 of the above-mentioned EDI ordinance are the basis for this. Reporting criteria are clinical suspicion and the need for pathogen-specific laboratory diagnostics.
literature
- Ulrich Vogel, Matthias Frosch: Gram-negative aerobic and facultative anaerobic cocci. In: Birgid Neumeister, Heinrich K. Geiss, Rüdiger W. Braun, Peter Kimmig (eds.): Microbiological diagnostics . Georg Thieme Verlag, Stuttgart / New York 2009, ISBN 978-3-13-743602-7 , pp. 419-425.
- Marianne Abele-Horn: Antimicrobial Therapy. Decision support for the treatment and prophylaxis of infectious diseases. With the collaboration of Werner Heinz, Hartwig Klinker, Johann Schurz and August Stich, 2nd, revised and expanded edition. Peter Wiehl, Marburg 2009, ISBN 978-3-927219-14-4 , p. 320 f. and 327-329.
- Karl Wurm, AM Walter: Infectious Diseases. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition, ibid. 1961, pp. 9-223, here: pp. 177-184.
Web links
- Meningococcal Diseases - Information from the Robert Koch Institute
- Meningococci, invasive diseases (Neisseria meningitidis). In: RKI-Ratgeber. Robert Koch Institute, February 1, 2014, accessed on March 27, 2020 .
- www.meningococcus.de - National Reference Center for Meningococci, Institute for Hygiene and Microbiology, University of Würzburg
- EpiscanGIS - Web-based geographic information system for monitoring meningococcal cases in Germany
- Meningococcal Network - Comparative genome analysis for recording, evaluating and preventing meningococcal diseases
Individual evidence
- ↑ E. Bartolini, E. Frigimelica, S. Giovinazzi, G. Galli, Y. Shaik, C. Genco, JA Welsch, DM Granoff, G. Grandi, R. Grifantini: Role of FNR and FNR-regulated, sugar fermentation genes in Neisseria meningitidis infection. In: Molecular Microbiology. (2006); 60, pp. 963-972. doi: 10.1111 / j.1365-2958.2006.05163.x
- ↑ Karl Wurm, AM Walter: Infectious Diseases. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. 1961, p. 177.
- ↑ a b Berlin recommends vaccination for gay men . Zeit Online , July 20, 2013.
- ^ Joanna Wane: The case for vaccination . Retrieved July 3, 2015.
- ↑ No taxi, no phone call, no help. In: taz.de
- ↑ These include household members, people who have had contact with the patient's secretions from the oropharynx, intimate partners, close friends and people sitting next to them at school.
- ↑ Marianne Abele-Horn (2009), p. 320 f.
- ↑ Marianne Abele-Horn (2009), p. 328.
- ↑ Bexsero, on the website of the European Medicines Agency .
- ↑ Bioboom in the Caribbean . In: Der Spiegel . No. 27 , 1999 ( online ).
- ↑ 50 Years of the Vaccination Program in Cuba - A Revolution in Health. ( Memento of November 10, 2011 in the Internet Archive ) In: Digital Granma International. March 3, 2011; Retrieved April 26, 2011.
- ↑ menveo.com
- ↑ a b Standing Vaccination Commission (STIKO) at the RKI: Statement on the new meningococcal B vaccine. In: Epidemiological Bulletin 49/2013. Robert Koch Institute, December 9, 2013, pp. 495–498 , accessed on May 17, 2014 .
- ↑ a b c Epidemiological Bulletin 2012, No. 30 (July 30, 2012) (PDF)
- ↑ Recommendation of the Berlin Vaccination Board for vaccination against meningococcal diseases . Berlin Senate Department for Health and Social Affairs, press release from July 18, 2013.
- ↑ Circular on the publicly recommended meningococcal vaccination (PDF) Berlin Senate Department for Health and Social Affairs, December 7, 2014.
