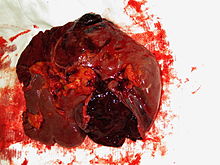
Splenectomy
The medical term splenectomy (also known as spleen extirpation ) describes the surgical removal of the spleen , which leads to asplenia . The most common reason for performing this procedure is injury to the spleen , for example from blunt abdominal trauma . Other reasons for removing the spleen are internal diseases that either involve a threatening dysfunction of the spleen or result in a severe enlargement of the spleen ( splenomegaly ) with the risk of a tear without an accident ("spontaneous rupture").
indication
The splenectomy is often necessary as an emergency procedure in the case of severe injuries to the spleen, if an organ-preserving surgical procedure is not possible or does not appear sensible due to external circumstances. A spontaneous rupture of the spleen due to the conditions listed below may also require an emergency splenectomy.
An indication for elective (i.e. not emergency) splenectomy can arise in the following clinical pictures:
- Hereditary spherocytosis
- Hereditary elliptocytosis
- Autoimmune hemolytic anemia
- Thalassemia requiring transfusion
- Sickle cell anemia requiring transfusion
- Werlhof's disease (if conservative measures fail)
- Thrombotic thrombocytopenic purpura ("Moschcowitz syndrome")
- Myelofibrosis - for splenic infarction , bleeding, high transfusion requirements, symptomatic splenomegaly
execution
In unclear emergency situations, access to the abdominal cavity is via a generous, median longitudinal incision, or alternatively via a cross-section above the navel. After the spleen has been properly identified as the source of bleeding, the longitudinal section can be extended transversely to the left and the cross section upwards. The source of the bleeding is identified as quickly as possible and the bleeding is stopped by local compression as far as possible. The more detailed inspection of the spleen determines the further procedure: If there is good accessibility, all possibilities are used to stop the bleeding without removing the spleen. If this does not succeed, the splenic hilum, i.e. the transition of the blood vessels from the area of the tail of the pancreas to the spleen, is manually moved under and placed between clamps.
The scheduled splenectomy is usually performed through an incision on the left side of the costal arch. As a rule, the splenic hilum can now be displayed precisely without disturbing bleeding; the individual blood vessels are first tied off and then severed. In addition, the splenectomy is also performed laparoscopically using a minimally invasive technique .
Complications
The most common complications after splenectomy concern the respiratory system : Pneumonia , atelectasis and pleural effusions are not uncommon . Pancreatic fistulas due to insufficiently recognized lesions of the pancreatic tail occur in about 1% of cases. Thromboembolic complications are also more common after splenectomy. The reason is the lack of breakdown of the blood platelets and the resulting thrombocytosis .
Long-term consequences
Although the spleen is not a primarily vital organ, its removal can have serious long-term consequences.
Infections
After a splenectomy, there is a lifelong increased risk of haematogenic bacterial and fungal infections. In particular, haematogenic infections with encapsulated bacteria, primarily pneumococci , Haemophilus influenzae and meningococci , can lead to a life-threatening septic post-splenectomy syndrome within a few hours , which occurs in 1–5% of patients after a splenectomy. Any fever and any severe fever-free illness can be a sign of the onset of a life-threatening infection. An empirical antibiotic therapy should then be started immediately, for example with intravenous or intramuscular ceftriaxone with or without vancomycin . Alternatively, after the splenectomy, the patient can be prescribed an oral antibiotic prophylactically, which he takes directly in the event of a febrile episode or severe illness, such as amoxicillin 2 g or levofloxacin 750 mg. Patients must be trained accordingly.
In addition, long-term antibiotic prophylaxis is recommended for children under five years of age , for older children and adults in the first two years after splenectomy, e. B. with an oral penicillin twice a day.
Vaccinations against Streptococcus pneumoniae , Haemophilus influenzae and meningococci as well as an annual flu vaccination are recommended. In the case of an elective splenectomy, vaccinations should start before the planned procedure.
Thrombosis
The lack of a filter function of the spleen can lead to a considerable increase in the number of blood platelets ( thrombocytosis ). This can lead to blood clots which can block the portal vein in particular . An average of 2–5% of patients without a spleen suffer from such a life-threatening thrombosis. Patients with rapidly increasing platelet counts are most at risk in the first two years after loss of the spleen. For the prevention of thrombosis can anticoagulant ( anti-coagulation ) are administered, the effectiveness of this prevention is not scientifically proven. As a complication of anticoagulant therapy, increased bleeding can occur, which must be taken into account when weighing up the risks and benefits. In most cases, low molecular weight heparins are used in a preventive dose for anticoagulation in the first few weeks or months , followed by acetylsalicylic acid .
Individual evidence
- ↑ C. Jurowich, M. Pauthner, C. Gebhardt: Perioperative Management in Visceral and Thoracic Surgery . Deutscher Ärzte Verlag, Cologne 2004, ISBN 3-7691-0405-6 .
- ^ JR Siewert: Surgery . 7th edition. Springer, Berlin / Heidelberg 2010, ISBN 3-540-30450-9 , 37 Milz , p. 760 ff .
- ^ Lorry G. Rubin, William Schaffner: Care of the Asplenic Patient . In: New England Journal of Medicine , 2014, Volume 371, Issue 4, July 24, 2014, pp. 349-356, doi: 10.1056 / NEJMcp1314291
- ↑ [1] RKI vaccination recommendation
- ↑ Konstantinos M. Stamou: Prospective Study of the Incidence and Risk Factors of Postsplenectomy Thrombosis of the Portal, Mesenteric, and Splenic Veins . In: Archives of Surgery . tape 141 , no. 7 , July 1, 2006, p. 663 , doi : 10.1001 / archsurg.141.7.663 ( archsurg.jamanetwork.com ).
- ↑ M. Engelhardt, P. Haas, C. Theilacker, S. Eber, M. Schmugge, W. Kern, H. Heimpel: Prevention of infections and thromboses after splenectomy or loss of function of the spleen . In: German Medical Weekly . tape 134 , no. 17 , April 2009, p. 897-902 , doi : 10.1055 / s-0029-1220231 .