Cerebral hemorrhage
| Classification according to ICD-10 | |
|---|---|
| I60.- | Subarachnoid hemorrhage |
| I61.- | Intracerebral haemorrhage |
| I62.- | Other non-traumatic intracranial bleeding |
| I62.0- | Subdural bleeding (nontraumatic) |
| I62.1 | Non-traumatic extradural bleeding Non-traumatic epidural bleeding |
| S06.2 | Diffuse brain injury |
| S06.3 | Localized brain injury |
| S06.4 | Epidural bleeding |
| S06.5 | Traumatic subdural bleeding |
| S06.6 | Traumatic subarachnoid hemorrhage |
| S06.8 | Other intracranial injuries |
| ICD-10 online (WHO version 2019) | |
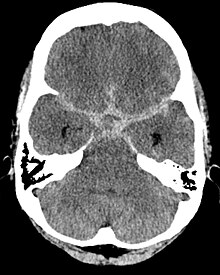
Colloquially, cerebral haemorrhage is an umbrella term for bleeding inside the skull (intracranial), in the area of the brain (intracerebral) or the meninges (extracerebral).
Cerebral haemorrhage in the narrower sense is only called intracerebral haemorrhage in the brain itself. This usually occurs suddenly, especially in people with high blood pressure, and manifests itself as a stroke . In the broadest sense, cerebral hemorrhages also include subarachnoid hemorrhage , epidural hemorrhage and subdural hemorrhage that occur in traumatic brain injury or vascular anomalies.
Bleeding in the brain can be life threatening. Many patients with a cerebral haemorrhage require neurosurgical treatment.
The incidence of cerebral hemorrhage in Germany is between 10 and 12 / 100,000 inhabitants.
causes
- trauma
- hypertension
- Vascular tumors
- Brain tumors
- Cerebral aneurysm (brain aneurysm)
- Vasculitis
- Coagulation disorder
- Treatment with anticoagulants ( anti-coagulants )
- Cerebral amyloid angiopathy
- Vascular malformations
If no cause can be proven, one speaks of spontaneous cerebral hemorrhage.
Above all, traumatic brain haemorrhages occur more frequently in alcoholics , as they often suffer falls while drunk, during which they hit their heads for lack of protective reflexes. In addition, people with alcohol dependency can have impaired blood clotting if the liver is damaged , which makes bleeding events easier and more complicated. The basal ganglia bleeding is a so-called loco typico bleeding (typical localization for the bleeding). The vessels make a "kink" in this area, which can encourage bleeding.
Intracranial, intracerebral bleeding
The intracerebral hemorrhage lies in the brain and results in an impairment of the brain function for which the affected brain tissue is required. The space-occupying behavior of the bleeding is determined by the size and location of the bleeding. Feared is the cerebral mass hemorrhage associated with mortality of 50 to 60% in the first year after the bleeding , which destroys large parts of the brain and can lead to entrapment .
Intracranial, extracerebral bleeding
Epidural hematoma

An epi dural hematoma occurs due to intracranial bleeding in the epidural space between the skull bones and dura mater , triggered by a trauma , usually with fractures of the skull.
A distinction is made between two forms with different prognostic dispositions:
In the case of an arterial epidural hematoma , the arterial vessels lying on the inside of the cranial bone tear, in particular the arteria meningea media . Typically, a symptom-free or symptom-free interval (latency) follows, which can also be completely absent, for minutes to hours. The bleeding progresses and increasingly pushes the dura mater and the brain inward. Nausea, vomiting, loss of consciousness and dilated pupils on the affected side are the consequences. There is danger to life. In the hospital, an emergency operation is usually carried out with opening of the skull ( trepanation ) or so-called Krönlein drilling (named after Rudolf Ulrich Krönlein ) behind and in front of the ear at the level of the eyebrows on the affected side to relieve pressure. With timely therapy, the chances of survival are around 70% (20% with disabilities).
In the case of a venous fracture hematoma, however, venous blood seeps from the fracture gap into the epidural space when the skull bone fractures. The bleeding, if progressive , is slow and minor.
Subdural hematoma

A subdural hematoma ( subdural hematoma , SDH) is a bruise ( hematoma ) under (Latin sub ) the hard meninges between the dura mater and the arachnoid .
The acute subdural hematoma occurs with severe skull injuries and additional damage. If the size and dynamics are appropriate, it must be relieved by opening the skull ( trepanation ) and, without surgery, usually ends fatally, especially if there is an existing midline shift.
The chronic subdural hematoma typically occurs as a result of slight head trauma, by definition after at least two weeks, whereby in most cases (in 50 percent of cases) no trauma can be found on exploration. Old age and anticoagulant conditions (from drugs or alcoholic liver damage ) favor its development. In older people, there is a physiological reduction in brain volume and thus a pull on the bridge veins , which can then be damaged by slight trauma. The outflow of blood via said bridge veins can be hindered by the subdural hematoma, so that there is also venous congestion of the part of the brain over which the subdural hematoma is located. Headache, feeling of pressure, disorientation, impaired consciousness, but rarely paralysis , especially hemiplegia , can result. The chronic subdural hematoma is also drained to the outside, the prognosis here is better than the acute one.
Subarachnoid hemorrhage
The subarachnoid hemorrhage (SAB) lies under the arachnoid membrane that covers the brain. This type of bleeding is arterial in nature and its leading symptom is a sudden headache event ( annihilating headache ) with nausea and vomiting.
Subarachnoid hemorrhage can occur in the event of a rupture of an aneurysm (malformation of the arterial vessel wall, which leads to a vascular sac with a deficient muscle layer) of the arteries from the cerebral artery (Willisi) or the large arteries arising from it. With a subarachnoid hemorrhage, in contrast to the two other types of bleeding, blood can be detected in the cerebrospinal fluid .
Depending on the cause of the bleeding, the subarachnoid hemorrhage is treated differently, from surgical to endovascular.
rehabilitation
To limit the consequential damage after a cerebral hemorrhage, long-term rehabilitation measures are often necessary, depending on the severity. Inpatient and outpatient rehabilitation attempts to reduce or eliminate neurological and physical dysfunction. In addition, the risk of further cerebral hemorrhage should be reduced and consequential damage limited. The ingestion of antihypertensive drugs (e.g. ambrisentan , bunazosin and gallopamil ) by the patient is usually part of the therapy after a cerebral haemorrhage caused by high blood pressure.
See also
Web links
Individual evidence
- ↑ cerebral hemorrhage. at: wicker-klinik.de , accessed on September 28, 2018.
- ↑ T. Hagen: The intracerebral hemorrhage in the context of amyoid angiopathy. In: The Radiologist. 1999; 39, pp. 847-854.
- ↑ Manio of Maravic: Neurological emergencies. In: Jörg Braun, Roland Preuss (Ed.): Clinic Guide Intensive Care Medicine. 9th edition. Elsevier, Munich 2016, ISBN 978-3-437-23763-8 , pp. 311–356, here: pp. 316–318 ( cerebral mass hemorrhage ).
- ↑ Ars Neurochirurgica: Acute subdural hematoma .
- ^ Dagmar Reiche: Roche Lexicon Medicine . 5th edition. Urban & Fischer, Elsevier, Munich et al. 2003, ISBN 3-437-15150-9 .
- ↑ Manio of Maravic: Neurological emergencies. In: Jörg Braun, Roland Preuss (Ed.): Clinic Guide Intensive Care Medicine. 9th edition. Elsevier, Munich 2016, ISBN 978-3-437-23763-8 , pp. 311-356, here: pp. 342 f. ( Epidural hematoma , subdural hematoma ).