Subarachnoid hemorrhage
| Classification according to ICD-10 | |
|---|---|
| I60.0 | Subarachnoid hemorrhage from the carotid siphon or carotid bifurcation |
| I60.1 | Subarachnoid hemorrhage originating from the middle cerebral artery |
| I60.2 | Subarachnoid hemorrhage originating from the anterior communicating artery |
| I60.3 | Subarachnoid haemorrhage from the posterior communicating artery |
| I60.4 | Subarachnoid hemorrhage originating from the basilar artery |
| I60.5 | Subarachnoid hemorrhage from the vertebral artery |
| I60.6 | Subarachnoid hemorrhage from other intracranial arteries |
| I60.7 | Subarachnoid hemorrhage from unspecified intracranial artery |
| I60.8 | Other subarachnoid hemorrhage |
| I60.9 | Subarachnoid hemorrhage, unspecified |
| I69.0 | Consequences of a subarachnoid hemorrhage |
| ICD-10 online (WHO version 2019) | |
The subarachnoid hemorrhage (from the Greek ἀραχνοειδής , "the spider-like meninges ", derived; see spider skin ; SAB) is a pathological occurrence in the area of the central nervous system . It is characterized by the fact that free blood enters the subarachnoid space filled with cerebrospinal fluid ( liquor cerebrospinalis ) .
In most cases, the cause of this special form of stroke is the bursting of an arterial vessel due to a deformity. The condition of free bleeding causes irritation of blood vessels in the brain and meninges . An accumulation of cerebral fluid with an increase in pressure in the skull ( hydrocephalus ) is typical of a complicated course.
The subarachnoid hemorrhage is accompanied by sudden severe headache and stiff neck. It can lead to short-term disorders of consciousness , but also to severe permanent brain dysfunction.
Incidence of illness, prognosis
The subarachnoid hemorrhage belongs to the group of apoplexies (strokes). It is responsible for 6 to 10 percent of strokes. According to the current study situation, it can be assumed that in industrialized countries about 10 people per 100,000 inhabitants per year suffer from subarachnoid hemorrhage ( incidence ). This corresponds to around 10,000 new patients per year in Germany. Worldwide, the incidence fluctuates quite strongly between 2 ( China ) and 22 ( Finland ) people per 100,000 people per year.
The age distribution of spontaneous subarachnoid hemorrhage differs from the age distribution of ischemic stroke. The most common SAB occurs after the age of 50. But it can occur at any age.
Women are affected slightly more often than men.
40 percent of the sick die within the first 30 days after the event. Of the survivors, 25 to 50 percent remain severely disabled. The mortality rate for recurrent bleeding (see section “Clinical presentation and severity classification”) is 50 to 70 percent.
definition
Anatomical basics
The subarachnoid space surrounds the brain and spinal cord like a fluid-filled cushion in which the brain literally floats in the cerebrospinal fluid, the cerebrospinal fluid . The brain is positioned in such a way that it is largely protected from damage caused by vibrations.
The walls of the subarachnoid space form the spider skin ( Latin: arachnoid ) on the outside and the soft meninges ( pia mater ) on the inside .
The arachnoid lies on the inside of the hard meninges ( dura mater ). It stretches across the surface of the brain, but, with the exception of the interhemispheric gap , does not extend into the individual cerebral furrows ( sulci ). From the arachnoid, small vascular bulges ( Granulationes arachnoideae ; Pacchioni granulations, named after the Italian anatomist Antonio Pacchioni, who first described them in 1705) protrude into the sinuses of the hard meninges, which are filled with venous blood . They regulate the amount of CSF and absorb excess CSF . The arachnoid is connected to the pia mater with fine threads .
The pia mater lies directly on the surface of the brain and follows it into all furrows.
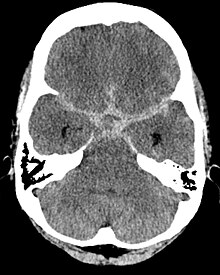
The subarachnoid space also houses the supplying blood vessels ( arteries and veins ). It is a narrow gap that is expanded to cisterns in some places (for example in the area of the brain base) . The blood often collects in the enlargements of the subarachnoid space and in the interhemispheric gap and can then be recognized by typical patterns using imaging methods ( computer tomography ).
Cause, risks and course of bleeding
Bleeding in the otherwise healthy brain usually occurs at particular weak points in the vascular system. These are mainly cerebral aneurysms . These are sac-shaped widenings of arterial vessel walls that lead to a thinning of the wall in the affected area.
Most aneurysms are congenital. They then mainly occur in places with increased blood flow stress. In particular, bifurcation points of arteries are at risk due to the formation of eddies and similar hemodynamic factors. Vascular sections that have been changed by arteriosclerosis or inflammatory arterial diseases are particularly affected . Much less often, aneurysms can also be acquired in the course of life. Fibromuscular dysplasia, polycystic kidney disease and connective tissue diseases such as Marfan's syndrome are more common .
In the event of a subarachnoid hemorrhage, this thin wall section can no longer withstand the stress of an otherwise perfectly tolerated rise in blood pressure and the vessel bursts at this point.
The vessels that form the cerebral arteriosis ( Willis ) are mainly affected . This vascular system at the base of the brain connects the largest arteries supplying the brain .
Ruptures (tears) of aneurysms of the brain base are the cause of subarachnoid hemorrhage in 80% of diseases; also come angiomas (benign vascular malformations) and arteriovenous malformations before. No source of bleeding can be found in 5–10% of all cases.
The bleeding usually occurs after situations with a brief increase in blood pressure , such as defecation (passing a stool), exertion, lifting heavy loads, or having sex. However, aneurysm ruptures can also occur spontaneously and calmly. Subarachnoid haemorrhage occurs more frequently in old age and during pregnancy. High blood pressure and smoking are recognized as proven risk factors for a rupture .
In contrast to first bleeding, which is only known based on its results, recurrent bleeding can be treated with causal therapy. Avoiding this recurrent bleeding is the goal of rapid diagnosis and surgical therapy.
In some cases, accidents ( traumatic brain injuries ) lead to subarachnoid hemorrhage. At the moment, however, it cannot be said with certainty whether the cause of the bleeding is not also here in the tearing of a deformity (e.g. aneurysm). Australian professional cricket player Philip Hughes died in November 2014 of a subarachnoid hemorrhage caused by a ruptured vertebral artery after being hit in the head by a ball during a cricket match.
Complications
The dreaded consequences of subarachnoid hemorrhage are:
- repeated bleeding (called recurrent bleeding )
- local vasoconstriction ( vasospasm )
- Hydrocephalus
- Hyponatremia
- epileptic seizures
- Brain edema
Recurrent bleeding
Most severe subarachnoid hemorrhages are multiple event. Heavy bleeding is usually preceded by minor ones; each bleeding can be followed by more. The cause of this recurrent bleeding lies in the fact that the vascular malformation that led to the previous bleeding continues to exist unless appropriate therapy has been carried out. About 35% of secondary bleeding occurs within the first three hours, up to 49% within the first six hours. 60% of patients who suffered rebleeding died in the first three months. Secondary bleeding occurs most frequently within the first three days after the initial event. With optimal medical care, their frequency is around 7%.
Vasospasm
The subarachnoid hemorrhage causes irritation of blood vessels. The result is an active narrowing (vascular or vasospasm ) of the affected vessels (primarily mediated by locally secreted vasoactive substances such as serotonin or prostaglandin ). This leads to an insufficient supply of the brain tissue with oxygen . On the one hand , the result can be an ischemic stroke , which, depending on the duration and size of the affected area, leads to permanent brain function damage. On the other hand, generalized vasospasms that set in later lead to an inadequate supply of the entire brain.
The vasospasm is the determining factor influencing the treatment outcome. It occurs with a frequency of 40 to 60 percent in subarachnoid hemorrhage. 1/3 of the spasms are only visible in their consequences (DIND = delayed ischemic neurological deficit ). Transcranial Doppler sonography (see below) is used for early detection of these conditions . Vasospasm usually occurs within 4 to 14 days - with a frequent peak between days 8 and 12 - after the initial event.
The cause of the vasospasm has not yet been clearly clarified. On the one hand, it is attributed to the action of substances that are released when the red blood cells ( erythrocytes ) break down . These substances are supposed to have a vasoconstrictor effect on healthy blood vessels ( endothelins , prostaglandins). An effect in the sense of blocking vasodilating (vasodilating) substances ( substance P ) is also conceivable. The released hemoglobin , which binds the NO necessary to maintain normal vascular caliber, plays an important role . This property is known as NO-scavenging . The resulting NO deficiency contributes to the narrowing of the arteries. On the other hand, local inflammatory reactions are also held responsible, which speaks for the activation of the complement system .
If the blood also penetrates the pia mater (soft meninges) (e.g. through a tear), then there is an additional hemorrhage into the brain tissue (so-called parenchymal hemorrhage ). This makes the course of the disease even more complicated, and permanent damage is more likely and greater.
Hydrocephalus
The dysfunction of the Pacchioni granulations ( granulationes arachnoideae ), the closure of the aqueduct and the exit points of the fourth ventricle can lead to a build-up of cerebral fluid ( hydrocephalus , "water head"). Since the cerebrospinal fluid is constantly being reproduced, there is, on the one hand, a disproportion between the space required by brain mass, normal blood volume and cerebral fluid and, on the other hand, the space available to the bony skull. This increases the pressure in the cranial cavity , which can lead to complex brain damage (for example through pinching of brain parts at the folds [ falx ] of the dura mater ). Depending on the cause, a distinction is made between aresorptive (Pacchioni granulations) and occlusive (aqueductus, exit points of the fourth ventricle) hydrocephalus.
The Hydrocephalus sometimes occurs immediately after subarachnoid hemorrhage, but sometimes days later. It can be shown very well in the computed tomogram (CT). Since hydrocephalus is very dangerous, a CT must be made immediately if this diagnosis is suspected. Hydrocephalus develops within the first 3 weeks after the initial event.
Hyponatremia
In 30% of patients, increased sodium excretion leads to a sodium deficiency in the blood ( hyponatremia ). The cause is probably the mechanical irritation of the hypothalamus with the result of increased secretion of antidiuretic hormone (SIADH). Reversible neurological symptoms occur at values below 125 mmol / l serum. Antidiuretic hormone leads to Na + secretion and H 2 O reabsorption in the kidneys and thus to dilution hyponatremia.
The problem lies in the treatment of hyponatremia. A too rapid equalization of the sodium levels can lead to central pontine myelinolysis with loss of nerve tissue in the area of brain stem structures. The greatest risk of developing hyponatremia is between the 4th and 14th day after the initial event.
Clinical picture and severity classification
The three main symptoms of subarachnoid hemorrhage are:
- sudden onset of devastating headache (so-called "thunderbolt headache")
- followed by short or long-lasting impaired consciousness up to unconsciousness (50% of cases)
- Neck stiffness ( meningism )
The brain itself is not sensitive to pain, but the arteries and meninges are. The typical sudden, devastating headache can be explained by the rupture of the vessel and the irritation of the neighboring vessels and the meninges.
The pain can also manifest in other places. In rare cases, it shows up in the chest, spine or legs. The spread of the blood in the subarachnoid space is probably responsible for this.
The disturbances of consciousness and the unconsciousness, however, are rather unspecific reactions of the brain to the stimulus. Symptoms of failure of the cranial nerves or focal (related to a specific region of the brain) epileptic seizures are rare in the acute situation. However, such variants are the trigger for occasional misdiagnosis.
The meningism , the third symptom is an expression of irritation of the meninges. The dura mater of the neck area reacts painfully to stretching, which can be checked by passive tilting of the head. In severe cases, the head is spontaneously overstretched towards the neck and the back is hollowed ( opisthotonus ).
Visual deterioration is seen in Terson syndrome , a vitreous hemorrhage that affects 10 to 20 percent of patients.
With subarachnoid hemorrhage, cardiac symptoms are also more common. ECG changes as well as cardiac arrhythmias are often neurogenic, i.e. that is, the damage to the brain causes an incorrect regulation of the heart's action. Bleeding into the heart muscle and heart attacks are also found to be above average. A malfunction of the hypothalamus , an important regulatory center in the brain , is suspected . These changes lead to an increased release of catecholamines , which causes a narrowing of vessels. This leads to an insufficient supply of oxygen in the heart muscle and the consequences mentioned.
Warning bleeding
Warning bleeding can also be detected in approximately 25 percent of patients with severe subarachnoid haemorrhage. The affected patients usually report sudden, extremely severe headaches (“like never before”), which in many cases can also trigger anxiety. After a short time they turn into a persistent headache or neck pain, which is usually no longer perceived as threatening. The pain is accompanied by a slight degree of neck stiffness. This type of warning bleeding corresponds to Hunt and Hess grade I (see table below).
The problem with this warning bleeding is primarily the correct detection. The complaints of patients, but also doctors, are often misinterpreted and incorrectly treated as migraines , extraordinary psychological stress or even spinal pain. A significantly more severe recurrent subarachnoid hemorrhage usually follows within 14 days.
Recognized early and correctly, in many cases the patient could be helped in a timely and efficient manner.
Severity classification
| Grade from WFNS or HUNT and HESS | corresponds to Glasgow Coma Scale | |
|---|---|---|
| I. | mild headache and / or meningism (neck stiffness), no neurological deficits | 15th |
| II | moderate to severe headache / meningism , no neurological deficits except cranial nerve disorders (here in combination!), no changes in consciousness | 13-14 |
| III | Somnolence or confusion and / or neurological deficits | 13-14 |
| IV | Sopor , severe neurological deficits, vegetative disorders | 7-12 |
| V | Coma (unconsciousness), extension synergisms, moribund patient | 3-6 |
The severity of the subarachnoid hemorrhage is classified according to the classification of the WFNS (World Federation of Neurological Surgeons) or according to HUNT and HESS (see table), which correlates well with the further course of the disease.
The Glasgow Coma Scale is a classification of the severity of traumatic brain injuries . It is advantageous to compare the two severity classifications, as the Glasgow Coma Scale, in contrast to the WFNS, is used very often in emergency services and the correlation becomes obvious.
The duration of unconsciousness is decisive for the severity of a subarachnoid hemorrhage. In most cases, patients wake up in a shorter time. However, 15 to 20 percent of patients remain in a coma.
Diagnosis
As with any other disease, the basis of diagnosis is the assessment of the clinical picture, including an assessment of the severity.
Imaging processes have proven to be a technical aid
proven.
Besides, they are
- Sonography (as a transcranial Doppler method) and the
- Lumbar puncture
established. The last two methods mentioned provide functional descriptions .
Computed tomography
The computed tomography (CT) of the head ( cCT ) is the fastest way to diagnose a subarachnoid hemorrhage. It has the highest sensitivity (100 percent on the first day of bleeding) and specificity of all imaging methods and can be performed quickly and safely for the patient under modern conditions - using a spiral CT with low loads. In 70 percent of cases, the source of the bleeding can be suspected from the first image. CT exams should be done immediately. Such a procedure enables rapid therapeutic action, since secondary bleeding would be life-threatening and must therefore be avoided. The classification according to Fisher allows a classification of the computed tomographic morphology:
- Grade 1: no evidence of bleeding
- Grade 2: subarachnoid hemorrhage less than 1 mm wide
- Grade 3: subarachnoid hemorrhage more than 1 mm wide, but without ventricular invasion
- Grade 4: Subarachnoid hemorrhage of any width with ventricular invasion (IVH) or expansion into the brain parenchyma
Angiography
Cerebral angiography is used as the standard method; it is a contrast agent-bound method of vascular imaging using X-rays . In the case of high sensitivity, however, it must be carried out in the first few hours, since the aneurysm must then be closed as a source of bleeding in order to gain therapeutic benefit. In its special form, digital subtraction angiography , the virtual vascular imaging methods of computed tomography and magnetic resonance imaging, this method, which has long been fully developed, is currently still superior in terms of diagnostic information. However, the latter are usually available more quickly and are less stressful for the patient.
Sonography
Transcranial Doppler sonography is used to assess vasospasm . As an ultrasound method, the method is virtually free of side effects. It should be used daily for the first ten days after the acute bleeding in order to detect vasospasms that are initially symptom-free (DIND - see above).
In the Doppler method, the flow rate of the blood is determined based on the reflection on the moving blood cells. While flow velocities below 100 cm / s are considered normal, values above 160 cm / s are considered critical.
Lumbar puncture
The classic lumbar puncture with the removal of liquor is highly sensitive. After just minutes, blood in the liquor in the lumbar spine is detectable in the case of a subarachnoid hemorrhage in the brain. This finding proves the subarachnoid hemorrhage purely qualitatively, the localization of the hemorrhage cannot be determined with it.
With this invasive method, there is a risk that the manipulation (leak in the lumbar dura mater ) and its consequences will result in uncontrolled loss of CSF. This can lead to negative pressure in the cerebral chambers . This pressure loss syndrome is associated with further damage to the brain. A lumbar puncture should therefore only be performed if the computed tomogram does not yield any results, but the patient's symptoms clearly indicate a subarachnoid hemorrhage.
It should also be noted that even small bleeding can occur during the lumbar puncture, but this is insignificant. However, they can stain the liquor with blood and simulate subarachnoid hemorrhage. The red blood cells ( erythrocytes ) disintegrate in the liquor, releasing the hemoglobin that is otherwise bound to them. This process depends on the elapsed time. Erythrocytes that are released in the skull in the event of a subarachnoid hemorrhage are no longer detectable in the liquor of the lumbar area, but their colorants are. In order to distinguish blood from a ruptured cerebral vessel from fresh blood (produced during the puncture), the bloody liquor must be centrifuged in order to be able to remove all cellular components. Should the CSF still show discoloration (so-called xanthochromic supernatant), the diagnosis would be confirmed.
therapy
First medical help
In the following, only therapy guidelines are described which, in their scientific maturity, meet the criteria of evidence-based medicine or have been included in the guidelines of the medical-scientific societies. These are those methods that demonstrably and effectively improve the survival and outcome of an affected patient. They represent the current status of the medical routine.
Subarachnoid hemorrhage usually requires observation and treatment methods of intensive care medicine .
The therapy primarily follows the unspecific goals of stabilizing the general condition. On the respiratory side, hypercapnia (increase in CO 2 in the blood due to insufficient breathing) must be avoided, as it can lead to increased intracranial pressure. That is why the decision to use ventilation is made generously. However, mechanical hyperventilation should also be avoided, since it may reduce the intracranial pressure for a short time through cerebral vasoconstriction, but the associated reduced perfusion can lead to ischemic brain parenchymnecrosis.
Targeted procedures pursue the objectives:
- Avoidance of recurrent bleeding
- Treatment of hydrocephalus
- Prevention and treatment of vasospasm
Avoidance of recurrent bleeding
There are the clipping and coiling proven. In addition to availability, the choice of method depends primarily on the specific conditions of the respective aneurysm (accessibility, shape, width of the aneurysm neck, origin of vessels):
- Clipping (closure with a clamp) of the aneurysm as a neurosurgical intervention to prevent secondary bleeding
- Coiling of the aneurysm as an interventional radiological method via an intravascular catheter. During coiling , a fine platinum coil is inserted into the aneurysm sac. This initiates coagulation processes that lead to sclerotherapy of the aneurysm via fibrin formation and connective tissue conversion.
Both methods, clipping or coiling , are usually carried out in the first 72 hours after the bleeding or 10 days later, as the vessels are particularly sensitive in the meantime and the development of vascular spasms is likely.
There is high evidence that surgical therapy is suitable for the prophylaxis of recurrent bleeding.
The coiling offers the advantage that it can penetrate the patient gently to the affected vessel sites without depending on the location of the aneurysm, opened the skull and brain tissue injured or needs to be removed. It is also suitable for the prophylaxis of asymptomatic aneurysms.
Prevention and treatment of vasospasm
The current guidelines for the treatment of SAB recommend the administration of the calcium channel blocker nimodipine in all patients. Calcium antagonists relax precapillary sphincters , i.e. muscular parts of arterial vessels. You thus counteract the vasospasm in the subarachnoid hemorrhage. The calcium antagonist nimodipine accumulates strongly in the brain due to its particularly high fat solubility and is therefore suitable for the treatment of subarachnoid hemorrhage. If given prophylactically, nimodipine is ideally given in tablet form. A mortar for administration through a gastric tube reduces the effect. If not otherwise possible, nimodipine can also be administered intravenously.
If the aneurysm bleeding is not supplied, the blood pressure should be kept at a mean arterial pressure of 60 to 90 mmHg, which corresponds to a highly normal blood pressure. A normal fluid balance should also be aimed for (normovolemia). Body temperature, blood sugar levels and blood salts should be kept within the normal range.
| Hydroxyethyl starch (HAES 130 10% 500–1000 ml / die) and crystalloid solution 3000–10000 ml / day (!) | Hemodilution (thinning of the blood) and hypervolemia (increase in blood volume) to reduce the viscosity of the blood. The thinner blood should be able to overcome the "bottleneck" in the area of vasoconstriction better. |
| inotropic substances (dopamine hydrochloride 3–30 µg / kg / min or noradrenaline) | Hypertension to increase the internal pressure of the vessels ( perfusion pressure ) with the aim of pressing open the "constriction" from the inside so that blood can reach the capillary vessel areas. Systolic (upper) blood pressure values of up to 240 mmHg are aimed for when the aneurysm is clipped. |
According to the current guidelines, the so-called triple H therapy is only recommended if vasospasms with neurological deficits occur despite the preventive measures:
- Hypervolemia
- hypertension
- Hemodilution
The 3H therapy aims to improve the disturbed blood flow in the damaged brain tissue by means of a high internal vascular throughput. For this purpose, the flow (hypervolemia) and the internal pressure of the vessels are increased (hypertension) and the viscosity (toughness) of the blood is lowered by reducing the erythrocyte volume ("blood thinning" (hemodilution)). The procedure requires strict monitoring in order to keep an overhydration of the organism with effects on gas exchange (respiration, lung function) and the circulatory system within acceptable limits.
Attempts can also be made to depict the vasospasms by means of angiography and to reduce the vasospasms by balloon dilatation and / or intra-arterial administration of vasodilating substances. However, these procedures are not generally recommended for all patients, so that an experienced practitioner has to decide on each individual case based on the location and extent of the spasms.
According to the current state of research, the following therapies have no proven effect and should no longer or not yet be used: platelet inhibitors, tirilazad, magnesium, corticosteroids, erythropoietin and clazosentan. Statins are still being tested.
Treatment of hydrocephalus
In addition to regular intensive care with securing gas exchange (ventilation), the installation of a ventricular catheter remains the method of choice. The catheter is used to drain excess CSF from the ventricular system (cerebral chambers) to the outside.
30% of patients also suffer from hydrocephalus later . In these cases, the liquor can be drained into the peritoneum, for example, via a permanently implanted shunt system .
literature
- Klaus Poeck, Werner Hacke: Neurology. 11th edition. Springer, Berlin 2001, ISBN 3-540-41345-6 .
- S1 guideline for subarachnoid hemorrhage of the German Society for Neurology. In: AWMF online (as of 2012)
Web links
Individual evidence
- ↑ MJ Wood, AM Nowitzke: Epidemiological aspects of spontaneous subarachnoid haemorrhage in Queensland, Australia. In: J Clin Neurosci. (2005); 12 (7), pp. 770-774.
- ↑ LH Pobereskin: Incidence and outcome of subarachnoid haemorrhage: a retrospective population-based study. In: J Neurol Neurosurg Psychiatry. (2001); 70 (3), pp. 340-343.
- ^ OG Nielsson u. a .: Incidence of intracerebral and subarachnoid haemorrhage in southern Sweden. In: J Neurol Neurosurg Psychiatry. (2000); 69 (5), pp. 601-607.
- ↑ a b T. Ingall u. a .: A multinational comparison of subarachnoid hemorrhage epidemiology in the WHO MONICA stroke study. In: Stroke. (2000); 31 (5), pp. 1054-1061.
- ↑ a b H. H. Steiner, G. Ranaie: The acute subarachnoid hemorrhage. In: Eckart, Forst, Burchardi (Hrsg.): Intensivmedizin. ecomed, 2004, ISBN 3-609-20177-0 .
- ↑ a b c d e f g h i Guideline for subarachnoid hemorrhage of the German Society for Neurology . In: AWMF online (as of 10/2005)
- ↑ Barbara I. Tshisuaka: Pacchioni, Antonio. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 1087.
- ^ Phillip Hughes: Doctors reveal condition 'incredibly rare' with only one other case resulting from cricket ball ever reported . In: ABC News .
- ↑ AM Naidech u. a .: Predictors and impact of aneurysm rebleeding after subarachnoid hemorrhage. In: Arch Neurol . (2005); 62 (3), pp. 410-416.
- ^ DS Pine, L. Tierney Jr .: A stressful interaction. In: N Engl J Med. , 1996, 334, pp. 1530-1534. PMID 8618610 (cardiac changes in subarachnoid hemorrhage)
- ↑ Timo Krings et al. a .: Diagnostic imaging to clarify the headache. In: Deutsches Ärzteblatt. 45/2004, p. 3026 ff.
- ↑ CM Fisher, JP Kistler, JM Davis: Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. In: Neurosurgery . 1980; 6, pp. 1-9. PMID 7354892