Ischemic Stroke
| Classification according to ICD-10 | |
|---|---|
| I63.- | stroke |
| ICD-10 online (WHO version 2019) | |

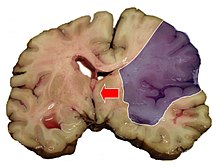
The ischemic stroke or cerebral infarction or "white" Stroke is the most common form of stroke . The cause is a sudden decrease in blood flow to the brain, known as ischemia , and thus an insufficient supply of oxygen and glucose , which are required for energy production. The reduced blood flow is usually caused by constrictions or blockages in the arteries that supply the brain . The ischemia can be reversible or lead to the death of nerve cells and other brain cells. Then a cerebral infarction occurs.
The individual regions of the brain fulfill different functions. These regions are supplied by blood vessels that vary between individuals only within narrow limits. As a result, a circulatory disorder in a certain blood vessel can normally be associated with a certain symptomatology, which can be explained by the failure of the brain area dependent on the blood vessel.
Cerebral infarction is a medical emergency and is one of the leading causes of disability and death in industrialized countries. Therapy only has a chance of success within a narrow timeframe and is preferably carried out in specialized departments, so-called stroke units . In aftercare, occupational therapy , physiotherapy , speech therapy and, in certain cases, psychotherapy are used.
Occurrence and frequency
After heart attacks and malignant neoplasms (cancer), stroke is the third most common cause of death in Germany, accounting for 15 percent of all deaths. Among the strokes, ischemic strokes form the largest group with around 80 percent. In addition, the stroke is the most common cause of acquired disabilities in adulthood. Studies on the epidemiology of stroke give an incidence of 182 / 100,000 for Germany . In absolute terms, this is 150,000 new strokes and around 15,000 recurrences per year. The prevalence is around 600 / 100,000 inhabitants per year. Stroke is also the most common cause of need for care in old age.
causes
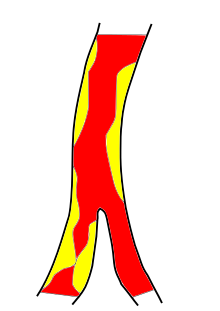
Macroangiopathy
Changes in large vessels are generally referred to as macroangiopathy. A common cause of ischemic strokes is macroangiopathy of the large arteries supplying the brain, which is usually caused by atherosclerotic plaques. Various mechanisms, such as an increase in blood pressure and infection, can cause the plaques to tear (rupture) and blood clots to form. These local arterial thromboses can, on the one hand, lead to a narrowing of the vessel, so that the cerebral blood flow behind the constriction is reduced and may be insufficient for the supply of the brain tissue (see the section on thrombosis ). On the other hand, the local thrombi can be carried away with the bloodstream and thus trigger an embolism . The embolus can then occlude a more distant blood vessel (see the Embolism section ).
TOAST classification
The differentiation according to TOAST ( Lit .: Adams 1993) is common, but controversial , figures for Germany:
- Cardiac embolism : Blood clots form in the heart, which are flushed into the vessels supplying the brain and block them ( incidence : 30.2 / 100,000)
- Small artery occlusion (25.8 / 100,000)
- Atherosclerosis of large arteries (15.3 / 100,000)
- other cause (2.1 / 1,000,000)
- undetermined cause (including competing causes and ESUS , 39.3 / 100,000) ( ref : Kolominsky-Rabas 2001)
Disease emergence
Interruption of the substrate supply
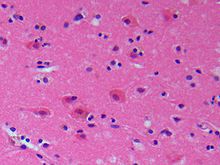
Like other tissues, brain tissue is supplied with energy substrates and oxygen via the blood. The brain gets its energy mainly from breaking down glucose . Over 95 percent of the glucose is broken down via glycolysis and the respiratory chain , for which oxygen is required (aerobic metabolism). If there is a lack of oxygen, the glucose is broken down to a greater extent via the anaerobic metabolic pathway (glycolysis and lactic acid fermentation ). In the anaerobic metabolic pathway, the energy yield is significantly lower. Because of this, and due to the low levels of glucose and oxygen, an interruption in the supply of substrate can only be tolerated for a short time. If the oxygen supply is completely interrupted, the oxygen in the cell-rich gray matter is consumed after 68 seconds and the glucose after 34 minutes. After 4 to 5 minutes, the first nerve cells die (“ necrosis occurs”).
Cerebral blood flow, ischemia and infarct threshold
The cerebral blood flow (CBF) is a measure of the cerebral blood flow. In addition to the cerebral blood flow, the glucose and oxygen levels in the blood are important parameters. The cerebral blood flow depends on cardiac output and blood pressure, the peripheral vascular resistance and the pressure in the cranial cavity ( intracranial pressure ). Like other body cells, brain cells have a structural metabolism to maintain the cell structure and a functional metabolism to exercise the active functions. The energy requirement for functional metabolism is higher than that for structural metabolism.
If the cerebral blood flow or the energy supply falls below the so-called functional threshold, the brain cells initially stop their active function reversibly. Ischemia occurs . However, this state can only be maintained for a certain period of time. If ischemia persists, an infarction occurs because the cell structure can no longer be preserved. If the cerebral blood flow or the energy supply falls further and below the so-called infarct threshold, the brain cells are also irreversibly damaged and die, so that a heart attack occurs.
Embolisms
The transfer of particles with the bloodstream is called an embolism. The ischemic stroke of embolic origin is caused by an occlusion of one or more arteries supplying the brain. These particles can consist of different components. According to the main components, the embolism is referred to, for example, as thromboembolism or as fat embolism .
Mostly, thromboembolism is responsible for the development of ischemic strokes. The embolus then originates either from the heart (cardiac embolism) or from the arteries supplying the brain (arterio-arterial embolism) . Various heart diseases such as atrial fibrillation , heart valve disease, acute myocardial infarction , coronary artery disease , heart failure and enlargement of the heart chambers ( ventricular hypertrophy ) increase the risk of cardiac embolism. The cardiac embolism also includes the paradoxical embolism that can arise in patients with venous thrombosis and persistent foramen ovale . Arterio-arterial emboli arise from arteriosclerotic changes in the arteries. Common origins are the aorta , the carotid fork, and the left and right carotid arteries .
Thrombosis
Blood clots in blood vessels are called thromboses. Cerebral infarctions can be triggered by thrombosis of the arteries supplying the brain. Most arterial thromboses arise in those parts of the vascular system where arteriosclerotic changes in the vascular wall exist. However, they can also occur when the inside of the vessel wall ( tunica intima ) is damaged. This is the case, for example, with dissections in which a tear in the inner vascular wall causes bleeding into the vascular wall (between tunica intima and tunica media ). Other causes of arterial thrombosis are inflammation of the vessel walls ( vasculitis ) and coagulation disorders, as well as foreign bodies within the vessel, for example stents and vascular prostheses .
Arterial thrombosis can develop slowly or quickly. Thromboses that develop slowly are only hemodynamically relevant when there is severe constriction ( stenosis ) of the interior of the vessel, which means that only then is the blood flow no longer sufficient to supply the brain tissue.
Hemodynamic Mechanisms
If the cerebral blood flow is insufficient to supply the brain tissue, an ischemic stroke can occur. This can be the case, as described in the Thrombosis section, due to a local constriction or in the case of systemic disorders of the blood flow, such as severe hypotension, for example after a heart attack , in which the cardiac output can be reduced.
Stroke risk factors
The most important risk factors for ischemic stroke that have been confirmed in large studies are:
- Old age : the stroke rate doubles per decade after the age of 55
- Gender: 24–30% higher in men than women
- Ethnicity : 2.4 times for African Americans , 2 times for Hispanics , bleeding rate higher for Han Chinese and Japanese
- Genetic predisposition : 1.9-fold in first-degree relatives
- High blood pressure : 3–5 odds ratio (OR) affects 25–40% of the population
- Cardiac arrhythmias ( atrial fibrillation ): 5–18 OR (1–2% of the population)
- Diabetes mellitus : 1.5–3.0 OR (4–20% of the population)
- Lipid metabolism disorders : 1–2 OR (6–40% of the population)
- Smoking : 1.5–2.5 OR (20–40% of the population)
- Alcohol disease : 1–3 OR (5–30% of the population)
- Lack of exercise : 2.7 OR (20-40% of the population) ( Lit .: Guidelines 2003)
Classifications
In addition to classifications according to etiology and pathogenesis, numerous other classifications are possible. Classifications based on the time course, the infarct pattern in the imaging, the affected brain wave area and the severity of the symptoms are widespread.
Classification according to time
In the past, a stroke was divided into the following stages according to the time course:
- TIA ( Transient Ischemic Attack ) - symptoms usually go away in less than an hour, by definition they last less than 24 hours. A TIA is a predictor of a completed heart attack (various studies show an average annual risk of between 2.2 and 6.3% of suffering a completed stroke after a TIA).
- PRIND (term for "(prolonged) reversible ischemic neurological deficit") - good regression with only minimal, non-disabling symptoms without time limit. The term RIND / PRIND stands for findings that last longer than 24 hours but shorter than three weeks. A standardization of all relevant term definitions is to take place in a new guideline.
- progressive infarction; the neurological symptoms increase over time.
- complete infarction; The stroke leaves behind a neurological deficit of varying severity, also: condition after apoplexy (ZnA).
The brain is able to partially compensate for damage to brain tissue and the associated symptoms by having other brain cells take over the function of the dead ones. This so-called plasticity depends on various factors such as B. the age of the patient or the nature of the disease. In most cases, however, the cause (such as atherosclerosis or atrial fibrillation ) of the stroke persists and must therefore be treated consistently.
Classification according to the infarct pattern in the imaging
A distinction can be made between territorial infarcts, border zone infarctions and lacunar infarcts.
Territorial infarcts arise from embolic occlusion of arteries supplying the brain and affect the supply area (territory) of the vessel. Lacunar infarcts are smaller than 1.5 cm. They mostly arise from microangiopathic changes. Border zone infarcts are hemodynamic in origin. They usually arise from the occlusion of the large extracranial vessels or from a temporary drop in blood pressure when the carotid arteries are constricted.
Symptoms
In ischemic stroke, several symptoms typically appear suddenly . The symptoms can also fluctuate or gradually increase. The symptoms do not allow a differentiation of the causes of a stroke.
- Clouding of consciousness : This can range from a slight drowsiness to tiredness ( somnolence , sopor ) to unconsciousness or a deep coma . In the worst case, a stroke can lead to death within minutes due to respiratory failure. The disturbance of consciousness is one of the main symptoms of infarcts in the posterior (vertebrobasilar) river area.
- Nausea, vomiting
Other key symptoms that are typical of a cerebral infarction:
- Half-sided paralysis ( hemiparesis ) or paralysis of one limb (rarely paralysis of all extremities)
- Pathological reflexes of the Babinski group
- Involvement of cranial nerves (difficulty swallowing, lumpy language)
- Neuropsychological deficiency symptoms ( aphasia , alexia , apraxia , neglect , cognitive dysphasia )
- Turning the head or gaze ( focus view )
- Visual field loss ( hemianopia )
- Memory loss ( amnesia )
Strokes in the anterior flow area
- For an overview of the blood supply to the brain see there.
The following symptoms can occur in unilateral infarcts of the internal carotid artery (ACI) (50% of all insults ), cerebral artery (ACM) (25% of cases) and in infarctions of vessels that branch off from them (partial infarctions). In the case of infarcts on both sides, the same symptoms are found, extended to both halves of the body:
- Unilateral, varying degrees of paralysis of the extremities ( hemiplegia , hemiparesis). The crossing of nerve fibers in the intersection of the pyramids affects the left side of the body and vice versa in the event of a heart attack in the right hemisphere.
- The face can also be paralyzed on one side (e.g. drooping corner of the mouth due to facial paresis ).
- With hemiplegia, the feeling of warmth, cold, pressure and the position of the affected half of the body can be lost (often temporarily). This can also be seen in abnormal sensations or numbness on the affected side of the body (sensory disturbance, sensory disturbance).
- Perception disorder ( neglect - can affect sight, hearing, feeling and motor skills) of one half of the body and the environment on the affected side. With this disorder, the affected side is not available to the patient. The patient does not notice that his perception is disturbed, so he cannot notice any hemiparesis that may occur at the same time.
- Visual disturbance in which half (or a quarter) of the field of vision is no longer visible in both eyes ( hemianopia or quadrant anopia ); Disruption of the processing of image information in the brain.
- Turning both eyes to the affected side of the brain: Déviation conjuguée ("focus view")
- Disturbance of language or difficulties in understanding what is being said ( aphasia ) if the language-dominant hemisphere of the brain (mostly on the left) is affected.
- Swallowing disorders (disorders of the cranial nerves IX , X and XII ).
- Apraxia , d. H. Inability to perform certain actions: button buttons, talking on the phone, etc. v. a. m.
- Disruption of general brain functions, such as concentration, memory, flexible reaction to environmental demands ...
Strokes in the posterior river basin
The rear part of the cerebrum as well as the brain stem, bridge and cerebellum are supplied from the arteriae vertebrales , which unite to form the unpaired arteria basilaris . The arteria cerebri posterior (so-called posterior cerebral circulation) arises from this on both sides , about 10% of which is infarcted.
In the case of an infarction in the area of the posterior cerebral circulation, the following can occur:
- Sudden onset of dizziness with nystagmus
- Unsteady gait, insecurity when grasping objects due to excessive arm and hand movements ( ataxia )
- Tremor ( tremor )
- Double vision due to eye movement disorders ( cranial nerve III )
- Gaze paresis (paralysis), d. That is, the view is only possible in certain directions
- Pain in the back of the head
- Scant blinking of an eye
Diagnosis and differential diagnosis

The primary diagnosis includes:
- a thorough medical history survey
- the physical (neurological) examination
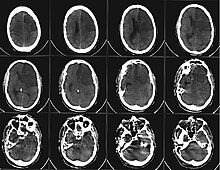
- This is usually followed by imaging diagnostics: In the past, computed tomography of the skull ( CCT ) was always performed first . This enables a quick distinction to be made between an ischemic stroke and a cerebral hemorrhage. This is important for the therapy decision. Today the MRI (with contrast agent) offers all the information that is needed to make a therapy decision. If one compares different recordings from different recording techniques, the size of the area can be estimated which has not yet been damaged, but has a reduced blood supply ( penumbra ). The size of this area should provide information about the chances of success of a possible therapy. However, there are still no larger studies on this assertion ( Lit .: Schellinger et al. 2003). Also, tumors or inflammatory changes in the brain ( meningitis , encephalitis ) or sinus thrombosis can be detected with it. It is more efficient in early diagnosis, but also slower and more expensive. Since no contrast agent may be used in a hemorrhagic insult, a CT is usually still done before the MRI.
- A Doppler sonography of the extra- and intracranial vessels is used to determine structural changes in the vessels supplying the brain, such as B. Atherosclerosis or dissections .
- An angiography may v. a. In the case of cerebral haemorrhage, it may be necessary to display extra- and intracranial vessels in order to display aneurysms , angiomas or arteriovenous malformations .
- A lumbar puncture with examination of the cerebrospinal fluid (cerebral fluid) is without diagnostic added value if an ischemic infarct is suspected. In the case of subarachnoid hemorrhage , however, blood or its breakdown products (xanthochromia) can be detected in the CSF.
- An EKG is used to detect cardiac arrhythmias that can cause thrombi and thus embolisms .
- An EEG is used to check the brain waves .
The differential diagnostic options for ischemic stroke are diverse:
- other disorders of blood flow: cerebral hemorrhage , sinus thrombosis , hypertensive crisis , aortic dissection
- Blood composition disorders: hypoglycemia , hyperglycemia , hypokalaemia , uremia, etc. a.
- Infections: meningitis , encephalitis , brain abscess , neurolues , toxoplasmosis, etc. a.
- Brain tumors
- primary disorders of the excitability of nerve cells such as epilepsy including Todd's palsy
- Reactive or autoimmune diseases : Guillain-Barré syndrome , multiple sclerosis
- Forms of migraine , such as migraine accompagné
- mental disorder
- Spinal cord disorders, such as incomplete paraplegia
therapy
Admission to the stroke unit
Even for the initial treatment of patients with a stroke (apoplexy) or who are suspected of having a stroke, hospital admission should, if possible, take place in a special ward for stroke patients, a so-called stroke unit . The first goal there is to offer the patient a quick and optimal diagnosis in order to determine the optimal therapy. Further treatment is based on intensive ongoing monitoring of the patient. The basic parameters of blood pressure, pulse, temperature, blood sugar and breathing are continuously monitored. The close cooperation between various medical disciplines such as neurologists, internists, neurosurgeons and radiologists is another advantage of the stroke unit, as is the early initiation of long-term rehabilitation (physiotherapy, occupational therapy , physiotherapy , speech therapy , provision of aids).
Lysis therapy (thrombolysis)
Do not speak of contraindications such as old age, serious pre-existing illnesses or similar. on the other hand, and if a cerebral hemorrhage has been ruled out by means of computed tomography , according to the latest study results (meta-analysis of the ECASS I-III and ATLANTIS studies) an attempt can be made within 4.5 hours to dissolve the blood clot (the thrombus ) ( lysis therapy ) to supply blood to the under-supplied brain area again and to contain the long-term effects. The sooner the therapy can be started, the better (“ time is brain ”). A distinction is made between systemic lysis therapy (drug is distributed throughout the entire circulation) and locally applied lysis therapy. The greatest danger in the context of lysis therapy is secondary bleeding. These can occur because blood is inhibited from clotting for hours. This can lead to bleeding in the brain with a further deterioration in the neurological status as well as blood loss through other existing wounds. Risk factors for relevant bleeding are old age, major infarction and previous damage to the smallest brain vessels (microangiopathy of the brain, especially the white matter). An American and a European study (e.g. European Cooperative Acute Stroke Study - ECASS) showed the positive effects of systemic lysis therapy in patients with ischemic stroke. It has not yet been finally clarified whether patients still benefit from lysis therapy after six hours or whether the risks of the side effects outweigh this. At present, lysis therapy in Germany is normally only carried out up to three hours after the onset of symptoms; In the case of certain rare sub-forms of stroke, however, this time window can be extended to six or even twelve hours ( Lit .: Guidelines 2002). In September 2008, the third European study on the treatment of stroke with lysis therapy showed that treatment can be carried out up to 4.5 hours after the onset of the symptoms of failure. An individualization of the lysis therapy concept is currently being lively discussed in the professional world. For example, by using magnetic resonance imaging (MRT), a lysis can be useful even after the 4.5 hour window (or if the onset of symptoms is unclear, e.g. when waking up from sleep (wake-up stroke)) if the size the actual tissue damage and the extent of the existing circulatory disturbance differ from each other (so-called diffusion-perfusion weighting mismatch). An MRI examination that is at least as sensitive as a computed tomography should not lead to a significant delay in the start of therapy, because the earlier a lysis therapy begins, the more effective it is. The selection of patients for lysis therapy is also currently being scrutinized. That is, one also considers subjecting patients with very severe or very mild failure symptoms to such therapy, since the medium-term result (i.e. after 90 days) appears to be better than without lysis. In addition, new drugs are being tested to extend the time window. However, expectations of the drug derived from blood-sucking bats with the inhibitor Desmoteplase , which should be used up to 9 hours after the onset of symptoms, could not be met (DIAS-2 study).
breathing
Care should be taken to ensure sufficient oxygen saturation of the blood. Secure data from prospective studies are currently not available. In patients who do not require intubation , the DGN recommends the administration of oxygen only in the case of severe symptoms, a peripheral oxygen saturation below 95% and at a dose of 2 to 5 liters / minute via a nasogastric tube. The general administration of oxygen was discussed controversially in 2012. If there are pathological breathing patterns, clinical or laboratory evidence of respiratory insufficiency , risk of aspiration or increasing clouding of consciousness, ventilation is indicated.
Blood pressure
According to common doctrine, blood pressure must not be lowered too far or too quickly, especially not in patients with pre-existing high blood pressure. The aim is to try to maintain the blood flow in the area of the penumbra by increasing blood pressure, since the autoregulation of the blood pressure is disturbed in this area and therefore the blood flow is dependent on the systemic arterial blood pressure. Unadjusted lowering of blood pressure can worsen the symptoms . As a guideline, medication should only be used in the acute phase if the blood pressure exceeds 220/120 mmHg. Conversely, it may also be necessary to use drugs to raise blood pressure to highly normal values. After about three days, blood pressure values above 180/100 mmHg should be treated, in patients with high blood pressure values above 180/105 mmHg. However, the study situation is not sufficient. Neither the use of blood pressure-increasing nor blood pressure-lowering substances is sufficiently proven ( Lit .: Blood pressure 2000). Currently, a large study (CHHIPS) is on this subject carried out ( Ref : Potter 2005).
Thrombosis prophylaxis
Since stroke patients with more pronounced symptoms of paralysis have a significantly increased risk of thrombosis and pulmonary embolism , adequate thrombosis prophylaxis must be carried out from the start. This can with Na - or Ca - heparin s. c. or low molecular weight heparin s. c. be performed. In addition, medical thrombosis prophylaxis stockings (MTPS) are used and early mobilization is sought as thrombosis prophylaxis.
Blood sugar
A normoglycemia or a highly normal blood sugar value (ie a blood sugar value less than 8.9 mmol / l [160 mg / dl]) is aimed for. Here one thinks v. a. on the brain metabolism, whereby both hypoglycaemia and hyperglycaemia have negative effects on the viability of nerve cells.
Body temperature
An elevated body temperature or a fever can worsen the prognosis after an ischemic stroke. It is recommended to actively lower body temperatures above 37.5 ° with anti-fever medication ( antipyretic ). However, there are no controlled studies on the active lowering of elevated body temperature by means of medicinal treatment or cooling. The increase in body temperature can be central or caused by infections. A search for an infection is recommended, but no prophylactic antibiotic therapy.
Brain edema
Sufficient sedation and analgesia must be carried out beforehand to treat the cerebral edema . Therapy is based on the principles of hyperosmolarity and hyperventilation . Hypervolaemia and hyperosmolarity can be achieved with substances such as mannitol or glycerol ; there must be a close-knit control v. a. the electrolytes and hemoglobin done since the most common side effects hemolysis , overhydration and electrolyte derailments are (due to overhydration). It should be noted that the effect of hyperosmolarity is only short-term and a rebound phenomenon is to be expected.
The drop in arterial carbon dioxide partial pressure (paCO 2 ) that occurs during hyperventilation leads to alkalosis and vasoconstriction . Hyperventilation must not be carried out too aggressively, since otherwise the infarct process is intensified by the vasoconstriction. As a rule of thumb, lowering paCO 2 to 30 mm Hg leads to a decrease in intracranial pressure of about 30%. Short-term hyperventilation with paCO 2 of 35 mm Hg (lower normal limit) is currently recommended .
Hypothermia treatment with a cooling down to 32–34 ° C body temperature is currently in the study status and is only being carried out in a few centers, but seems to be promising in patients with craniocerebral trauma.
If the intracranial pressure rises and it is likely or cannot be controlled acutely with medication, then neurosurgical decompression in the form of hemicraniectomy can be considered (e.g. for space-occupying, so-called malignant media infarction). The decisive factor is the early decision on such a decompression operation, i. H. just a few days after the stroke, when massive swelling starts (and not only when the swelling is fully developed). Several large randomized controlled studies (DECIMAL, DESTINY and HAMLET) have shown that hemicraniectomy significantly increases the chances of survival and less severe disability in patients under the age of 60 with a malignant cerebral infarction. However, the proportion of patients with severe disabilities dependent on help is also increasing, so it is recommended that the presumed will of the patient be included in the therapy decision.
Even in patients over 60, a hemicraniectomy seems to significantly increase the chance of survival, as was shown in another randomized-controlled Destiny II study, the results of which were published in 2014. A third of these elderly patients have severe disabilities and will be permanently dependent on outside help.
The use of steroids is controversial, the current recommendations speak out against the administration of cortisone preparations in cerebral infarctions, since the swelling is caused by the damaged nerve cells themselves (in contrast to the so-called "vasogenic" edema in brain tumors, which is excellent for cortisone -like drugs like dexamethasone may respond).
prophylaxis
Treatment of risk factors ( as ) part of the secondary prevention of further infarctions mandatory for therapy. Second myocardial infarction has a much worse prognosis than the primary one.
As a rule, ASA medication is used to prevent further strokes . Only if there is an increased risk of recurrence (e.g. due to a simultaneous peripheral arterial occlusive disease) is this carried out with an ASA- dipyridamole combination preparation , clopidogrel or phenprocoumon . When selecting the appropriate drug, the other risk factors must be considered.
If the cause is a narrowing (stenosis) of a carotid artery , the current guidelines recommend surgical or interventional radiological therapy in the form of a stent angioplasty to remove the stenosis ("carotid desobliteration"). The SPACE study showed that both therapies had similar successes, with surgery appearing to have a slight advantage. It is important that an operation is carried out as early as possible, i.e. H. should take place a few days after the stroke or TIA, because only then will the benefits outweigh the risks of the operation.
Complications
- Aspirations can occur in the course of the disease , especially if there is difficulty swallowing ( dysphagia ) . This is understood as the entry of saliva, food or vomit into the airways. This can lead to pneumonia.
- "Post-stroke depression "
- Seizures or epilepsy can occur after the infarction .
- A primary ischemic infarction can bleed in secondarily. Clinically, this is usually a second event. In such a case, the therapeutic approach is the same as for intracerebral hemorrhage .
- The dead brain tissue and the penumbra can swell so much that a space-consuming infarct develops. The pressure in the brain increases. In order to avoid entrapment and thus the death of the patient, space may have to be surgically created by temporarily removing part of the skull ( decompression craniectomy ).
rehabilitation
In post-stroke treatment, attempts are made to relearn lost skills so that the stroke patient can cope with life independently. In some cases, other regions of the brain can take over the functions of the failed areas. Traditionally, attempts are made to help the patient with the help of physiotherapy , occupational therapy , speech therapy and neuropsychology (including the earliest possible care and therapy according to the Bobath concept ); further treatment concepts are mirror therapy and video therapy .
forecast
Some stroke patients go into a coma or die. One year after a stroke (in the broader sense), 60% of patients are still alive. 64% of the patients who survive the first year are dependent on outside help. 15% of them have to be cared for in nursing homes. The average annual risk of stroke again is 6% for about five years. In the first 6 months after a stroke it is 9%, in the first year it is between 13 and 14% and then drops to 4–5% in the following years. The cases in which the symptoms disappear again after a short time (see TIA and PRIND ) should give the person concerned a reason to seek medical advice on preventive measures in order to prevent a possible recurrence. Dead nerve cells can no longer be reproduced, but other parts of the brain can still take over the lost function after a few weeks through learning processes. Early regression gives a favorable prognosis.
literature
- Jörg Braun, Roland Preuss: Clinical Guide Intensive Care Medicine. 6th edition. Elsevier, Urban & Fischer, Munich 2005, ISBN 978-3-437-23760-7 .
- Gerhard F. Hamann, Mario Siebler, Wolfgang von Scheidt: Stroke: Clinic, Diagnostics, Therapy, Interdisciplinary Manual. ecomed Verlagsgesellschaft, 2002, ISBN 3-609-51990-8 .
- Graeme J. Hankey: Long-Term Outcome after Ischaemic Stroke / Transient Ischaemic Attack. In: Cerebrovasc Dis. 2003; 16 (suppl 1), pp. 14-19 doi: 10.1159 / 000069936 .
- Peter Kolominsky-Rabas: Indicative figures on stroke from the population-based Erlangen stroke register as part of federal health reporting. 2004, URL: [1]
Further literature
- Klaus Poeck, Werner Hacke: Neurology . Textbook. 12th edition. Springer, Berlin et al. 2006, ISBN 3-540-29997-1 .
- HP Adams, BH Bendixen, LJ Kappelle, J. Biller, BB Love, DL Gordon: TOAST. Trial of Org 10172 in Acute Stroke Treatment. Classification of subtype of acute ischemic stroke. Definitions for use in multicenter clinical trial. In: Stroke. Mar: 1993: 24, pp. 35-41.
Guidelines:
- S1 guideline for acute therapy of ischemic stroke of the German Society for Neurology . In: AWMF online (as of 09/2012)
- S1 guideline for primary and secondary prevention of cerebral ischemia of the German Society for Neurology. In: AWMF online (as of 10/2008)
- S3 guideline stroke of the German Society of General Medicine and Family Medicine. In: AWMF online (as of 10/2012)
- S2e guideline motor therapies for the upper extremity for the treatment of stroke of the German Society for Neurological Rehabilitation (DGNR). In: AWMF online (as of 2009)
- S3- guideline secondary prophylaxis of ischemic insult of the German Society for Neurology, as of 09/2012.
- WHO definition: Adams et al: Principles of Neurology. 6th edition, pp. 777-810.
Patient guide:
- Trudy Geisseler, Margot Burchert, Daniel Inglin: Hemiplegia. Everyday life is therapy - therapy is everyday life (helping people to help themselves). 4th edition. Springer, Berlin 2004, ISBN 3-540-21221-3 (with photos)
- Günter Krämer : Stroke. What you should know by now. Trias, Stuttgart 1998, ISBN 3-89373-365-5 .
- Katrin Naglo: Hemiplegia after a stroke, head trauma and other brain diseases. A guide for those affected and their families . Schulz-Kirchner, Idstein 2007, ISBN 3-8248-0510-3 .
To the stroke unit:
- Hans-Christoph Diener, Elmar Busch, Martin Grond, Otto Busse (eds.): Stroke-Unit-Manual. 2005, ISBN 3-13-133531-9 .
- Germar Kroczek, Karin Schaumberg, Anke Husberg: Stroke Unit. Pflaum 2002, ISBN 3-7905-0829-2 .
- Michael Laag, Joachim Meyer: Stroke Unit. Huber, Bern 2000, ISBN 3-456-83376-8 .
Experience report:
- Dieter Zimmer : The yellow card. Lübbe, 1996, ISBN 3-404-61361-9 (mild outcome, well written, also funny)
Individual references, footnotes
- ↑ Dirk M. Herrmann: Ischemic stroke. In: Dirk M. Hermann, Thorsten Steiner, Hans C. Diener: Vascular Neurology: Cerebral ischemia, hemorrhage, vascular malformations, vasculitis and vascular dementia. 1st edition. Thieme-Verlag, 2010, ISBN 978-3-13-146111-7 , p. 191.
- ↑ Kolominsky-Rabas 2004
- ↑ a b c d e S. Wolff, K. Nedeltchev: Causes and basic types of cerebral infarcts. Psychiatry & Neurology No. 3. 2010, pp. 3–6, PDF version
- ↑ Cerebral circulatory disorders: Ischemic infarcts. In: W. Hacke: Neurology . Springer-Verlag 2010, 13th edition, ISBN 978-3-642-12381-8 , p. 172.
- ↑ a b Cerebral circulatory disorders: Ischemic infarcts. In: W. Hacke: Neurology . Springer-Verlag 2010, 13th edition, ISBN 978-3-642-12381-8 , p. 181.
- ↑ Dirk M. Herrmann: Ischemic stroke. In: Dirk M. Hermann, Thorsten Steiner, Hans C. Diener: Vascular Neurology: Cerebral ischemia, hemorrhage, vascular malformations, vasculitis and vascular dementia. 1st edition. Thieme-Verlag, 2010, ISBN 978-3-13-146111-7 , p. 193.
- ^ Hankey 2003.
- ^ Clearing report "German guidelines on stroke", 2005. Main document (PDF; 946 kB)
- ↑ Hamann, 2002.
- ↑ E. Bernd Ringelstein, Darius G. Nabavi: The ischemic stroke. A practice-oriented presentation of pathophysiology, diagnostics and therapy. W. Kohlhammer Verlag, 2007, ISBN 978-3-17-018853-2 , pp. 20-25.
- ↑ In such a specialized medicine. Supply unit, e.g. B. that of the Heidelberg University Hospital , over a thousand (HD 2006: 1,400 people, length of stay on average 4 days) treatments are initiated. No more than 15 to 30 minutes should elapse between admission and a first CT. Maria Stumpf: Guide. Interview with W. Hacke . RNZ, July 13, 2007, p. 3.
- ^ MG Lansberg et al. Efficacy and safety of tissue plasminogen activator 3 to 4.5 hours after acute ischemic stroke: a metaanalysis. In: Stroke. 2009 Jul; 40 (7), pp. 2438-2441.
- ↑ W. Hacke et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. In: N Engl J Med. 2008 Sep 25; 359 (13), pp. 1317-1329)
- ↑ M. Koehrmann et al. Thrombolysis in ischemic stroke: An update. In: Neurologist. 2007, 78, pp. 393-405.
- ↑ Manio of Maravic: Neurological emergencies. In: Jörg Braun, Roland Preuss (Ed.): Clinic Guide Intensive Care Medicine. 9th edition. Elsevier, Munich 2016, ISBN 978-3-437-23763-8 , pp. 311-356, here: pp. 319 f. ( Stroke Unit: Acute Therapy ).
- ↑ a b Werner Hacke among others: Acute therapy of ischemic stroke . Guideline of the German Society for Neurology (DGN) and the German Stroke Society (DSG) in the German Society for Neurology, status October 2008, update of the online version in May 2009, PDF version (last accessed on October 8, 2011).
- ^ The preclinical administration of oxygen part 2: The apoplectic insult. January 18, 2012, accessed February 16, 2012 .
- ↑ Manio von Maravic (2016), p. 320.
- ↑ a b Dirk M. Herrmann: Ischemic stroke. In: Dirk M. Hermann, Thorsten Steiner, Hans C. Diener: Vascular Neurology: Cerebral ischemia, hemorrhage, vascular malformations, vasculitis and vascular dementia. 1st edition. Thieme-Verlag, 2010, ISBN 978-3-13-146111-7 , p. 202.
- ↑ P. Ringleb, PD Schellinger, W. Hacke: Guidelines for Management of Ischaemic Stroke and Transient Ischaemic Attack 2008 Guidelines of the European Stroke Organization (ESO), as of March 16, 2008. PDF version ( Memento of the original from January 31 2012 in the Internet Archive ) Info: The archive link was automatically inserted and not yet checked. Please check the original and archive link according to the instructions and then remove this notice. (last accessed October 8, 2011).
- ↑ K. Vahedi, J. Hofmeijer u. a .: Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomized controlled trials. In: The Lancet Neurology . Volume 6, Number 3, March 2007, pp. 215-222, ISSN 1474-4422 . doi: 10.1016 / S1474-4422 (07) 70036-4 . PMID 17303527 .
- ↑ Acute diagnosis and therapy for cerebral ischemia Early decompression surgery for malignant media infarction - pooled analysis of three randomized controlled studies. (No longer available online.) German Stroke Society, 2010, archived from the original on August 29, 2014 ; Retrieved June 11, 2014 .
- ↑ E. Jüttler, A. Unterberg u. a .: Hemicraniectomy in older patients with extensive middle-cerebral-artery stroke. In: The New England Journal of Medicine . Volume 370, Number 12, March 2014, pp. 1091-1100, ISSN 1533-4406 . doi: 10.1056 / NEJMoa1311367 . PMID 24645942 .
- ↑ In the case of a stroke, opening the skull saves the lives of older people. Joint press release of the German Stroke Society (DSG), the German Society for Neurology (DGN) and the German Society for Neurosurgery (DGNC), April 14, 2014, accessed on June 11, 2014 .
- ↑ Kolominsky-Rabas 2004.
- ^ Hankey 2003.