thrombosis
| Classification according to ICD-10 | |
|---|---|
| I80.– | Thrombosis, phlebitis and thrombophlebitis |
| ICD-10 online (WHO version 2019) | |
A thrombosis (derived from " thrombus " or thrombosis ) is a vascular disease or disorder of the circulatory system in which a blood clot (thrombus, blood clot) forms (intravitally) in a blood vessel . Thromboses can occur in all vessels. Most often it is a thrombosis of the veins ( venous thrombosis or phlebothrombosis ), especially a thrombosis of the deep leg veins ( deep vein thrombosis - DVT). In contrast to deep, i.e. non-superficial, vein thromboses, superficial vein thromboses have a different appearance with an inflammatory component (see thrombophlebitis ).
In pregnancy , a venous thrombosis is a common complication and is different from the other forms ( see below ).
Peripheral deep vein thrombosis is treated below. For the much rarer thromboses of the arteries see arterial thrombosis , those of the sinus veins in the brain see sinus thrombosis .
The term “thrombosis” was coined by Galen in the 2nd century and established in the German language by Rudolf Virchow around 1845 .
Emergence
A thrombus is caused by blood clotting - a process that is actually a protective mechanism: after an injury, the coagulation system protects the body from bleeding to death. This means that the blood clumps and closes the wound. In contrast to the coagulation system, the blood in the uninjured blood vessels should not clump, but rather flow freely. Here a clot is a disruptive obstacle to the blood flow, causes a thromboembolism and is dangerous as a trigger for a pulmonary embolism . If the blood's natural ability to coagulate increases abnormally, the risk of thrombosis and embolism increases.
causes
There are usually several factors that combine to cause thrombosis. These can be both hereditary and external factors.
The causes of the formation of a venous thrombus are according to the Virchow's triad, which is still valid today :
- Change in blood composition:
- Clotting disorders (hypercoagulability)
- Hereditary increased blood clotting
- Hereditary or medicinally reduced ability to dissolve blood clots (see fibrinolysis ), such as:
- Certain foods, drugs, or toxins that affect blood clotting, such as birth control pills , especially third and fourth generation micro pills .
- pregnancy
- Dehydration (increased blood viscosity )
- Antiphospholipid Syndrome
- Reduced blood flow velocity ( stasis , immobilization , hypocirculation):
- Dilated veins (varices) and varicose veins
- Limbs trapped by external pressure
- Inability to move caused by being bedridden (including after operations or in a cast)
- Sitting for a long time - especially at an angle in the knee - with restricted mobility (e.g. when traveling by bus or plane) if the risk factors mentioned below are present
- Damage to the inner vessel walls ( endothelium ):
- Damage of a traumatic nature (injuries, bruises, operations)
- Degenerative changes (for example, age-related)
- Inflammatory changes in the veins
- Diabetes mellitus
- Hypoxic vascular wall damage caused by carbon monoxide (smoking)
- Tumor infiltrates
- Operations
Risk factors
- Lack of exercise, especially long lying down when sick
- Obesity
- Lack of fluids ( desiccosis )
- Unusual intense physical exertion (thrombosis par effort)
- Hormonal contraceptives (“pill”), rarely complications, increasingly with obesity and smoking
- Past thrombosis
- Smoke
- pregnancy
- Cancers
- chemotherapy
- Intravenous drug use (e.g. heroin ) through damage to blood vessels
- height
Clinical appearance
Depending on the location and extent of the thrombosis, the symptoms can be very different. Many thromboses go unnoticed by those affected. Diagnostically it is particularly critical that even severe thromboses that later lead to life-threatening pulmonary embolism can be almost symptom-free in the initial stage and therefore often remain undetected.
Typical are, at least with pronounced venous thrombosis:
- Swelling and sensation of warmth on the ankle, lower leg or whole leg with a feeling of tension
- Reddened and tight skin, possibly blue
- Feeling of tension and pain in the foot, calf and hollow of the knee (relief when lying up)
- Overheating of the swollen leg
localization
The legs are most commonly affected by deep vein thrombosis. One then speaks of calf vein or leg vein thrombosis . If both the calf, the hollow of the knee and the thigh are affected, this is called a multi-tier thrombosis. A pelvic vein thrombosis is rare in contrast, but more dangerous because of the size of the vessel and the higher pulmonary embolism risk. Pelvic vein thrombosis is feared in pregnant women, in which a clot can loosen after birth due to the lack of compression of the uterus and lead to pulmonary embolism.
Superficial phlebitis, thrombophlebitis, must be differentiated from deep vein thrombosis . It is also found most often on the legs, but has to be considered separately due to its completely different prognosis. Thromboses on the arms and in the shoulder area are significantly less common than on the lower extremities. However, a distinction must also be made here between deep thrombosis and superficial phlebitis. Thromboses on the arm are not infrequently caused by venous catheters , whereas the infused solutions can lead to phlebitis through direct irritation of the venous wall .
If all veins of a cross-section of the extremity are thrombotically closed, one speaks of phlegmasia caerulea dolens - a very rare and particularly severe form of venous thrombosis with the risk of death of the affected extremity.
Complications
The most important complication of fresh deep vein thrombosis is pulmonary embolism , which can be fatal under certain circumstances. Because of the risk of pulmonary embolism, any suspicion of deep vein thrombosis should be clarified immediately. The most important late complication of deep vein thrombosis is post-thrombotic syndrome .
Investigation methods
Clinical Findings
There is no definite evidence of leg vein thrombosis. Many patients only complain of diffuse, not very pronounced symptoms in the affected leg. This applies above all to thromboses that are (still) limited to the lower leg at the time of the examination and those that are (still) short. Extensive thrombosis typically (but not always) results in pain and swelling of the affected extremity with a (significant) difference in circumference and (clearly) compressible edema . Pelvic vein thrombosis can very rarely cause swelling in both legs.
Further signs of thrombosis, which are not conclusive but characteristic, are pressure pain on the sole of the foot ( Payr sign ) of the affected leg and in the course of the veins.
A scoring system to increase the probability of a diagnosis is the system according to Wells et al. (see table).
| Clinical characteristics | Score |
|---|---|
| active cancer | 1 |
| Paralysis or recent immobilization of the legs | 1 |
| Bed rest for three days or major surgery in the past twelve weeks | 1 |
| Pain / induration along the deep veins | 1 |
| Swelling of the whole leg | 1 |
| Increased circumference of the lower leg to the opposite side> 3 cm | 1 |
| Impressible edema | 1 |
| visible collateral veins | 1 |
| previous deep vein thrombosis | 1 |
| alternative diagnosis as likely as DVT | −2 |
|
Score> 2 : probability of DVT high
Score <2 : probability of DVT not high |
|
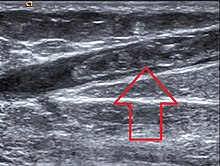
Technical findings
Today, the diagnosis of venous thrombosis is usually made using sonography (Doppler and duplex sonography). If this is not available or if there are still uncertainties about how to proceed after the ultrasound examination, phlebography ( X-ray examination with contrast agent ) is used. If a modern ultrasound device is available and the examiner is sufficiently experienced, the more complex and more stressful venography only rarely has to be used.
Laboratory chemistry
Fibrin breakdown products as a breakdown product of thrombi can be detected in the blood with a D-dimer test. With a sensitivity of 95%, a negative D-dimer test with a low or medium risk score according to Wells makes it possible to rule out the presence of a deep vein thrombosis with sufficient certainty. The specificity, on the other hand, is low, so that increased D-dimers are in no way sufficient as evidence of a thrombosis.
For prophylaxis, the most important congenital coagulation disorders can be examined, which affect more than 5% of the population. These include a mutation in the factor V gene, a mutation in the factor II gene, protein C deficiency, protein S deficiency and antithrombin deficiency.
Differential diagnosis
Various diseases have a similar appearance and are considered as differential diagnoses - such as thrombophlebitis , which is an inflammatory disease of the superficial veins, lymphedema and edema, and cellulitis ; But also the Baker cyst , enlarged lymph nodes or a hematoma can cause symptoms comparable to a thrombosis.
therapy
The surgical removal of venous thrombi is reserved for special cases.
Medication
In order to prevent the thrombus from enlarging, the aim is to inhibit blood clotting ( anticoagulation ). Initially, heparin preparations or factor Xa inhibitors are used. Once the clot has stopped growing, the body can begin cleaning up the damage. He breaks down the clot and tries to clear the veins again. This takes a few weeks to months - the more sections of the venous system were affected, the longer. During the breakdown of the clot and the regeneration of the veins, substances are released that increase the coagulability of the blood. During this time, the risk of a new thrombosis is particularly great. Therefore, anticoagulant drugs must continue to be taken. Then 4-hydroxycoumarins - such as phenprocoumon , warfarin or ethylbiscoum acetate - are used for about three to six months. The intake of coumarins requires regular blood tests and special attention, because the drugs prevent thrombosis, but also increase the willingness to bleed. In most cases, tablet-taking can be stopped after three to six months. If the risk factors persist, the risk of thrombosis also remains; the patient also suffers a new thrombosis or coagulation disorder; in both cases the medication may have to be given for life.
In recent years, drugs have been developed which, like coumarin derivatives, can be taken as tablets, but which do not require the coagulation values to be checked. Some of them have already been approved and are used in hospitals to prevent thrombosis or pulmonary embolism. The most recent study results (Re-Cover, Einstein-Extension-Study, Calisto-Study) are very promising and show that these new drugs can also be used to treat a leg vein thrombosis or pulmonary embolism. Once approved by the authorities, these drugs will make life with anticoagulants much easier and, in certain areas of application, even more effective or safer.
Drug dissolution ( thrombolysis ), which was still used more frequently in the 1990s, is only used in exceptional cases in the case of venous thrombosis, because there is a higher risk of bleeding.
compression
Furthermore, the legs are wrapped with compression bandages or supported by a special medical compression stocking to prevent the thrombus from growing further. The compression speeds up blood flow in the deep veins and reduces or prevents the redistribution of blood from the deep veins to the superficial veins. This also speeds up blood flow in the deep veins.
Mobilization
For fear of a pulmonary embolism , immobilization of the patient used to be the top priority. The patients were admitted to the hospital and usually had to stay in bed for at least 14 days. Even touching the affected leg was avoided in order not to mechanically loosen the thrombus. Today, patients with lower and thigh vein thrombosis are usually no longer immobilized and are no longer treated as inpatients. Mobilization with adequate compression prevents stasis (standstill of the blood in the vessel), which is one of the three main triggering factors for thrombus formation and for thrombus growth (see Virchow's triad ). In the case of extensive leg vein thromboses and most recent pelvic vein thromboses, mobilization is not possible due to pain. In the case of pelvic vein thrombosis, there is also the fact that adequate compression is not possible. These cases are still treated as inpatients today. The mobilization takes place according to the complaints.
Aftercare
The so-called post - thrombotic syndrome (PTS) can result from deep thrombosis . Veins affected by thrombi can remain closed, and the bypass circuits that are formed, which are mostly closer to the surface, can expand like varicose veins. Very often venous valves are destroyed or their function is restricted by scarring, which leads to increased blood backflow in the direction of gravity . The chronic excess of blood causes the vessels in the affected limbs to dilate excessively. These physical factors can be measured during an examination by a specialist (phlebologist).
The patient can delay the onset of PTS or reduce its effects by:
- Lots of movement of the affected limbs, which promotes the return of blood through the muscle pump . With a given physical condition, this can definitely be (competitive) sport, with sports and equipment that do not allow a vertical posture to be preferred ( swimming , cycling, especially recumbent bikes )
- Continuous compression of the affected limb (s) with the help of compression stockings or tights to compensate for the increased fluid pressure in the tissue and to increase the flow rate of the blood
- Avoiding sitting or standing for hours or regularly interrupting it through " vein gymnastics "
"Vein-strengthening" drugs offered in the trade - often horse chestnut based - may be effective for minor venous problems, but not for existing varicose veins or other symptoms of post-thrombotic syndrome.
Aftercare also especially at first appearance, to estimate the part, recurrence risk of exclusion of Factor V Leiden , a prothrombin , an antithrombin III deficiency, determining the Methylfolates in the erythrocytes, and a protein C or protein -S deficiency .
Vascular replacement for closed or destroyed veins is very difficult due to the tissue structure of veins and only possible and necessary in exceptional cases.
prevention
The most important measure to prevent thrombosis is exercise. It can be carried out passively or actively, as the muscle activity (such as the legs) supports the venous return ( muscle pump ). If movement is not possible (e.g. after an operation), medical thrombosis prophylaxis stockings should be used if risk factors are present. They support the veins by increasing external tissue pressure, which accelerates the return of blood. Contraindications for preventive measures through physiotherapy are pronounced edema (water retention in the legs), a fresh thrombosis or embolism as well as pronounced pain symptoms (for example suddenly occurring, pulling or cramp-like pain, similar to a sore muscles).
On long-distance trips you should get up as often as possible, move your legs, drink a lot and avoid coffee , tea or alcohol (“dehydration”). People with an increased risk of leg vein thrombosis can wear compression stockings and use anticoagulants, especially heparin , which can be injected by the doctor if prescribed. According to an S3 guideline of the AWMF from 2009, the intake of acetylsalicylic acid (ASA) does not make sense. However, more recent studies such as the WARFASA and ASPIRE studies sometimes come to a different assessment. ASA , which is very effective in arterial diseases, also has an effect, albeit a small one, in the venous limb of the vascular system. In addition, these more recent studies also show that ASA can significantly reduce the risk of venous thrombosis after major orthopedic interventions such as knee or hip joint operations or after bone fractures. For long-term drug prophylaxis , oral anticoagulants of the coumarin type , e.g. B. Marcumar , another alternative.
Pregnancy-associated deep vein thrombosis
This is a special form and one of the most common complications in pregnancy. It occurs in one to two pregnancies per thousand and is found predominantly on the left leg (85% versus 55% otherwise), and much more often proximally , i.e. located in the pelvis or thigh (72% versus 9% otherwise) instead of distally in the Lower legs, with a correspondingly significantly increased risk of pulmonary embolism and post-thrombotic syndrome. More than half of all pregnancy-associated leg vein thromboses occur within the first twenty weeks of pregnancy, but the risk is increased until twelve weeks after giving birth. Risk factors are an increased body mass index , vomiting during pregnancy and a lack of exercise. The risk of leg vein thrombosis during the puerperium is increased after a caesarean section . The risk of recurrence when pregnant again is six to nine percent.
Since the D-dimer is usually increased during pregnancy, it is not suitable for diagnosing thrombosis.
In addition to unfractionated heparin, low molecular weight heparins, which do not cross the placenta and do not get into breast milk, are used for therapy. In contrast, vitamin K antagonists such as Marcumar cross the placenta and are teratogenic with a typical embryopathy and are therefore contraindicated in pregnancy. However, since they do not get into breast milk, they can be used after birth.
World Thrombosis Day
The October 13, 2014 was organized by the International Society on Thrombosis and Hemostasis ( International Society on Thrombosis and Haemostasis , ISTH) for the first world-thrombosis day ( English World Thrombosis Day proclaimed WTD). The German Society for Angiology - Society for Vascular Medicine took part in the campaign.
The information day is intended to draw attention to the importance of a timely diagnosis and treatment of thrombosis and is repeated annually on October 13th. The date was chosen in honor of Rudolf Virchow , who was born on October 13, 1821.
Body size as a risk factor
A large study of two cohorts of more than two million Swedish people included suggests that taller people are at increased risk of developing blood clots, while smaller people are less prone to it.
The men were observed from the time they were mustered (1969 to 2010) until 2012, while the women were observed from their first pregnancy (1982 to 2012) until 2012. Men who were less than 160 cm tall had a 65 percent lower risk of developing venous thromboembolism than men who were 190 cm or taller ( hazard ratio 0.35, 95% - confidence interval 0.22-0.55 ). Women who were shorter than 155 cm had an approximately 69 percent lower risk than women who were 185 cm or taller (hazard ratio 0.31, 95% confidence interval 0.22-0.42). This effect was also shown in comparison with siblings who had different body sizes, with a hazard ratio per 10 cm difference of 0.69 for brothers and 0.65 for sisters. The author speculates that this could be due to the longer leg veins, which had a larger surface, and that the greater pressure gradient increases the risk that the blood flow will be slowed down or stop in the meantime.
See also
- Peripheral arterial occlusive disease (PAOD) or intermittent claudication
- Thrombosis tendency: thrombophilia
- Thrombosis stocking
Professional associations
- German Society for Angiology - Society for Vascular Medicine e. V.
- German Society for Vascular Surgery and Vascular Medicine e. V.
- Society for Thrombosis and Hemostasis Research (GTH)
Trade journal
Different types of thrombosis
- "Arm vein thrombosis": Paget-von-Schroetter syndrome
- Cerebral vein thrombosis
- Jugular vein thrombosis
- Mesenteric vein thrombosis
- Renal vein thrombosis
- Superficial thrombophlebitis
- Perianal thrombosis - a blood clot in the external veins of the anus that is generally not life threatening
- Portal vein thrombosis
- Phlegmasia alba dolens
- Sinus thrombosis
literature
- Christin Mpliatis: Polymorphisms of the blood coagulation system and the risk of thrombosis. Individualized thrombosis prophylaxis. Dissertation at the University of Greifswald 2011.
- C. Kearon, EA Akl et al .: Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. In: Chest. Volume 141, Number 2 Suppl, February 2012, pp. E419S – e494S, ISSN 1931-3543 . doi: 10.1378 / chest.11-2301 . PMID 22315268 . PMC 3278049 (free full text).
- S2 guideline for venous thrombosis and pulmonary embolism: Diagnostics and therapy of the German Society for Angiology - Society for Vascular Medicine e. V. (DGA). In: AWMF online (as of June 1, 2010)
- S3 guideline AWMF guideline prophylaxis of venous thromboembolism (VTE) of Arbeitsgem. the scientist Medicine. Professional societies (AWMF). In: AWMF online (as of May 1, 2010)
Web links
Individual evidence
- ^ Heinz Otremba: Rudolf Virchow. Founder of cellular pathology. A documentation. Echter-Verlag, Würzburg 1991, p. 22 f.
- ↑ thrombosis. In: Digital dictionary of the German language . Retrieved August 15, 2019
- ↑ Thrombosis - Prevent and Treat . ( Memento from September 25, 2013 in the Internet Archive ) (PDF; 701 kB) German Society for Angiology - Society for Vascular Medicine e. V. 2011.
- ↑ a b c d IGeL - Services (August 2006): Thrombosen - Travel Thromboses ( Memento from February 10, 2008 in the Internet Archive ) labor28.de, accessed on May 13, 2013, archived from the original.
- ↑ a b c LADR : Free path! Thrombosis prophylaxis (PDF)
- ↑ Annika Joeres : Thrombosis Risk: The Pill of Unreason . In: Die Zeit , No. 5/2013
- ↑ M. Sand et al .: Surgical and medical emergencies on board European aircraft: a retrospective study of 10189 cases (PDF; 95 kB). In: Critical Care , 2009 Jan 20; 13 (1), p. R3.
- ↑ Birth control pills: How high is the risk of thrombosis? Doctors newspaper, October 27, 2014, accessed December 6, 2018
- ↑ Taller people may be more susceptible to blood clots . In: Medical News Today . ( medicalnewstoday.com [accessed September 6, 2017]).
- ↑ H. Schinzel, M. Hendelmeier: Therapy of deep vein thrombosis. German Med. Wochenschrift 2013, 138; Pp. 786-791, Georg-Thieme Verlag.
- ^ PS Wells et al .: Accuracy of clinical assessment of deep-vein thrombosis. In: The Lancet , 1995, 345, pp. 1326-1330.
- ↑ eva.unibas.ch (PDF) p. 2, table below left.
- ↑ Abigail Thrush, Tim Hartshorne: Vascular Ultrasound. How, Why and When . 2011, ISBN 978-0-443-06918-5 , pp. 246-249.
- ↑ German Society for Angiology - Society for Vascular Medicine e. V.
- ↑ Living with Blood Thinners - Anticoagulant Drugs (press release). (PDF; 29 kB) German Society for Angiology - Society for Vascular Medicine e. V. (DGA), archived from the original on October 5, 2013 ; accessed on September 6, 2014 .
- ↑ Vine leaves and butcher's broom root against varicose veins - studies show that herbal ingredients can help with venous diseases
- ^ S1 guideline for diagnosis and therapy of deep leg and pelvic vein thrombosis . In: AWMF online
- ↑ AWMF guideline on prophylaxis of venous thromboembolism (VTE). Retrieved May 20, 2015 .
- ↑ Does ASA protect against recurrence of thrombosis? Medical Tribune, accessed July 16, 2015 .
- ↑ ASA reduces the number of venous thromboses
- ^ Ian A. Greer: Pregnancy complicated by venous thrombosis New England Journal of Medicine 2015, Volume 373, Issue 6 of August 6, 2015, pp. 540-547, doi: 10.1056 / NEJMcp1407434
- ↑ International Society on Thrombosis and Haemostasis. Retrieved September 6, 2017 .
- ↑ World Thrombosis Day | Home. Retrieved September 6, 2017 .
- ↑ DGA participates in World Thrombosis Day . dga-gefaessmedizin.de
- ↑ Bengt Zöller, Jianguang Ji, Jan Sundquist, Kristina Sundquist: Body Height and Incident Risk of Venous Thromboembolism. Clinical Perspective: A Cosibling Design . In: Circulation: Cardiovascular Genetics . tape 10 , no. 5 , September 5, 2017, ISSN 1942-325X , p. e001651 , doi : 10.1161 / CIRCGENETICS.116.001651 ( ahajournals.org [accessed September 6, 2017]).

