Hydrocele
| Classification according to ICD-10 | |
|---|---|
| P83.5 | congenital hydrocele |
| N43.1 | infected hydrocele |
| N43.2 | other hydrocele |
| N43.3 | Hydrocele, unspecified |
| ICD-10 online (WHO version 2019) | |
The accumulation of serous fluid around the testicle (in the scrotal compartment ) is referred to as a hydrocele or water fracture (from ancient Greek ὕδωρ, ὕδατος hydor, hydatos , German 'water' and κήλη , break) . A hydrocele can be unilateral or bilateral.
Must be distinguished is an edema with fluid accumulation in the Skrotalhüllen.
to form
According to the localization of the fluid, a distinction can be made:
- Hydrocele testis , fluid around the testicle
- Hydrocele funiculi , fluid along the spermatic cord
- Hydrocele vaginalis communicans , fluid also along the spermatic cord in the abdomen
- Hydrocele multilocularis , fluid in several of the named places
Emergence
A hydrocele can be congenital or acquired.
Congenital hydrocele
A congenital hydrocele is an incomplete obstruction ( obliteration ) of the processus vaginalis testis . It is a finger-shaped protuberance of the peritoneum that accompanies the testicle on its migration - the Descensus testis - from the abdominal cavity into the scrotum . The processus vaginalis usually obliterates soon after the testicle has reached the scrotum - with the exception of the area adjacent to the testicle, which surrounds it as the tunica vaginalis testis or the serous testicular membrane. If not sclerosing, it communicates with the abdomen and fills with fluid. There can also be a prolapse of the intestine into the open process, which is then referred to as an indirect hernia .
Acquired hydrocele
The genesis of an acquired hydrocele has not yet been clarified in detail. Inflammation of the testicle, epididymis and spermatic cord as well as blunt violence play a role here.
Diagnosis
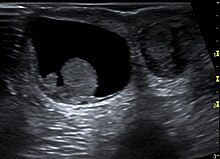
In addition to the physical examination with inspection and palpation , a reliable differentiation of testicular tumors , bruises and elephantiasis is possible using ultrasound, among other things .
The previously used diaphanoscopy , in which a cold light source is placed on the scrotum, only plays a subordinate role in diagnostics.
therapy
A congenital hydrocele is usually treated surgically, as there is a risk of an intestinal prolapse ( hernia ) with the complication of entrapment. The open vaginal process is removed and closed on the inner inguinal ring . However, if the hydrocele are less pronounced, surgery does not need to be carried out, as the disease is benign and in normal-sized testes there is no tendency towards a malignant course. In some patients, the hydrocele partially regresses over time.
Acquired hydroceles can be surgically removed if they cause discomfort or are a nuisance due to their size. The removal of a water fracture is called hydrocele ablation, whereby different surgical techniques can be used depending on the location. An inguinal or scrotal incision provides surgical access. During the operation, the testicular envelopes are removed (OP according to von Bergmann ) or turned over (OP according to Winkelmann / Jaboulay and OP according to Lord).
A puncture usually shows no long-term success. However, healing (by self-sticking of the protein-containing fracture) can also take place after several punctures without surgery.
Web links
Individual evidence
- ^ W. Pschyrembel: Clinical dictionary. 265th edition. Verlag Walter de Gruyter, Berlin 2014, ISBN 978-3-11-018534-8 .
- ^ V. Hofmann, KH Deeg, PF Hoyer: Ultrasound diagnostics in paediatrics and pediatric surgery. Textbook and atlas. Thieme, Stuttgart 2005, ISBN 3-13-100953-5 .
- ↑ M. Bettex, N. Genton, M. Stockmann (Ed.): Pediatric surgery. Diagnostics, indication, therapy, prognosis. 2nd edition, Thieme 1982, p. 7 ff., ISBN 978-3-642-11330-7
- ↑ JW Thüroff, H. Schulte-Wissermann (editor): Pediatric urology in clinic and practice. , 2nd edition 2000, Thieme, p. 501 ff., ISBN 3-13-674802-6