Hypoplastic left heart syndrome
| Classification according to ICD-10 | |
|---|---|
| Q23.4 | Hypoplastic left heart syndrome |
| ICD-10 online (WHO version 2019) | |
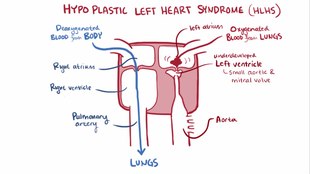
When hypoplastic left heart syndrome ( HLHS ), also Linksherzhypoplasie syndrome called ( hypoplastic = too small, underdeveloped ), is more associated with each occurring malformations of the heart and the connected main artery ( aorta ). The hypoplastic left heart is characterized by a complete ductus dependence (i.e. the blood flow through a small vascular connection, the ductus arteriosus Botalli). The reasons for this are:
- a high-grade aortic valve stenosis or aortic valve atresia (narrowing or absence / closure of a heart valve between aorta and left ventricle = ventricle )
- and / or mitral valve stenosis or mitral valve atresia (narrowing or absence / closure of the valve between the left atrium and the left main chamber)
- with severe hypoplasia (= underdevelopment) of the ascending aorta (the ascending part of the large body artery from which the coronary arteries arise) (2-4 mm, normally 10-12 mm) in type I
- and in type II (different appearance of the heart defect in different forms) with normal diameter of the ascending aorta
- and very small (hypoplastic) or missing left ventricle (which cannot develop in the first place due to the mitral valve malformation)
- and often simultaneously present hypoplastic left atrium = atrium
Endocardial fibrosis (thickening of the heart wall without functional benefit) of the left ventricle and atrium can also occur regularly. Usually the ventricular septum (heart septum at the ventricular level) is intact, while an open foramen ovale (= opening between the right and left atrium, which due to its appearance is called foramen ovale (= "oval hole")) or a real atrial septal defect (ASD) allows the pulmonary venous blood (flowing from the pulmonary vein) to flow out of the left atrium into the right atrium. In up to 20% of cases there is a preductal aortic coarctation (= narrowing of the aorta in front of the confluence of the ductus arteriosus). The right heart structures are usually enlarged in a compensatory manner (enlargement / hypertrophy of the right atrium and ventricle).
Physical processes / pathophysiology
In contrast to the regular blood flow of a properly developed heart, in HLHS the blood from the pulmonary veins initially flows through the left atrium. The existing atrial gap (foramen ovale), which ensures the child's survival, allows the blood to mix with non-oxygenated blood via the right atrium. This is called medically a left-right shunt . The mixed blood then flows from the right ventricle into the pulmonary artery and further via the Ductus arteriosus Botalli back into the descending aorta (descending part of the aorta, further divided into the thoracic aorta and the abdominal aorta ). At the same time, blood flows through the open ductus arteriosus against the normal direction of flow into the (underdeveloped) ascending aorta (part of the aorta from which the coronary arteries arise) and thus into the coronary arteries. This process is called “retrograde perfusion”.
Children with this clinical picture are also referred to as "blue babies".
treatment

If a diagnosis of hypoplastic left heart syndrome has been confirmed, there are now various approaches to treatment:
- the child is left to the so-called "natural course" without medical or surgical care. This means that it usually dies within a few days or hours, only in exceptional cases within a few weeks.
- the 3-step surgical palliation.
- classic Norwood operation , also known as the Norwood procedure
- This surgical technique initially includes a first life-sustaining operation, the Norwood Stage1 operation, in which the underdeveloped aorta is widened using a plastic patch. For this purpose, the right ventricle is connected to the aorta at the same time during this operation and a shunt (= plastic tube) is placed for the pulmonary blood flow. This operation is carried out using the heart-lung machine and in a state of cardiac arrest.
- The Norwood Stage2 operation, also known as the Glenn anastomosis (or " Hemi-Fontan "), connects the superior vena cava with the pulmonary artery. This operation gives the child a safer living situation because the shunt from the first operation can now be removed. Treatment with anticoagulant drugs - such as coumarins - is no longer necessary in most cases.
- Norwood Stage3 operation = complete Fontan (TCPC): In this operation step, the inferior vena cava is also connected to the pulmonary artery, so that a complete separation of the circulation is achieved.
- alternatively the casting procedure (hybrid operating room)
- This is a so-called hybrid procedure by pediatric heart surgeons and pediatric cardiologists. First, a stent is inserted into the ductus arteriosus by catheter intervention to ensure the perfusion of the body's circulation. The pulmonary arteries are then surgically tied on both sides to restrict the pulmonary blood flow. The operation can initially take place without a heart-lung machine.
- In the course of the Norwood stage 2 operation with reconstruction of the underdeveloped aorta (see above).
- classic Norwood operation , also known as the Norwood procedure
- as a rare last resort: a heart transplant
forecast
Although the HLHS is certainly a serious cardiac malformation complex, the experience of the last few years shows that the treatment of this heart defect now offers good treatment prospects in the specialized heart centers. Experience from America shows that there are already adults who were once born with HLHS and who received a good to very good quality of life through the Norwood procedure. In America, the HLHS is no longer a mandatory indication for an abortion. On the contrary, there is even an obligation to treat children with this malformation, since with adequate treatment these children can be helped to lead a normal life with a good quality of life.
The different perspectives between Germany and America also stem from the fact that z. In part, the figures from the beginnings of this surgical technique in Germany are still included in the mortality rates, which thus show a falsified picture of today's reality. Thanks to the use of experienced pediatric cardiac surgeons, improved surgical techniques and refined examination methods, a large proportion of the children who are operated on today have much better long-term prognoses than at the beginning of this surgical technique in the 1980s. The last option is the possibility of a heart transplant, which can now be carried out with good results. There are therefore various treatment approaches for the HLHS that give the child the opportunity to lead a fulfilled life with a good quality of life.
Back to heart defect descriptions
literature
- JA Connor, R. Thiagarajan: Hypoplastic left heart syndrome. In: Orphanet Journal of Rare Diseases. Volume 2, 2007, p. 23, ISSN 1750-1172 . doi: 10.1186 / 1750-1172-2-23 . PMID 17498282 . PMC 1877799 (free full text). (Review).
- S2k guidelines for hypoplastic left heart syndrome (HLHS) of the German Society for Pediatric Cardiology (DGPK). In: AWMF online (as of 2013)
- Parents information brochure from the Bundesverband Herzkranker Kinder BVHK e. V .: HLHS guidelines and the univentricular heart as of 03/2013
Web links
- Children's Heart Center Kiel on the topic
- Hypoplastic Hearts Germany e. V. on the subject
- Animated heart defect description HLHS
- Declaration by the Fördergemeinschaft Deutsche Kinderherzzentren e. V.
Individual evidence
- ↑ Hakan Akintürk, Ina Michel-Behnke, Klaus Valeske, Matthias Mueller, Josef Thul: Hybrid Transcatheter-Surgical Palliation . In: Pediatric Cardiology . tape 28 , no. 2 , April 1, 2007, ISSN 1432-1971 , p. 79-87 , doi : 10.1007 / s00246-006-1444-7 .