Gastric resection
In medicine, the surgical removal of part of the stomach is called gastric resection , also known as partial gastric resection . The complete removal of the stomach is called a gastrectomy , often called a total gastric resection or total gastrectomy .
Indications
The gastric resection is performed to treat gastric or duodenal ulcers that cannot be treated with drugs (gastric ulcer , duodenal ulcer ). The effect of the resection is a strong reduction in gastric acid production, since the parietal cells responsible for this are mainly located in the lower two thirds of the stomach.
It is also rarely performed in cases of gastric outlet stenosis, i.e. narrowing of the gastric outlet due to scarring, if local endoscopic or surgical therapy with balloon dilation, stenting or pyloroplasty is not possible. It is also used for benign tumors, exceptionally also for gastric cancer , provided that it is limited, is located in the lower third of the stomach and the risk of surgery is too great for a gastrectomy due to accompanying diseases.
Since the beginning of the 1990s, the incidence of therapy-resistant duodenal or gastric ulcers has decreased drastically due to the greatly improved drug treatment ( proton pump blockers , eradication therapy when Helicobacter pylori is detected ), so that gastric resection, which used to be very common, is only rarely required.
Elimination of pain, positioning and access
Today, only intubation anesthesia is used to eliminate pain, which contributes to a good overview of the surgical field due to the possibility of muscle relaxation .
An epidural catheter can be put on for analgesia both before and after surgery .
The patient is supine with the thoracic spine slightly hyperextended. The stomach is accessed via a median or transverse upper abdominal laparotomy .
Operating principle
The gastric resection, developed in the last third of the 19th century, is performed using several different methods, depending on the findings and the indication. These differ in the type of new connection between stomach and duodenum ( Billroth I) or small intestine (Billroth II), both 2/3 resections, and the extent of the resection (4/5 or subtotal resection).
The removal of the distal part of the stomach is carried out in the same way in all three methods. First, the stomach is "skeletonized", that is, cut off from its blood supply by ligating the vessels. The dextra gastric artery and the dextra gastroomental artery (dextra gastroepiploic artery) are severed. The artery gastrolienalis and the artery gastric artery remain blood supply to the rest of the stomach. Then the stomach is detached from its adhesions on the posterior wall ( bursa omentalis ) and set down in the upper third and a little below the gastric gate ( pylorus ). The wide opening of the residual stomach is closed except for a residual opening of about 3 cm.
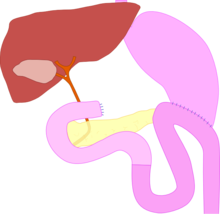
Resection according to Billroth I
After removal of the distal part of the stomach, the stomach stump is connected directly to the open end of the duodenum by an end-to-end anastomosis ( gastroduodenostomia terminoterminalis oralis partialis inferior ). This maintains the physiological food passage.
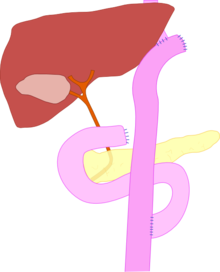
Resection according to Billroth II
After gastric resection, the duodenum is blindly closed and a side-to-end anastomosis is made from the first loop of the small intestine ( jejunum ) and stomach stump ( gastrojejunostomia terminolateralis ante- / retrocolica anterior ), whereby the jejunal loop is ante- or retrocolic (in front of or behind the horizontal part of the colon ) can be pulled up. In order to avoid the continuous contact of the bile and duodenal secretions with the gastric mucosa in the area of the gastrojejunostomy, a laterolateral enteric anastomosis is also applied between the incoming and outgoing small intestine ( Braun's foot point anastomosis; not shown in the picture). This can reduce the rate of recurrent ulcers or anastomotic ulcers.
Distal 4/5 gastric resection
The procedure essentially corresponds to the resection according to Billroth II, but the stomach is separated significantly higher up. A Y-anastomosis according to Roux is often used here as an anastomosis : For this purpose, the small intestine is cut about 20 cm below the Treitz ligament (transition from the duodenum to the jejunum), the discharge end is connected to the stomach stump, the feeding end with an end to-side anastomosis attached to the previously opened small intestine.
Risks and Complications
Nonspecific surgical risks are intra- and postoperative bleeding ( blood reserves must be kept ready), wound healing disorders, formation of incisional hernias , thrombosis , pulmonary embolism and postoperative pneumonia .
Specific early complications are injury to the biliary tract , pancreas , liver, and spleen . Insufficiency of the duodenal stump or anastomotic leakage can lead to peritonitis . Dumping syndrome , sling syndrome and gastric stump carcinoma (after 15–20 years) can occur as late complications .
Dumping syndrome occurs when the stomach ceases to function as a reservoir when eating large amounts of carbohydrate-rich food. In early dumping, the carbohydrates in the small intestine withdraw water from the vascular system, which, together with a stimulation of the parasympathetic nervous system, can lead to a drop in blood pressure and even to a volume shock. Late dumping, on the other hand, occurs about 2 hours after ingestion of excessive insulin secretion, which leads to palpitations and hypoglycaemia. Most of the time, the symptoms go away with getting used to and adjusting your eating habits. Otherwise the intestinal passage must be surgically switched to Billroth I.
There is scientific evidence of exocrine pancreatic insufficiency after (partial) stomach removal. Stool fat excretion and dyspepsia improve with enzyme substitution. In patients with fatty stools after a gastrectomy, substitution with digestive enzymes ( pancreatin , fungal enzymes ) should be used.
See also
literature
- JR Siewert, AH Hölscher, J. Lange et al .: Interventions in benign diseases of the stomach . In: Breitner. Edited by F. Gschnitzer et al .: Surgical Operations Teaching Volume IV: Abdominal Surgery 2 . 2nd Edition. Verlag Urban & Schwarzenberg, Munich / Vienna / Baltimore 1989, ISBN 3-541-14442-4
Individual evidence
- ↑ Helmut Wyklicky: gastrectomy. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 880 f.
- ↑ Gastric carcinoma: "Diagnosis and therapy of adenocarcinomas of the stomach and esophagogastric junction" . (PDF) Oncology Guideline Program, p. 136 ( AWMF Register Number 032-009OL).