Monoclonal gammopathy of unclear significance
| Classification according to ICD-10 | |
|---|---|
| D47.2 | Monoclonal gammopathy |
| ICD-10 online (WHO version 2019) | |
The monoclonal gammopathy of undetermined significance ( MGUS ) is a paraproteinemia and the precursor of a malignant lymphoproliferative disease, z. B. multiple myeloma , Waldenström's disease or amyloidosis . Monoclonal immunoglobulins and / or immunoglobulin components (e.g. free light chains ), which are also referred to as M protein / gradient or paraprotein, are produced. The immunoglobulin isotype can be of the IgG , IgA , IgM , IgD or IgE type , but there can also be exclusively free light chains of the kappa or lambda type.
By definition, MGUS is only a forerunner of a malignant haematological disease because the criteria for such a diagnosis are not met. MGUS is found in a comparatively large proportion of people over the age of 50 (1–3%; corresponding to 4–5 new cases per 100,000 people per year). The incidence increases with age, with men being affected slightly more often than women. MGUS can develop into smoldering multiple myeloma , which is another asymptomatic preliminary stage.
Diagnostic examinations
In order to be able to make the exclusion diagnosis MGUS, various examinations must be carried out. In addition to a basic medical history, this includes various laboratory parameters:
Quantitative and qualitative study of the M protein
If the M protein pattern has not yet been clarified, the following combination can be used to clearly determine the type and concentration of the M protein:
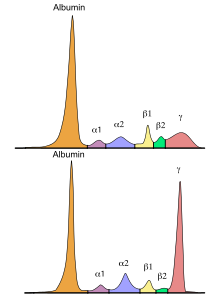
- Serum protein electrophoresis
- Immunofixation electrophoresis (serum and urine)
- Quantitative determination of the free light chains kappa and lambda in the serum including calculation of the quotient (ratio)
Other laboratory parameters
- Blood count including differential blood count
- Electrolytes ( sodium , potassium , calcium )
- Kidney retention parameters ( creatinine including calculated GFR , urea )
- Total protein and albumin in the serum
- Quantitative determination of immunoglobulins (IgG, IgA, IgM)
- Qualitative test for protein in the urine
Diagnostic criteria
Evidence of monoclonal antibody production, as well as:
- M protein <30g / l
- <10% plasma cells in the bone marrow
- no organ damage ( CRAB criteria , from English for Hyper C alcemia ( hypercalcemia ), R enal insufficiency ( renal failure ), A nemia ( anemia ) and B one Lesions ( osteolysis ))
Slightly modified criteria apply to IgM MGUS:
- M protein <30g / l
- <10% lymphoplasmocytic infiltration in the bone marrow
- No evidence of anemia, constitutional symptoms, hyperviscosity syndrome , lymphadenopathy , hepatosplenomegaly, or other organ damage attributable to the lymphoproliferative disease.
Risk factors
Environmental factors
Various environmental factors are discussed as possible risks to the development of MGUS:
- Obesity
- Pesticides
- radiation
- Autoimmune diseases
- Frequent inflammation and infection
Genetic factors
A mutation of the MYD88 gene in B cells from the bone marrow and peripheral blood was detected in around 10% of the cases, as is also the case in Waldenström's disease. Translocations of the immunoglobulin heavy chain (IgH) in the chromosomal areas 4p16, 6p21, 11q13, 16q23 and 20q11 and hyperdiploidy are also considered early changes that contribute to the development of MGUS. Also, people with first-degree relatives who have been shown to have MGUS are at increased risk of developing MGUS.
forecast
| Factors | risk | after 20 years | after 20 years * |
|---|---|---|---|
| 0 | Low | 5% | 2% |
| 1 | Low - medium | 21% | 10% |
| 2 | Medium high | 37% | 18% |
| 3 | High | 58% | 27% |
| * taking into account the average life expectancy | |||
MGUS goes into a further stage with an average probability of about 1 to 1.5% annually. The transition to a symptomatic disease is not necessarily linear, but can also take place suddenly and rapidly after a stable phase. A distinction can be made here between an evolving and non-evolving -MGUS. Therefore, follow-up controls of a once diagnosed MGUS are useful. If there is at least one risk factor, a check-up after 6 months and then annually is recommended. If the laboratory constellation seems stable, there is no risk factor and the patient shows no other evidence of a symptomatic disease, controls are usually recommended after 6 months and then every 2 to 3 years.
The risk of further development (progression) of the MGUS can be estimated on the basis of the following factors:
- abnormal ratio of free light chains
- M protein in serum> 15 g / l
- M protein of the IgA, IgM, IgD or IgE type
For MGUS patients in whom only free light chains are produced (light chain MGUS; LC-MGUS), the risk of progression to a malignant disease is approx. 0.3% per year. However, an impairment of kidney function is observed in almost a quarter of all those affected. A regular check-up (6 months after diagnosis and annually thereafter) is also advisable here. Correspondingly, not only multiple myeloma, which is symptomatic by definition, is now differentiated from the precursor stages, but also so-called monoclonal gammopathy of renal significance (MGRS). Although it does not meet the criteria for multiple myeloma, it is still a malignant disease.
MGUS-associated diseases
MGUS-associated diseases not directly related to M protein
The following diseases occur more frequently in MGUS patients: infections (2-fold), osteoporosis , myeloid diseases (2-8-fold) and thrombosis (2-3-fold). The survival rate of those affected is shorter than that of the normal population (8.1 versus 11.8 years; adjusted for age and gender). A higher risk of death caused by infections, kidney diseases, heart diseases, etc. can be the result of symptomatic manifestations of MGUS.
MGUS-associated diseases related to M protein
Monoclonal proteins can cause severe organ damage through deposition in organs or through autoimmune activity. The following diseases can occur: systemic manifestations (e.g. heart diseases), neurological diseases (e.g. peripheral neuropathy ), hematological diseases, skin diseases, metabolic diseases, kidney diseases (e.g. MGRS).
Secondary MGUS
After treatment of multiple myeloma, monoclonal gammopathies with an altered isotype can occur (secondary MGUS). The incidence is up to 73% after an autologous stem cell transplant and up to 33% in patients without a transplant. A secondary MGUS is not based on the recurrence of the disease, but on the oligoclonal reconstitution of the building up immune system and should not be treated.
Monoclonal gammopathy of renal significance
Due to the potentially nephrotoxic properties of free light chains, symptomatic kidney disease can already occur in the course of MGUS, which is referred to as monoclonal gammopathy of renal significance (MGRS). It is therefore sensible to watch out for complications, both when making the diagnosis and during the course of the disease, which may be caused by deposits of monoclonal proteins in the tissue. Although these diseases are rare, they can be associated with significant morbidity and justify haematological therapy from a nephrological point of view.
treatment
By definition, MGUS is not a malignant disease that requires treatment. Treatment from a hematological point of view is only indicated when symptoms develop in the form of organ damage (e.g. CRAB criteria). In MGUS-associated diseases, palliative therapy is necessary, which in certain cases (such as MGRS) can also include hematological-oncological therapy.
literature
- SV Rajkumar, A. Dispenzieri, RA Kyle: Monoclonal gammopathy of undetermined significance, Waldenström macroglobulinemia, AL amyloidosis, and related plasma cell disorders: diagnosis and treatment . In: Mayo Clin Proc. , 2006 May, 81 (5), pp. 693-703. Review. PMID 16706268
- M. Kortüm et al .: DGHO guidelines “Monoclonal gammopathy of unclear significance” (MGUS). Status August 2010. DGHO guideline "MGUS"
- RA Kyle et al .: International Myeloma Working Group. Monoclonal gammopathy of undetermined significance (MGUS) and smoldering (asymptomatic) multiple myeloma: IMWG consensus perspectives risk factors for progression and guidelines for monitoring and management . In: Leukemia , 2010, 24, pp. 1121-1127. PMID 20410922
- Wikilite.com: Information page on Monoclonal Gammopathy of Indeterminate Significance (MGUS) English-language page with extensive current literature references.
Individual evidence
- ^ A b RA Kyle et al .: Review of 1027 patients with newly diagnosed multiple myeloma . In: Mayo Clin Proc . 78, No. 1, Jan 2003, pp. 21-33. doi : 10.4065 / 78.1.21 . PMID 12528874 .
- ↑ a b A Dispenzieri et al .: Prevalence and risk of progression of light-chain monoclonal gammopathy of undetermined significance: a retrospective population-based cohort study . In: Lancet . 375, No. 9727, May 15, 2010, pp. 1721-1728. doi : 10.1016 / S0140-6736 (10) 60482-5 . PMID 20472173 .
- ^ A b RA Kyle et al .: Prevalence of monoclonal gammopathy of undetermined significance . In: N Engl J Med . 354, No. 13, March 30, 2006, pp. 1362-1369. doi : 10.1056 / NEJMoa054494 . PMID 16571879 .
- ↑ onkopedia.com - Initial diagnosis of multiple myeloma - DGHO guidelines , October 21, 2012.
- ↑ a b c d e f g h N van de Donk et al .: The clinical relevance and management of monoclonal gammopathy of undetermined significance and related disorders: recommendations from the European Myeloma Network . In: Haematologica . 99, No. 6, March 21, 2014, pp. 984-96. doi : 10.3324 / haematol.2013.100552 . PMID 23224402 . PMC 4040895 (free full text).
- ↑ A Dispenzieri et al .: International Myeloma Working Group guidelines for serum-free light chain analysis in multiple myeloma and related disorders . In: Leukemia . 23, No. 2, November 20, 2008, pp. 215-224. doi : 10.1038 / leu.2008.307 . PMID 19020545 .
- ^ A b c SV Rajkumar et al .: International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma . In: Lancet Oncology . November 15, 2014, pp. E538 – e548. doi : 10.1038 / leu.2010.60 . PMID 20410922 .
- ↑ Steven P. Treon, Lian Xu, Guang Yang, Yangsheng Zhou, Xia Liu, Yang Cao, Patricia Sheehy, Robert J. Manning, Christopher J. Patterson, Christina Tripsas, Luca Arcaini, Geraldine S. Pinkus, Scott J. Rodig, Donald A. Skifter, Stephen E. Lincoln, Zachary R. Hunter: MYD88 L265P Somatic Mutation in Waldenström's Macroglobulinemia. In: New England Journal. 2012, Volume 367, Issue 9 of August 30, 2012, pp. 826-833.
- ^ RA Kyle et al .: A long-term study of prognosis in monoclonal gammopathy of undetermined significance . In: N Engl J Med . 346, No. 8, February 21, 2002, pp. 564-569. doi : 10.1056 / NEJMoa01133202 . PMID 11856795 .
- ↑ C Cesana et al .: Prognostic factors for malignant transformation in monoclonal gammopathy of undetermined significance and smoldering multiple myeloma . In: J Clin Oncol . 20, No. 6, March 15, 2002, pp. 1625-1634. doi : 10.1200 / JCO.2002.20.6.1625 . PMID 11896113 .
- ^ J Bladé et al .: Pathogenesis and progression of monoclonal gammopathy of undetermined significance . In: Leukemia . 22, No. 9, March 26, 2008, pp. 1651-7. doi : 10.1038 / leu.2008.203 . PMID 18668131 .
- ^ A b RA Kyle et al .: Monoclonal gammopathy of undetermined significance (MGUS) and smoldering (asymptomatic) multiple myeloma: IMWG consensus perspectives risk factors for progression and guidelines for monitoring and management . In: Leukemia . 24, February 4, 2010, pp. 1121-1127. doi : 10.1038 / leu.2010.60 . PMID 20410922 .
- ^ N Leung et al .: Monoclonal gammopathy of renal significance: when MGUS is no longer undetermined or insignificant . In: Blood . 120, No. 22, November 22, 2012, pp. 4292-4295. doi : 10.1182 / blood-2012-07-445304 . PMID 23224402 .
- ↑ JP Fermand et al .: How I treat monoclonal gammopathy of renal significance (MGRS) . In: Blood . 122, No. 22, October 9, 2013, pp. 3583-3590. doi : 10.1182 / blood-2013-05-495929 . PMID 24108460 .