Penile prosthesis
A penile prosthesis ( penile implant or erectile tissue implant ) is an implantable product for the treatment of erectile dysfunction , Peyronie's disease , ischemic priapism , deformity and traumatic injury to the penis, as well as for phalloplasty in men or for phalloplasty and metoidioplasty in operations to reassign gender from woman to man. While there are many different types of implants, most fall into one of two categories: flexible and hydraulic implants.
history
The first modern prosthetic reconstruction of a penis is attributed to NA Borgus, a German doctor who in 1936 performed the first surgical attempts on soldiers with traumatic amputation of the penis . He used costal cartilage as a prosthetic material and reconstructed the genitals for both micturition and sexual intercourse . In 1952, Willard E. Goodwin and William Wallace Scott were the first to describe the insertion of synthetic penile implants with acrylic prostheses . Silicone-based penile implants were developed by Harvey Lash and the first case series were published in 1964. NASA is credited with developing a high quality silicone used in penile implants today. The prototypes of contemporary inflatable and pliable penile implants were discovered by two groups of physicians from Baylor University (Gerald Timm, William E. Bradley, and F. Brantley Scott) and the University of Miami (Michael P. Small and Hernan M. Carrion). Small and Carrion pioneered the popularization of semi-rigid penile implants in 1975 with the introduction of the Small Carrion prosthesis (Mentor, USA ). Brantley Scott described the initial device consists of two inflatable cylindrical bodies made of silicone, a reservoir with radiopaque liquid and two pump units consisting. The first generation products were marketed by American Medical Systems (AMS; now Boston Scientific ), with which Brantley Scott was associated. AMS has released numerous prosthesis updates since the first generation implants. In 1983 Mentor (currently Coloplast ) came on the market. In 2017 there were more than ten manufacturers of penile implants worldwide, but only a few are still on the market. One of the most recent additions to the market is Zephyr Surgical Implants, which, along with penile implants for CIS men, introduced the first line of hydraulic and flexible penile prosthesis for sex reassignment in trans men .
According to an analysis of the 5% Medicare Public Use Files from 2001 to 2010, about 3% of patients diagnosed with erectile dysfunction opt for an erectile tissue implantation. Nearly 25,000 inflatable (hydraulic) penile prostheses are implanted in the United States each year.
The list shows the penile implants available on the market in 2020.
| product | Companies | Country of origin | Type of implant | Introduced in |
|---|---|---|---|---|
| AMS Spectra | Boston Scientific ( formerly American Medical Systems ) | United States | Flexible | 2009 |
| Tactra | Boston Scientific ( formerly American Medical Systems ) | United States | Flexible | 2019 |
| genesis | Coloplast | United States | Flexible | 2004 |
| ZSI 100, ZSI 100 FtM and ZSI 100 D4 | Zephyr Surgical Implants | Switzerland | Flexible | 2012 |
| tube | Promedon | Argentina | Flexible | 2007 |
| AMS Ambicor | Boston Scientific ( formerly American Medical Systems ) | United States | Refillable | 1994 |
| AMS 700 series (LGX, CX, CXR) | Boston Scientific ( formerly American Medical Systems ) | United States | Refillable | 1983 |
| titanium | Coloplast | United States | Refillable | 2002 |
| ZSI 475 and ZSI 475 FtM | Zephyr Surgical Implants | Switzerland | Refillable | 2012 |
Types of penis implants
Flexible (semirigid) erectile tissue implant
The flexible (semi-rigid) penile prostheses consist of a pair of rods that are implanted into the corpora of the penis. The rods are hard, but "malleable" in the sense that they can be brought into the erect position by bending them up by hand. There are two types of flexible implants: one made of silicone with no rod inside, also called soft implants, and another with a spiral wire core made of silver or steel, coated with silicone inside. Some of the models have trimmable ends that are provided for length adjustment. A wide variety of flexible implants are currently available worldwide.
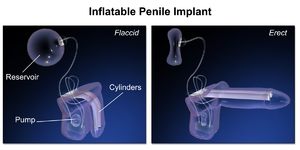
Refillable erectile tissue implant
The inflatable penile implant, which has been developed more recently, consists of a set of inflatable cylinders and a pump system. Because of the differences in structure, there are two types of inflatable implants: two-piece and three-piece. Both types of inflatable prostheses are filled with sterile saline , which is pumped into the cylinders during the process. The cylinders are implanted in the erectile tissue of the penis. The pump system is connected to the cylinders and implanted in the scrotum . With three-part implants, a separate large reservoir is connected to the pump. The reservoir is usually placed in the retropubic space (Cavum Retzii), but other locations have also been described, e.g. B. between the transverse muscle and the rectus muscle . Three-part implants provide the desired rigidity and a girth of the penis that is similar to a natural erection. In addition, due to the large reservoir, three-piece implants provide complete relaxation of the penis when the fluid is drained, making them more comfortable than two-piece inflatable or malleable implants.
The saline solution is pumped manually from the reservoir into bilateral cylinder chambers that are implanted in the shaft of the penis and replace the cavernous bodies that do not function or that function only minimally. This leads to an erection. The glans of the penis , however, remains unaffected. Ninety to ninety-five percent of refillable prostheses produce erections suitable for sexual intercourse . In the United States, the refillable prosthesis has largely replaced the pliable prosthesis due to the lower infection rate, long implant life and 80-90% satisfaction rate.
The first prototype, presented by Scott and colleagues in 1975, was a three-part prosthesis (two cylinders, two pumps, and a fluid reservoir). Since then, the IPP has undergone numerous modifications and improvements in terms of the reliability and durability of the implant, including changes to the chemical material used in implant manufacture, the use of hydrophilic and antibiotic-eluting coatings to reduce infection rates, the introduction of the one-button Approval, etc. As the products have developed, the surgical techniques for implanting penile prostheses have also improved. Refillable penile implants were one of the first procedures in urology to introduce the "no-touch" surgical technique. This enabled the rate of postoperative infections to be significantly reduced.
Medical use
Erectile dysfunction
Despite the recent rapid and extensive development of nonsurgical treatments for erectile dysfunction , particularly novel targeted drugs and gene therapy , penile implants remain the mainstay and gold standard for the treatment of erectile dysfunction in patients resistant to oral drugs and injectable therapy. In addition, implants can be a relevant option for people with erectile dysfunction who seek a permanent solution without drug therapy. Penile implants have been used to treat erectile dysfunction for a variety of causes, including vascular, cavernous, neurogenic, psychological, and post-operative (e.g. prostatectomy ). The American Urological Association recommends educating all men with erectile dysfunction about penile implants as a treatment option and discussing the possible results with them.
Deformity of the penis
Penis implants can help restore the penis to its natural shape in various conditions that have led to penile curvature. These can be traumatic injuries, penile surgery, disfiguring and fibrous diseases of the penis such as Peyronie's disease . In Peyronie's disease, the change in the curvature of the penis interferes with normal sexual intercourse and causes erectile dysfunction due to an interruption in blood flow in the erectile tissue of the penis. Therefore, the implantation of penile prostheses in Peyronie's disease addresses several mechanisms involved in the pathophysiology of the disease.
Gender reassignment from woman to man
Although various models of prosthesis are implanted after phalloplastic surgery, described in the first case of the 1978 by Pucket and Montie, the first erectile tissue implants specifically designed and manufactured for female-to-male sex reassignment surgery did not appear until 2015 by Zephyr Surgical Implants are introduced. Both flexible and inflatable models are available. These implants have a more realistic shape with an ergonomic glans at the tip of the prosthesis. The refillable model has a pump with a refillable cover that resembles a testicle. The prosthesis is implanted with a strong suture fixation on the pubic bone . Another, thinner, flexible implant is intended for metoidioplasty. These prostheses are all single-cylinder, as there are no cavernous spaces in the Transmann. The fixation on the pubic bone prevents the prosthesis from migrating during sexual activities.
Results
satisfaction
The overall satisfaction rate with erectile tissue implants reaches over 90%. Both self-reported and partner-reported satisfaction rates are evaluated to evaluate the results. It has been shown that the implantation of a refillable penile prosthesis brings more patient and partner satisfaction than drug therapy with PDE5 inhibitors or intracavernous injections. Satisfaction rates are reportedly higher with refillable rather than malleable implants, but there is no difference between 2 and 3-piece products. The most common reasons for dissatisfaction are reduced penis length and girth, disappointed expectations and difficulties in using the implant. Therefore, it is crucial to provide detailed preoperative advice and guidance to patients and their partners.
Correction of the curvature
33% to 90% of cases of Peyronie's disease patients who have had a refillable PI procedure have successfully corrected their penile deformity. The residual curvature after an implantation usually requires additional surgical intervention.
Complications
The most common complication associated with penile implant placement appears to be infection, with rates of 1-3% reported. Infections at both the surgical site and the implantation site are reported. If the infection affects the penile implant itself, the implant must be removed and the cavities flushed with antiseptic solutions. In this scenario, the insertion of a new implant is required to avoid further tissue fibrosis and shortening of the penis. The rate of repeated operations or replacement of the implant is between 6% and 13%. Other reported complications include perforation of the corpus cavernosum and urethra (0.1-3%), which are common in patients with previous fibrosis, prosthetic erosion or extrusion, change in the shape of the glans, hematoma, shortening of penis length, and malfunction of the implant. Due to the continuous improvement of surgical techniques and modifications of the implants, the complication rates have decreased significantly over time.
In order to overcome the postoperative penile shortening and to increase the perceived length of the penis and patient satisfaction, ventral and dorsal phalloplasty procedures in combination with penile implants have been described. A modified glanulopexy has been proposed to prevent the deformity and hypermobility of the glands that are possible complications of penile implants. In cases of severe penile shortening, sliding techniques have been performed in which the penis is lengthened with penile implants. However, these techniques had higher complication rates and are currently avoided.
Individual evidence
- ^ Paul Perito: Penile Implants . Perito Urology.
- ^ A b Hernan Carrion, Daniel Martinez, Justin Parker, Tariq Hakky, Michael Bickell, Alexander Boyle, Luke Weigand, Rafael Carrion: A History of the Penile Implant to 1974 . In: Sexual Medicine Reviews . 4, No. 3, July 2016, pp. 285-293. doi : 10.1016 / j.sxmr.2016.05.003 . PMID 27871961 .
- ^ Willard E. Goodwin, William Wallace Scott: Phalloplasty . In: Journal of Urology . 68, No. 6, December 1952, pp. 903-908. doi : 10.1016 / S0022-5347 (17) 68301-0 . PMID 13000938 .
- ↑ HARVEY LASH, DONALD C. ZIMMERMAN, ROBERT A. LOEFFLER: Silicone Implantation . In: Plastic and Reconstructive Surgery . 34, No. 1, July 1964, pp. 75-80. doi : 10.1097 / 00006534-196407000-00011 . PMID 14200523 .
- ↑ a b c d e f g Katherine M. Rodriguez, Alexander W. Pastuszak: A history of penile implants . In: Translational Andrology and Urology . 6, No. S5, November 2017, pp. S851-S857. doi : 10.21037 / tau . 04.02.2017 . PMID 29238664 . PMC 5715175 (free full text).
- ^ A b F. Brantley Scott, William E. Bradley, Gerald W. Timm: Management of erectile impotence Use of implantable inflatable prosthesis . In: Urology . 2, No. 1, July 1973, pp. 80-82. doi : 10.1016 / 0090-4295 (73) 90224-0 . PMID 4766860 .
- ↑ Michael P. Small, Hernan M. Carrion, Julian A. Gordon: Small-Carrion penile prosthesis . In: Urology . 5, No. 4, April 1975, pp. 479-486. doi : 10.1016 / 0090-4295 (75) 90071-0 . PMID 1093303 .
- ^ Culley C. Carson: F. Brantley Scott: a visionary in the world of urology . In: Trends in Urology & Men's Health . 9, No. 3, May 2018, pp. 32–33. doi : 10.1002 / tre.639 .
- ↑ a b c d Eric Chung: Penile prosthesis implant: scientific advances and technological innovations over the last four decades . In: Translational Andrology and Urology . 6, No. 1, February 2017, pp. 37-45. doi : 10.21037 / tau . 12/06/2016 . PMID 28217449 . PMC 5313299 (free full text).
- ↑ Daniel J. Lee, Bobby B. Najari, Wesley L. Davison, Bashir Al Hussein Al Awamlh, Fujun Zhao, Darius A. Paduch, John P. Mulhall, Bilal Chughtai, Richard K. Lee: Trends in the Utilization of Penile Prostheses in the Treatment of Erectile Dysfunction in the United States . In: The Journal of Sexual Medicine . 12, No. 7, July 2015, pp. 1638-1645. doi : 10.1111 / jsm.12921 . PMID 26096365 .
- ↑ Rabih O. Darouiche, Anthony J. Bella, Timothy B. Boone, Gerry Brock, Gregory A. Broderick, Arthur L. Burnett, Raphael Carrion, Culley Carson, Brian Christine, Chipriya B. Dhabuwala, Lawrence S. Hakim, Gerard Henry , LeRoy A. Jones, Mohit Khera, Drogo K. Montague, Ajay Nehra: North American Consensus Document on Infection of Penile Prostheses . In: Urology . 82, No. 4, October 2013, pp. 937-942. doi : 10.1016 / j.urology.2013.05.048 .
- ^ Paul Perito: Malleable Penile Implant Prosthesis . Perito Urology.
- ^ Brian Le, Arthur L. Burnett: Evolution of penile prosthetic devices . In: Korean Journal of Urology . 56, No. 3, 2015, p. 179. doi : 10.4111 / kju.2015.56.3.179 . PMID 25763121 .
- ^ Paul Perito: Penile Implants . Perito Urology.
- ^ J. Francois Eid: Penile Implant: Review of a "No-Touch" Technique . In: Sexual Medicine Reviews . 4, No. 3, July 2016, pp. 294-300. doi : 10.1016 / j.sxmr.2016.01.002 . PMID 27871962 .
- ↑ a b c d Mathew Q Fakhoury, Joshua Halpern, Nelson Bennett: Recent advancements in penile prosthetics . In: F1000Research . 8, February 18, 2019, p. 193. doi : 10.12688 / f1000research.17407.1 . PMID 30828431 .
- ↑ Arthur L. Burnett, Ajay Nehra, Rodney H. Breau, Daniel J. Culkin, Martha M. Faraday, Lawrence S. Hakim, Joel Heidelbaugh, Mohit Khera, Kevin T. McVary, Martin M. Miner, Christian J. Nelson, Hossein Sadeghi-Nejad, Allen D. Seftel, Alan W. Shindel: Erectile Dysfunction: AUA Guideline . In: Journal of Urology . 200, No. 3, September 2018, pp. 633–641. doi : 10.1016 / j.juro.2018.05.004 . PMID 29746858 .
- ↑ a b c James Anaissie, Faysal A. Yafi: A review of surgical strategies for penile prosthesis implantation in patients with Peyronie's disease . In: Translational Andrology and Urology . 5, No. 3, June 2016, pp. 342-350. doi : 10.21037 / tau.04.04.2016 . PMID 27298781 . PMC 4893506 (free full text).
- ↑ Marco Falcone, Giulio Garaffa, Arianna Gillo, Dino Dente, Andrew N. Christopher, David J. Ralph: Outcomes of inflatable penile prosthesis insertion in 247 patients completing female to male gender reassignment surgery . In: BJU International . 121, No. 1, January 2018, pp. 139–144. doi : 10.1111 / bju.14027 . PMID 28940910 .
- ↑ CHARLES L. PUCKETT, JOSEPH E. Montie: Construction of Male Genitalia in the Transsexual, Using a Tubed Groin Flap for the penis and a Hydraulic Inflation Device . In: Plastic and Reconstructive Surgery . 61, No. 4, April 1978, pp. 523-530. doi : 10.1097 / 00006534-197804000-00005 . PMID 345304 .
- ^ Paul Neuville, Nicolas Morel-Journel, Delphine Cabelguenne, Alain Ruffion, Philippe Paparel, Jean-Etienne Terrier: First Outcomes of the ZSI 475 FtM, a Specific Prosthesis Designed for Phalloplasty . In: The Journal of Sexual Medicine . 16, No. 2, February 2019, pp. 316–322. doi : 10.1016 / j.jsxm.2018.11.013 . PMID 30638882 .
- ↑ a b c Sarah C. Krzastek, Ryan Smith: An update on the best approaches to prevent complications in penile prosthesis recipients . In: Therapeutic Advances in Urology . 11, January 8, 2019, p. 175628721881807. doi : 10.1177 / 1756287218818076 . PMID 30671142 .
- ↑ Selahittin Çayan, Ramazan Aşcı, Ozan Efesoy, Mustafa Suat Bolat, Erdem Akbay, Önder Yaman: Comparison of Long-Term Results and Couples' Satisfaction with Penile Implant Types and Brands: Lessons Learned From 883 Patients With Erectile Dysfunction Who Underwent Penile Prosthesis Implantation . In: The Journal of Sexual Medicine . 16, No. 7, July 2019, pp. 1092-1099. doi : 10.1016 / j.jsxm.2019.04.013 . PMID 31155387 .
- Jump up ↑ Matthew J. Ziegelmann, Manaf Alom, Raevti Bole, Tobias Kohler, Landon Trost: Modified Glanulopexy Technique for Supersonic Transporter Deformity and Glanular Hypermobility in Men With Penile Prostheses . In: The Journal of Sexual Medicine . 15, No. 6, June 2018, pp. 914-919. doi : 10.1016 / j.jsxm.2018.04.633 . PMID 29731427 .