Relaxometry
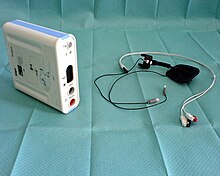
As relaxometry or Neuromuscular monitoring (NMM) is referred to the monitoring of the neuromuscular transmission of impulses to the motor end plate with the use of muscle relaxants ( relaxation , neuromuscular blockade ) under an anesthetic . Using two electrodes, a peripheral nerve is stimulated by the relaxometer and the resulting muscle response is measured qualitatively or quantitatively. Based on these values, the anesthetist can assess the effect of the muscle relaxants and control their dosage accordingly.
Basics
In order for a striated skeletal muscle to be activated, the signal from the brain, which is conducted via a motor nerve , must be transmitted to the muscle. This happens at the motor end plate , a chemical synapse that forms the interface between nerve and muscle cells. The messenger substance acetylcholine (ACh) is released from the presynaptic membrane by the action potential , which is conducted through the nerve . It diffuses through the synaptic gap , binds to the acetylcholine receptors of the muscle cell and triggers a muscle contraction there through the influx of sodium ions.
As part of general anesthesia (general anesthesia) , muscle relaxants are administered to improve the conditions for endotracheal intubation or to enable operations in the abdominal cavity . These block the ACh receptors on the muscle cell so that signal transmission is no longer possible; the muscle relaxes ( neuromuscular blockade , relaxation ). Relaxometry ( neuromuscular monitoring ) is used to monitor this deliberate blockage . This makes it possible to individually adapt the need for muscle relaxants to the patient, to ensure optimal operating conditions and at the same time to limit the duration of action as precisely as possible.
In relaxometry, a peripheral nerve is stimulated through the skin (transcutaneously) via two glued-on electrodes and the response of the associated muscle is measured. A supramaximal current strength (approx. 40–60 mA ) ensures complete excitation of the nerves and reproducibility of the findings. In addition to the current intensity, optimal stimulation is achieved through a monophasic, rectangular shape of the pulse and a duration of around 0.2 ms.
The adductor pollicis muscle is usually used as the test muscle , while the ulnar nerve is stimulated . In the course of the neuromuscular blockade, this differs in its properties from other, clinically relevant muscle groups ( diaphragm , larynx muscles ). The orbicularis oculi muscle ( stimulated via the facial nerve ) shows better agreement . The flexor hallucis brevis muscle ( posterior tibial nerve ) can also be used if wrist monitoring is not possible.
Stimulation pattern
Single stimulation
A single stimulation ( single twitch ) is the simplest form of stimulation. It can be used to check the correct electrode position and to adjust the stimulus strength.
Train-of-four
Train-of-Four (TOF) is the most widely used stimulation pattern in relaxometry and the standard for monitoring the effects of non-depolarizing muscle relaxants. A series of four stimuli is emitted at a speed of 2 Hz. In addition to the extent, the type of neuromuscular blockage can also be determined. TOF stimulation is suitable for monitoring during all phases of anesthesia.
When relaxing with depolarizing muscle relaxants ( succinylcholine ), the stimulus responses are evenly reduced; when using non-depolarizing substances, a decrease (fatigue, fading ) from the first to the fourth response can be ascertained with increasing effect . This ratio (T4 / T1) is known as the TOF quotient or TOF ratio and is 1.0 for the non-relaxed muscle. With increasing relaxation, this quotient becomes smaller; with deep relaxation, under certain circumstances only individual or no stimulus responses can be evoked ( TOF number : with two remaining answers, TOF number 2).
Tetanic stimulation
A high-frequency nerve stimulation leads to the fusion of the associated muscle contractions ( tetanus ). After a short series of stimuli at 50 Hz, the increased transmitter release at the motor end plate leads to a temporary increase in the muscle reactions, which can be determined with subsequent individual stimulations. This procedure is known as Post Tetanic Count (PTC) and enables monitoring during very deep relaxation when TOF stimulation can no longer generate a response.
Double burst stimulation
With double burst stimulation (DBS), a double series of three and three (DBS 3.3) or three and two (DBS 3.2) stimuli is delivered. This sequence is intended to facilitate the tactile assessment during the recovery of the blockage; it is used during the anesthesia recovery.
Registration methods
There are various methods of measuring the stimulus response of the stimulated muscle. The visual or tactile assessment allows a deep relaxation to be checked, but is imprecise in the recovery phase and a differentiation between TOF quotients> 0.5 is not possible. In mechanomyography (MMG), the development of muscle strength is measured using a force transducer. It is the scientific reference method, but is not suitable for clinical practice. The electromyography (EMG) measures the induced over the test muscle action potentials, which is performed by means of two measuring electrodes. It is disadvantageous that it is influenced by movements, electrical artifacts and cold. The Akzeleromyografie (AMG) measures the acceleration of a piezo sensor , the z. B. is attached to the end of the thumb and is a clinical routine method due to the sufficient accuracy and good practicability. In addition to these, there are other measurement methods.
Clinical use
Relaxometry is mainly used for interventions in which muscle relaxation is mandatory (abdominal interventions, eye operations, etc.). It enables the control of the strength and duration of the effectiveness of muscle relaxants, which can be dosed in such a way that there is sufficient neuromuscular blockage, if necessary, while overdosing with a prolonged anesthetic duration can be avoided.
Due to the routine use in all anesthesia with the use of muscle relaxants, a relaxation overhang (residual blockade of the muscles) after anesthesia can be almost excluded. Although requested by some authors, such a broad application has not yet prevailed in practice compared to a purely clinical assessment by the anesthetist.
Historical aspects
Harvey and Masland carried out the first measurements of a muscular blockage using nerve stimulation in 1941. With mechanomyographic and electromyographic registration, Botelho developed methods for measuring muscle response in 1955. The first intraoperative monitoring device was designed by Christie and Churchill-Davidson. 1958.
supporting documents
literature
- R. Rossaint, Ch. Werner, B. Zwissler (Ed.): The anesthesiology. General and special anesthesiology, pain therapy and intensive care medicine. 2nd Edition. Springer, Berlin 2008, ISBN 978-3-540-76301-7 .
- Michael Heck, Michael Fresenius: Anesthesiology revision course. 5th edition. Springer, Berlin 2007, ISBN 978-3-540-46575-1 .
- TM Hemmerling, N. Le: Brief review: Neuromuscular monitoring: an update for the clinician. In: Can J Anaesth. 54 (1), Jan 2007, pp. 58-72. PMID 17197470
- D. Nauheimer, G. Geldner: Monitoring of the neuromuscular blockade - methods and devices. In: Anasthesiol Intensivmed Emergency Med Schmerzther. 43 (5), May 2008, pp. 374-381. PMID 18464216
Individual evidence
- ^ L. de Rossi, H. Fritz, L. Kröber, U. Klein: [Cisatricurium in the orbicularis oculi muscle. Comparison of the neuromuscular action of cisatracurium and atracurium in the orbicularis oculi muscle and the adductor pollicis muscle]. In: Anaesthesiologist. 48 (9), Sep 1999, pp. 602-606. PMID 10525592
- ↑ J. Engbaek, D. Ostergaard, J. Viby-Mogensen: Double burst stimulation (DBS): a new pattern of nerve stimulation to identify residual neuromuscular block. In: Br J Anaesth. 62 (3), Mar 1989, pp. 274-278. PMID 2522790
- ↑ T. Fuchs-Buder, R. Hofmockel, G. Geldner, C. Diefenbach, K. Ulm, M. Blobner: Use of neuromuscular monitoring in Germany. In: Anaesthesiologist. 52 (6), Jun 2003, pp. 522-526. PMID 12835874
- ↑ AM Harvey, RL Masland: Actions of durarizing preparations in the human. In: Journal of Pharmacology and Experimental Therapeutics . Vol. 73, Issue 3, 1941, pp. 304-311.
- ^ SY Botelho: Comparison of simultaneously recorded electrical and mechanical activity in myasthenia gravis patients and in partially curarized normal humans. In: Am J Med. 19 (5), Nov 1955, pp. 693-696. PMID 13268466
- ^ TH Christie, HC Churchill-Davidson: The St. Thomas's Hospital nerve stimulator in the diagnosis of prolonged apnoea. In: The Lancet . 1 (7024), Apr 12, 1958, p. 776. PMID 13526270