Semen analysis
A spermiogram is the result of an ejaculate analysis and is used to assess the man's fertility. A spermiogram is performed if there is a suspicion of infertility if the desire to have children is unfulfilled or if sterility is to be ensured after a vasectomy .
After three to five days of abstinence , the semen is usually obtained by means of masturbation in order to ensure sufficient informative value - any further abstinence does not significantly improve the result. The laboratory analysis begins after the sperm has liquefied, which usually begins after about 15-30 minutes. The focus is on the microscopic assessment of the sperm cells with regard to their concentration, mobility and shape. The spermiogram cannot currently be replaced by a rapid test ( sperm test ), since the rapid tests developed so far can only show partial areas of the results of a spermiogram.
Standardized ejaculate analysis according to WHO
The World Health Organization (WHO) has published a laboratory manual that standardizes the methods of examining the ejaculate and assessing it using reference values.
The standard tests and associated reference values are listed in the following table.
| Reference values for a sperm analysis according to WHO | |
| Ejaculate volume | ≥ 1.5 ml (1.4-1.7) |
| PH value | ≥ 7.2 |
| Sperm concentration | ≥ 15 million spermatozoa per milliliter |
| Total sperm count | ≥ 39 million spermatozoa |
| agility | ≥ 32% progressively motile sperm |
| morphology | ≥ 4% (3.0-4.0%) |
| Share of living sperm ( eosin test) | ≥ 50% |
| Spermatozoa antibody determination • Mixed antiglobulin reaction (MAR) • Immunobead test (IBT) |
<50% sperm with adhering particles <50% sperm with adhering particles |
| Leukocytes | <1 million per milliliter |
More recent data from the USA and China indicate that the reference values may no longer be adequate for the future, as the parameters in France have also deteriorated continuously over the last few decades. As a possible criticism of the above Reference values and relatively narrow limits in the WHO manual must be taken into account in more recent studies that state that fertile men show a wide variation in the classic parameters of sperm quality. In the Chinese study, 62.2% showed normal semen parameters according to the WHO criteria from 2010, but 37.8% showed values that were too low for at least one of the parameters.
Macroscopic and physico-chemical properties
Parameters of the sperm such as quantity, appearance, viscosity , liquefaction time and pH value are assessed. The normal pH value is slightly alkaline, an acidic pH value has a killing effect on the sperm cells. A brownish discoloration can indicate the presence of blood. Ideally, the volume should be at least 1.5 ml and liquefaction should start within 15–30 minutes. When dripping off a glass rod, the sample may pull short but not long threads. If necessary, the ejaculate must be liquefied before the further examination, otherwise the results may be falsified.
Spermatozoa Concentration
The concentration of spermatozoa in the ejaculate is determined by counting them in a hemocytometer . For this purpose, defined amounts of two different dilutions of the ejaculate are introduced into the counting chambers of the cytometer and viewed under a phase contrast microscope . After the counting process has been completed, the sperm concentration can be calculated back, taking into account the degree of dilution.
Mobility (motility)
The WHO divided motility into three categories:
- progressive motility (PR) = progressive mobility
- non-progressive motility (NP) = only local mobility, "circular swimmer"
- immotile = no mobility
The examination is carried out microscopically. A distinction between "fast progressive motile (a)" and "slowly progressive motile (b)" is no longer made. Progressive mobility (PR) occurs when the spermatozoa actively move forward linearly or in a large arc, regardless of speed. Non-progressive local motility (NP) is present in all other patterns of sperm motility without progression, e.g. B. Swimming in small circles, tail movements that do not move the head, or when only tail motility can be observed. The mobility is classified as normal if more than 32% of the spermatozoa move progressively (category PR) and at least 40% (38–42%) move at all (category PR + NP).
The " Computer Assisted Sperm Analysis " (CASA, German: computer- assisted sperm analysis ) is an objective measuring system . The microscopic image is digitized by a computer. The distances covered by the sperm cells are calculated from several successive images.
morphology
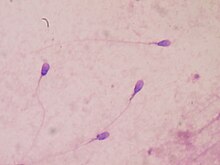
While the limit value for the proportion of normally formed spermatozoa was set at 30% in the 1992 edition, the current edition only has a value of 4%.
Human spermatozoa can be morphologically assessed according to various criteria, whereby microscopically determined shape defects on the head, middle and tail ( flagellum ) are classified and weighted differently. In addition to the WHO criteria of 1992, the “strict criteria” according to Kruger, for example, are also used, which apply particularly strict standards in the assessment.
vitality
The vitality (proportion of living spermatozoa) is determined by staining dead spermatozoa with the dye eosin , which penetrates the cell interior through the cell membrane. The cell membrane of living sperm cells, on the other hand, is impermeable to eosin. Stained and unstained cells are counted under the microscope.
Spermatozoa Antibodies
The presence of sperm antibodies (English: antisperm antibodies , ASA) in the seminal fluid can also impair fertility ( "immunological infertility" ). These antibodies are directed against the sperm cells by binding to their surface in an autoimmune reaction and inhibiting the sperm cells. The ejaculate is therefore tested for IgA and IgG spermatozoa antibodies using a mixed antiglobulin reaction (MAR) or an immunobead test (IBT). The principle of both tests is based on the fact that antibody-bearing spermatozoa are made visible under the microscope through agglutination with antiglobulin-coated particles or spheres. At most half of the motile sperm cells may be coated with antibodies and bond with the particles.
Biochemical investigation
Optionally, the laboratory manual also provides for biochemical analyzes to be carried out, which are listed in the following table. Deviating values indicate possible functional disorders of the prostate , the seminal vesicle and the vas deferens .
| Optional biochemical tests and normal values | |
| α-glucosidase | > 11 mU / l ejaculate |
| Fructose | > 13 µmol / l ejaculate |
| zinc | > 2.4 µmol / l ejaculate |
Assessment of the semen analysis
The WHO has established the following nomenclature for assessing the semen analysis.
| Assessment of the semen analysis using the WHO reference values | |
| Normozoospermia | ("normal") ejaculate parameters corresponding to the reference values |
| Oligozoospermia | <15 million spermatozoa per milliliter or <39 million spermatozoa per ejaculate |
| Asthenozoospermia | <32% progressively motile sperm |
| Teratozoospermia | reduced proportion of morphologically normal spermatozoa |
| Oligoasthenoteratozoospermia ( OAT syndrome ) | Combination of insufficient concentration, insufficient mobility and a reduced proportion of normal sperm morphology |
| Azoospermia | No spermatozoa in the ejaculate |
| Aspermia | no ejaculate |
Further deviations from the norm
| Explanation of terms | |
| Multispermia (polysemia) | > 6 ml ejaculate volume |
| Hypospermia (parvisemia) | <2 ml ejaculate volume |
| Cryptozoospermia | <1 million sperm per milliliter |
| Hyperzoospermia | > 150 million sperm per milliliter |
| Polyzoospermia | > 200 million sperm per milliliter |
| Necrozoospermia | only dead, immobile sperm present in the ejaculate |
Individual evidence
- ↑ a b c d WHO laboratory manual for the Examination and processing of human semen, WHO 5th ed. WHO June 2010. apps.who.int (PDF)
- ↑ Geoffroy-Siraudin C, Guichaoua MR and a .: Decline of semen quality among 10 932 males consulting for couple infertility over a 20-year period in Marseille, France. In: Asian J Androl. 2012 Jul; 14 (4), pp. 584-90. PMID 22522503
- ↑ Redmon JB, Swan SH u. a .: Semen Parameters in Fertile US Men: The Study for Future Families. In: Andrology 2013 Nov; 1 (6), pp. 806-14. PMID 24009155
- ↑ Yun-Ge Tang, Wei-Bing Qin and others. a .: The reference values for semen parameters of 1213 fertile men in Guangdong Province in China. In: Asian J Androl. 2015; 17 (2), pp. 298–303. PMID 25432502
- ↑ a b World Health Organization. Laboratory manual for the examination of human semen and sperm-cervical mucus interaction, 3rd ed. Cambridge, Cambridge University Press, 1992.
- ↑ TF Kruger et al. a .: New method of evaluating sperm morphology with predictive value for human in vitro fertilization. In: Urology. 1987 30 (3), pp. 248-251. PMID 3629768
- ↑ R. Menkveld, TF Kruger: Advantages of strict (Tygerberg) criteria for evaluation of sperm morphology. In: Int J Androl. 1995 (18), Suppl 2, pp. 36-42. Review. PMID 8719857
- ↑ K. Abshagen, HM Behre, TG Cooper, E. Nieschlag: Influence of sperm surface antibodies on spontaneous pregnancy rates. In: Fertility and Sterility . 70 (2), 1998, pp. 355-356. PMID 9696234
Web links
- WHO Laboratory Manual 5th Edition 2010
- Seed test: in practice or at home? Federal Center for Health Education (BZgA)