Spina bifida
| Classification according to ICD-10 | |
|---|---|
| O35.0 | Care of the mother with (suspected) malformation of the central nervous system in the fetus. |
| Q76.0 | Spina bifida occulta |
| Q05.- | Spina bifida aperta |
| ICD-10 online (WHO version 2019) | |
A Spina bifida is a Neuralrohrfehlbildung that different forms can have different weights and has a corresponding effect. The time range for the development of this malformation is between the 22nd and 28th day of embryonic development , namely the period of so-called primary neurulation , i.e. the formation of the neural tube from the neural plate and its closure - in the case of spina bifida of the lower end. Spina bifida occurs in Central Europe on average in one in 1000 children, with girls being affected slightly more often than boys.
etymology
The term spina bifida is derived from the Latin spina for "sting" or "thorn", which refers to the processus spinosus , the spinous process of the vertebral body; the Latin bifidus means “split in two”. Spina bifida therefore means "split spinous process". In German "Wirbelspalt" is common. The German term “open back” only applies to the special form of the spina bifida aperta (see below).
Expressions
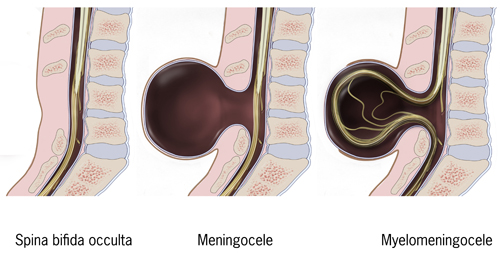
There are different types of spina bifida :
- Spina bifida occulta
- Occulta means "hidden, not visible". This form of spina bifida is characterized in that only one to two forked vertebral arch place without the spinal cord with its spinal meninges (meninges) is involved. It is therefore not visible from the outside. The Spina bifida occulta is quite common and is often only by chance during X-rays detected or an examination of the back. Spina bifida occulta is found with remarkable frequency, especially in bed-wetting children . As a rule, it has no special medical significance; treatment is not necessary. A dermal sinus can occur.
Spina bifida occulta : cleft arch on the posterior arch of the atlas in computed tomography
- Spina bifida aperta
-
Aperta means "open, visible". There are three different forms:
- Meningocele : A simple, light form of spina bifida aperta compared to the other two types is the meningocele . Only the membranes of the spinal cord (= meninges) bulge through a vertebral arch under the skin. The resulting blister (= cyst ) is visible. It can be surgically removed. There are no impairments, because the spinal cord is in its usual position and not damaged.
- Myelomeningocele : In this more severe form, there is a gap in the spine ( cell = fracture) and through this gap parts of the spinal cord (= myelon ), the spinal cord membranes (= meninges) and nerves in a bladder (= cyst) visibly protrude outwards . As a result, the nerve cords lose their protection in the affected area, and damage occurs. The incident described can be surgically covered by meninges.
- Myeloschisis : This term is often used for particularly severe findings of a spina bifida aperta in which the nerve tissue in the affected area is visibly completely exposed and not covered by skin or connective tissue .
A combination of a meningomyelocele with a spinal lipoma is called a lipomeningomyelocele .
Effects
Depending on the severity of the malformation, i.e. depending on the severity of the damage to the spinal cord, people with spina bifida aperta are hardly or very severely physically impaired . Problems with walking up to paralysis of the legs and reduced or completely eliminated sensitivity are possible (paraplegia). Control over the bowel and bladder is also often limited or eliminated. It essentially depends on the height of the spine the malformation is located and how severely the nerves are affected. Often occurs together with spina bifida , a hydrocephalus (accumulation of cerebrospinal fluid in the brain fluid chambers due to a discharge failure) on. This allows portions of the lower brain stem and cerebellum to be shifted down into the foramen magnum and into the upper cervical canal. This leads to CSF circulation disorders and is known as Arnold-Chiari malformation . The cognitive development of the child is usually not impaired if spina bifida is present alone , while additional brain malformations or untreated hydrocephalus can negatively affect the prognosis . However, exact predictions are not possible due to the different location and the individual extent of the damage.
People with spina bifida are more likely to have an allergic reaction to latex . However, the cause is not yet known. It is believed that it is triggered by frequent contact with latex through increased hospital stays and operations (or through latex catheters). Since latex was avoided in medical care, latex allergies have become less common among children with spina bifida.
In Hindu areas, children with tail-like appendages are sometimes worshiped as the reincarnation of the monkey god Hanuman and given gifts.
diagnosis
Nowadays, ultrasound examinations in prenatal diagnosis can often diagnose spina bifida aperta before birth. A suitable diagnostic method is fine ultrasound ; the triple test can estimate the likelihood of a neural tube malformation . The ICD-10 code O35.0 is given when caring for the expectant mother in the event of (suspected) malformation of the central nervous system in the unborn child.
The diagnosis of spina bifida aperta is immediately possible after birth due to the visible malformation on the back, which is often found in the lumbar spine and sacrum , less often in the thoracic and cervical spine.
The Spina bifida occulta is found just happen normally.
therapy
Because of the risk of infection, a spina bifida aperta must be surgically closed in the first few days after birth at the latest, one variant being skin covering with meninges .
The neurogenic bladder , which is often present , usually requires long-term therapy, as otherwise the kidney function can be lost.
Since most people with spina bifida throughout their lives more or take less medical and daily living support and assistance to complete and often extended particularly in children rehabilitation in orthopedic and urological field are needed, a high degree of cooperation on the part of the affected child and his Environment provided.
Spina bifida can already be operated on prenatally . In the USA from 2003 to 2010 a prospective randomized study ("MOMS-Trial") was carried out on the benefits of open fetal surgery in this disease. The study was terminated prematurely after an interim analysis (of 183 results from the planned 200 operations), as the benefit for the prenatal operated children was already obvious due to several convincing and statistically significant advantages: A drainage of cerebral fluid due to hydrocephalus was at the age of 12 months is necessary for only 40% of the prenatally operated children, in contrast to 82% of the postnatal operated ones (p <0.001). After prenatal surgery, there were also better results with regard to mental and motor development (p = 0.007) as well as a decrease in the displacement of cerebellar and brain stem components, known as Chiari II malformation, into the spinal canal of the cervical spine. However, the open surgical procedure, which requires opening the abdomen and uterus of the pregnant woman through larger incisions in order to be able to close the open back of the fetus, has been associated with considerable maternal trauma and complications.
In Europe, this type of procedure is only performed in a few clinics. Janusz Bohosiewicz has operated open fetal surgery on more than 40 unborn babies at the University Clinic in Katowice / Poland since 2003. Between 2010 and 2020, almost 140 fetuses were operated on prenatal open backs by Martin Meuli in the Children's Hospital Zurich .
The editorial accompanying the publication of the MOMS trial called for the development of a less invasive prenatal surgical method. It was not mentioned that such a gentler, fetoscopic procedure was developed in Germany in 2003 by the pediatrician Thomas Kohl and has since been optimized in over 200 operations.
The aim of this minimally invasive procedure is to completely avoid opening the womb and uterus by making larger incisions. Instead, in the fetoscopic procedure, the unborn child is reached through three small tubes (trocars) with an outer diameter of only 5 mm each. These are ultrasonically guided through an incision of just a few millimeters each, directly through the maternal abdominal wall and uterine wall into the fruit cavity. After partial removal of the amniotic fluid and the filling of the fruit cavity with carbon dioxide ( Partial Amniotic Carbon Dioxide Insufflation = PACI), the unborn baby is positioned so that its open back can be surgically dissected and covered with a patch. This can ensure that the exposed spinal cord is protected from amniotic fluid, stool and mechanical damage throughout the rest of the pregnancy. Since the closure is watertight, it also prevents the loss of cerebral fluid that would otherwise persist over the course of pregnancy via the spina bifida into the fruit cavity. As a result, the displacement of the cerebellum and brain stem ( Chiari malformation type II) can be largely reversed in most cases. The surgical procedure is technically difficult, but it is now almost always possible to securely close the back over the malformation.
Critics of the minimally invasive procedure complained in the spring of 2012 that there were still no adequate and scientifically sound studies on the effectiveness of this procedure and its risks for mother and fetus, as well as the outcome of the children operated on in this way. Only subgroups of prenatally fetoscopically operated children have so far been independently re-examined. A Berlin pediatrician and employee of the Spina-bifida-Ambulanz of the Berlin Charité complained, among other things, that their own individual observations would suggest the need for a moratorium on this intervention, since seven children in Berlin who are being cared for in Berlin have hydrocephalus requiring shunt and all have Chiari II - have malformation and paralysis. A significant advantage of prenatal fetoscopic surgery is currently not conclusively proven when there are high risks for mother and fetus and for the further course of pregnancy compared to surgery on the child after birth. A comparison of the results with the systematically examined pregnancies in the MOMS study is rejected as inadmissible. This criticism is justified primarily with an inadequate data situation, with presumably no personal access to further patient data was given.
This is probably one of the reasons for the statement by the American pediatrician David Shurtleffs, which was also only published in early 2012, that the use of this technique is not yet ethically justifiable. He is not aware of any current data, so his position is based on the results of a controlled study carried out by independent experts on the first 19 interventions carried out between summer 2002 and spring 2009. It is true that the prenatal fetoscopically operated children showed a statistically significantly better leg function than a control group operated only after birth, as well as a lower need for postnatal drainage of excess cerebral fluid (ventriculo-peritoneal shunt implantation). However, some of them were born before the 30th week of pregnancy, three died, and in three cases the operation was discontinued due to insufficient experience with the new procedure.
Since the end of the pilot study on the first 30 pregnant women, current results have been published on the use of the now significantly more sophisticated minimally invasive fetoscopic surgical technique.
The increasingly extensive, well-documented experiences with the method, which were increasingly widespread nationally and internationally in 2012, confirm the positive results of the pilot study: the leg function, if it is still present at the time of the intrauterine operation, is surprisingly good, even if the spina bifida begins in the upper lumbar spine area. In an analysis of 20 children who had prenatally minimally invasive fetoscopic surgery on their spina bifida between July 2010 and December 2011, more than half were born with normal or largely normal leg function. The anal reflex was detectable in 16 of the newborns (80%), although it was weakened in half of the cases. If the cerebral ventricles were still narrow at the time of the operation, implantation of a cerebrospinal fluid drainage system for hydrocephalus therapy was usually not necessary after the birth (within the first year of life, only about every second child who had been operated on prenatally needs a shunt). In contrast, about 80% of infants with spina bifida treated only after birth receive a cerebral fluid drainage. In almost all cases, after the minimally invasive prenatal closure of the spina bifida, a reverse displacement of the displacement of the cerebellar and brain stem, known as the Chiari II malformation, into the spinal canal of the cervical spine was observed.
In contrast to the first 30 or so operations, major maternal and child complications as a result of the operation are rarely observed. Almost all pregnant women who have undergone surgery leave the clinic after about a week to continue the pregnancy at home. However, about half of them are still admitted and monitored in a gynecological clinic from about the 30th week of pregnancy, since at this point in time a vaginal loss of amniotic fluid occurs through the defects in the pericarp caused by the operation. These pregnancies can usually continue for weeks under inpatient supervision. Children who, on average, undergo fetoscopic surgery on their malformation in the 24th week of pregnancy are not born until an average of nine weeks later, after completion of the 33rd week of pregnancy. At this point in pregnancy - with good care by neonatal doctors ( neonatologists ) - child damage due to immaturity of the child's organs hardly occurs. The operation-related mortality of the intervention could be reduced significantly to 3%. In the course of the most recent forty interventions between May 2010 and September 2012, only one child died as a result of an infection of the fruit cavity.
A study published in 2015 with 71 patients from the German Center for Fetal Surgery & Minimally Invasive Therapy came to the result that 72% of the minimally invasive fetal-surgically treated fetuses did not require any new neurosurgical open back surgery after birth.
In summary, the two prenatal surgical procedures offer the opportunity to significantly improve the postnatal prognosis and the quality of life of spina bifida children. However, functions of the lower extremities and presumably also of the bladder and rectum that were lost prior to prenatal surgery cannot be regained. In addition, from a certain brain chamber width at the time of diagnosis, a prenatal spina bifida occlusion can no longer prevent the need for postnatal measures to drain the cerebral fluid.
So far there have been few long-term results, but it is already evident that at least in a small proportion of prenatally operated children, existing functions can be lost again at birth or in the first years of life. Reasons for this can be, for example, as yet unavoidable attachments of the spinal cord ( tethered cord ) in the surgical area, which can lead to loss of function when the patient grows in length or during second interventions to loosen the spinal cord (de-tethering). Also, complications of the Chiari II malformation cannot be avoided in every case, although it has been proven that the malformation can be positively influenced by prenatal surgery. It is also little known to what extent a minimally invasive fetoscopic operation can preserve bladder and rectal dysfunction or even sexual functions. A study (file number 113/12) on the subject of "Interdisciplinary follow-up examination of children with spina bifida after intrauterine endoscopic closure of the myelomeningocele", which was given a positive vote by the ethics committee of the medical faculty of the University of Gießen, is currently devoting itself to these and numerous other questions about the new minimally invasive prenatal surgical procedures.
prevention
Around half of the cases that occur in Germany each year could be prevented. Numerous international studies have shown that the additional intake of folic acid during pregnancy (i.e. about one year before and during pregnancy) can reduce the risk of neural tube defects. Such an increase in folic acid intake is u. a. recommended in the USA, England, the Netherlands and Switzerland and, since June 1994, also in the Federal Republic of Germany.
literature
- Hermann Wendt: De spina bifida. Dissertation inauguralis medica . Berlin 1858.
Web links
Individual evidence
- ↑ K. Masuhr: Neurology. 6th edition. Thieme-Verlag, 2007.
- ↑ asbh-stiftung.de ( Memento from September 15, 2013 in the Internet Archive )
- ↑ Jalees Andrabi: The holy tail. Growth lad, 12, hailed as god. In: The Sun. July 23, 2013, accessed July 26, 2013 .
- ↑ 12-Year-Old Indian Boy With A Tail Growing On His Back Hailed As God. In: The Inquisitr. July 23, 2013. Retrieved July 26, 2013 .
- ↑ NS Adzick, EA Thom u. a .: A randomized trial of prenatal versus postnatal repair of myelomeningocele. In: New England Journal of Medicine . Volume 364, Number 11, March 2011, pp. 993-1004, ISSN 1533-4406 . doi: 10.1056 / NEJMoa1014379 . PMID 21306277 .
- ↑ J. Bohosiewicz, T. Koszutski et al. a .: Fetal repair of myelomeningocele in human fetuses. Experience related with 33 cases. In: Archives of Perinatal Medicine. Volume 17, Number 2, 2011, pp. 81-84.
- ↑ First open back operations before birth. In: Neue Zürcher Zeitung. July 28, 2012.
- ↑ Zurich star surgeon stops - he operated on children before they were born. June 25, 2020, accessed June 25, 2020 .
- ^ JL Simpson, MF Greene: Fetal surgery for myelomeningocele? In: The New England Journal of Medicine . Volume 364, Number 11, March 2011, pp. 1076-1077, ISSN 1533-4406 . doi: 10.1056 / NEJMe1101228 . PMID 21306233 .
- ↑ Thomas Kohl et al .: Percutaneous fetoscopic patch coverage of spina bifida aperta in the human - early clinical experience and potentia . 2006, PMID 16491001
- ^ German Center for Fetal Surgery & Minimally Invasive Therapy (DZFT) at the University Hospital Mannheim: Intrauterine therapy of spina bifida. Retrieved September 13, 2018 .
- ↑ D. Shurtleff: Fetal endoscopic myelomeningocele repair. In: Developmental Medicine and Child Neurology . Volume 54, Number 1, January 2012, pp. 4-5, ISSN 1469-8749 . doi: 10.1111 / j.1469-8749.2011.04141.x . PMID 22126087 .
- ^ RJ Verbeek, A. Heep et al. a .: Fetal endoscopic myelomeningocele closure preserves segmental neurological function. In: Developmental medicine and child neurology. Volume 54, Number 1, January 2012, pp. 15-22, ISSN 1469-8749 . doi: 10.1111 / j.1469-8749.2011.04148.x . PMID 22126123 . (Review).
- ↑ J. Degenhardt, R. Schürg, A. Kawecki, M. Pawlik, C. Enzensberger, R. Stressig, R. Axt-Fliedner, T. Kohl: Maternal outcome after minimally-invasive fetoscopic surgery for spina bifida. The Giessen experience 2010–2012. In: Ultrasound Obstet Gynecol. 40 (Suppl. 1), 2012, p. 9
- ^ B. Neubauer, J. Degenhardt, R. Axt-Fliedner, T. Kohl: Early neurological findings in infants after minimally invasive fetoscopic closure of their spina bifida aperta. In: Z Birth Neonat. 216, 2012, p. 87
- ↑ T. Kohl, A. Kawecki et al. a .: Early neurological findings in 20 infants after minimally-invasive fetoscopic surgery for spina bifida at the University of Giessen 2010-2011. In: Ultrasound Obstet Gynecol. Volume 40, 2012, p. 9.
- ↑ Thomas Kohl et al .: Percutaneous minimally invasive fetoscopic surgery for spina bifida aperta. Part III: neurosurgical intervention in the first postnatal year. Retrieved August 9, 2018 . doi: 10.1002 / uog.14937
- ↑ See MOMS-Trial and J. Degenhardt, A. Kawecki, C. Enzensberger, R. Stressig, R. Axt-Fliedner, T. Kohl: Relocation of the Chiari II malformation within a few days after minimally invasive patch closure as an indication for an effective closure of the malformation. In: Ultrasound in Med. Volume 33, 2012, S95 and J. Degenhardt, A. Kawecki, C. Enzensberger, R. Stressig, R. Axt-Fliedner, T. Kohl: Reversal of hindbrain herniation within a few days after minimally- invasive fetoscopic surgery for spina bifida indicates the desired water-tight closure of the lesion. In: Ultrasound Obstet Gynecol. Volume 40, 2012, p. 74.
- ↑ Pregnancy and childbirth in patients with spina bifida Reinhold Cremer Children's Hospital Cologne ( Memento of the original from July 29, 2014 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. (PDF; 98 kB)
- ↑ Folic acid lowers the risk of spina bifida. In: Deutsches Ärzteblatt.
- ↑ Pediatrics online
- ↑ Margaret A. Honein et al. a .: Impact of Folic Acid Fortification of the US Food Supply on the Occurrence of Neural Tube Defects. (PDF)