Wernicke encephalopathy
| Classification according to ICD-10 | |
|---|---|
| E51.2 | Wernicke encephalopathy |
| ICD-10 online (WHO version 2019) | |
The Wernicke encephalopathy is a degenerative brain disorder enzephaloneuropathische in adulthood. It occurs when there is a vitamin B 1 deficiency.
The first description goes back to Carl Wernicke (1848–1905), who wrote a study of hemorrhagic changes in the gray matter of the corpora mamillaria in three alcoholics in 1881 and referred to this as polioencephalopathia haemorrhagica superior . Further names are pseudoencephalitis haemorrhagica superior , polioencephalitis haemorrhagica and Wernicke syndrome .
The Wernicke-Korsakoff syndrome is a combination of Wernicke's encephalopathy and Korsakoff's syndrome (amnesia with Konfabulationstendenz with or without polyneuropathy). This name was first proposed in 1904 by the German neurologist and psychiatrist Karl Bonhoeffer .
causes
Wernicke encephalopathy is mainly found in malnourished alcoholics, but also in patients with chronic gastritis, chronic inflammatory bowel diseases (such as Crohn's disease ), in the case of prolonged vomiting e.g. B. under chemotherapy or after obesity surgical interventions.
In 2003, several babies in Israel who were fed only thiamine-free food developed the syndrome.
A glucose infusion in alcoholics with an unclear impaired consciousness can trigger Wernicke encephalopathy or Korsakoff syndrome in the case of a latent thiamine deficiency, since the metabolism of glucose requires thiamine as a coenzyme .
Emergence
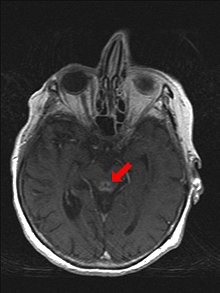
It is based on a vitamin B 1 deficiency ( thiamine ), which leads to disorders in the carbohydrate metabolism due to the failure of energy-rich phosphorylation . After an edematous swelling of the brain, later bleeding and capillary sprouting also occur in certain parts of the brain (corpora mamillaria, hypothalamic core areas around the third ventricle, lamina tecti and periaqueductal gray with oculomotor core areas ). Atrophy of these structures follows .
The combination with Korsakoff syndrome is called Wernicke-Korsakoff syndrome . The damage can become irreversible.
Symptoms
Wernicke encephalopathy is classically described by a triad of symptoms:
- Organic brain psychosyndrome ( HOPS ) with mental changes such as memory loss, psychosis, confusion and confabulations , disorientation
- Unsteady gait and stance (cerebellar ataxia )
- Eye movement disorders and eye muscle paralysis (horizontal nystagmus , ophthalmoplegia , anisocoria , double vision (diplopia)).
In the beginning there are often double vision, speech disorders, unsteady gait and tingling paresthesia of the legs. In addition to the triad of symptoms, reflex disorders, disorders of consciousness, apathy and somnolence , fine motor disorders with dysdiadochokinesis , bulbar speech disorder ( dysarthria ), swallowing disorders ( dysphagia ), sleep disorders ( insomnia ), vegetative disorders such as hypotension , hypothermia and hyperhidrosis can also occur .
diagnosis
The vitamin B 1 level can be detected in the blood, whereby the plasma level can be false-negative . The whole blood test is considered to be more sensitive.
therapy
The treatment is carried out by giving thiamine. Since the absorption of oral thiamine is variable and difficult to control, it must be administered intravenously in an emergency. While there are no studies on the optimal dosage, according to a 2012 review, 200 mg thiamine is usually given over two days. Sometimes 500 mg three times a day for two days, followed by 500 mg thiamine once for five additional days is also recommended. Thereafter, further long-term oral administration is generally recommended.
See also
literature
- G. Sechi, A. Serra: Wernicke's encephalopathy: new clinical settings and recent advances in diagnosis and management. In: The Lancet Neurology . Volume 6, Number 5, May 2007, pp. 442-455, ISSN 1474-4422 . doi : 10.1016 / S1474-4422 (07) 70104-7 . PMID 17434099 . (Review).
- Mario Lanczik: Wernicke's disease. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 1475.
Individual evidence
- ↑ Carl Wernicke: The acute, hemorrhagic poliencephalitis superior. In: Carl Wernicke: Textbook of brain diseases for doctors and students. Volume 2. Verlag von Theodor Fischer, Berlin 1881, pp. 229–242.
- ↑ Bonhoeffer K .: The Korsakow symptom complex in its relationship to the various forms of disease. In: Allg Z Psychiatrie psych-gerichtl Med . tape 61 , 1904, pp. 744-752 .
- ↑ A. Fattal Valevski, A. Kesler, BA Sela include: Outbreak of life-threatening thiamine deficiency in infants in Israel Caused by a defective soy-based formula . In: Pediatrics . tape 115 , no. 2 , February 2005, p. e233 – e238 , doi : 10.1542 / peds.2004-1255 , PMID 15687431 .
- ↑ a b J.F. Merola, PP Ghoroghchian, MA Samuels, BD Levy, J. Loscalzo: At a loss. Clinical problem-solving. In: New England Journal of Medicine . 2012; Volume 367, pp. 67-72.