Cerebral arteriovenous malformation
| Classification according to ICD-10 | |
|---|---|
| Q28.2 | Arteriovenous malformation of the cerebral vessels |
| Q28.29 | Congenital arteriovenous malformation of the cerebral vessels, unspecified |
| ICD-10 online (WHO version 2019) | |
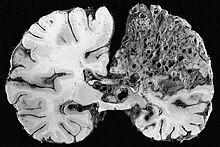
A cerebral arteriovenous malformation (zAVM) (also intracranial arteriovenous malformation ) is a congenital malformation of the blood vessels within the brain in which the arteries are directly connected to the veins without intervening capillaries .
anatomy
→ see arteriovenous malformation
frequency
Cerebral arteriovenous malformations are very rare. Information on the frequency can only be estimated, as not every AVM is clinically suspicious and therefore many remain undetected. It is believed that around 0.05% of the population have an AVM in their brain.
According to a study from 2003, the scientists even assumed that there was only 0.01% of the population and stated that around one million people nationwide, e.g. B. would have to be examined with an MRI for an AVM in order to prove the assumed frequency of one AVM carrier per 10,000 inhabitants.
risk
The greatest risk comes from a possible cerebral hemorrhage . The blood flow within the AVM is increased, the vessel walls are stretched, thinner than usual and therefore more prone to ruptures . The result can be a life-threatening stroke .
Since the exact number of people with cerebral AVM is unknown, the information on the average risk of bleeding is only of limited use. The risk of cerebral hemorrhage is estimated at 2–3% per year and increases after the first bleeding.
In a study in the greater New York area, it was found that the risk of bleeding varies depending on various factors. The authors therefore propose a new assessment system for the risk assessment of cerebral AVM, according to which the risk can be between 0.9% and 34.4% per year, depending on the location of the AVM, the blood-draining veins and a previous cerebral haemorrhage.
Symptoms
Not every cerebral AVM becomes clinically apparent. The AVM is often only discovered after a stroke , along with the symptoms described there .
Cerebral AVM that have not yet caused a cerebral hemorrhage can also be conspicuous by symptoms of a TIA , e.g. B. Sensory disturbances, abnormal sensations, visual or speech disorders or paralysis on one side . The cause is an undersupply of the brain tissue adjacent to the AVM . Due to the short-circuit connections within the AVM, the blood immediately drains unchecked through the veins, the natural resistance from the microscopic capillaries is missing. As a result, the blood pressure in the surrounding brain tissue can be reduced and neurological failures can occur. Which brain functions are affected depends on the location of the AVM in the brain. Also seizures and headaches can be a cerebral AVM symptoms.
diagnosis
Various imaging methods are used for diagnosis with cerebral AVM. With the increased use of these techniques, AVM are also being discovered more and more frequently as a secondary finding.
Computed tomography / angiography
The computed tomography (CT) or CT angiography uses X-rays and therefore also represents a radiation exposure to the body. The investigation takes a few minutes and allows for a brain hemorrhage a quick assessment of the situation. By administering contrast media, the blood vessels and thus the cerebral AVM can be made visible.
Magnetic resonance imaging / angiography
The resolution of the images is slightly higher in magnetic resonance imaging (MRT) or magnetic resonance angiography (MRA) and therefore more accurate. In particular, accompanying changes in the AVM can be better represented. The method works with changing magnetic fields without radiation exposure for the patient and is therefore recognized as a safer method. Since there is no radiation exposure, the MRI is also preferred for regular AVM follow-up examinations after a treatment. The examinations usually take longer, sometimes up to an hour. With the MRI , too , the blood vessels can be better visualized through the targeted administration of contrast media .
Digital subtraction angiography
The most precise and unambiguous detection of a cerebral AVM and blood flow is currently only possible with what is known as digital subtraction angiography (DSA) . It is a medical procedure and is mainly carried out as an inpatient in specialized clinics for planning or final control of a treatment. Here, a catheter z. B. introduced into an artery in the area of the groin and pushed through the main artery past the heart into the arteries supplying the brain. There, under constant X-ray monitoring, contrast agent is injected into individual vessels, which are then clearly visible in the high-resolution images. Computer calculations can remove bones, brain tissue and other parts of the image from the recordings. An exact three-dimensional model of the brain vessels, especially the AVM, is created. Like treatment, the procedure is associated with risks.
Treatment options
In 2007, a global, long-term clinical study ARUBA (A Randomized Trial of Unrupted Brain Arteriovenous Malformations) began, in which 39 specialized clinics from 9 countries took part. The aim of the study was to find out whether or not cerebral AVMs that had previously been clinically normal (i.e. had not yet triggered a cerebral hemorrhage) should be treated. In February 2014, the first interim results were presented and it was announced that the study had not accepted any new study participants since 2013. The reason was that the number of bleeding, stroke and death in the group of treated patients was significantly higher than in the comparison group without treatment. The authors of the study therefore advise against treating cerebral AVM that have not yet caused bleeding. The German Society for Neurology has noted this interim balance in its guidelines and points out that in the case of uninterrupted zAVM, the treatment options should be carefully considered.
In the case of clinically conspicuous zAVM that have already caused a cerebral haemorrhage or are noticeable through sensitivity disorders or other physical or mental impairments, treatment may still be necessary in order to avert greater damage. When assessing whether treatment is appropriate, z. B. the age and condition of the patient play a role. The aim of every treatment is to completely eliminate the short-circuit connection, either by completely removing the affected blood vessels or by closing the blood vessels, as this is the only way to rule out the risk of (renewed) cerebral hemorrhage. However, due to the delicate situation in the brain, every treatment also entails great risks, which must be weighed against the natural risk of bleeding of the cerebral AVM. The appropriate treatment method must be found individually for each patient in an interdisciplinary team of neurosurgeons, neurologists, neuroradiologists, etc., whereby combinations of the treatment methods are also possible.
Neurosurgical removal
Whether neurosurgical removal is an option depends to a large extent on the size and location of the AVM. Possibly. The operation on the open skull can be preceded by embolization . The Spetzler-Martin scale is intended to help neurosurgeons assess the risk and the chances of success of an intervention.
Embolization
In the case of embolization , the so-called endovascular treatment, a catheter, similar to the DSA , e.g. B. led from the inguinal artery to the brain. There, under constant x-ray control, a kind of adhesive, the “embolizate”, occasionally also small platinum spirals, is injected, which seal the vessels internally. The embolizate can e.g. B. consist of ethylene-vinyl alcohol copolymer . Complete closure of the cerebral AVM is often not possible through embolization alone. The intervention is risky, for example, because the embolizate can get into the wrong blood vessels that supply important areas of the brain. The embolization can take place under general anesthesia as well as under local anesthesia, in one or more sessions.
Irradiation
The third treatment method is stereotactic irradiation of the AVM, e.g. B. with the gamma knife or with a linear accelerator . It is usually a one-time irradiation. As a result of the radiation, the cells of the blood vessels in the AVM mutate. They gradually enlarge, which causes the blood vessels to close. This process happens very slowly and can take several years. During this time, the natural risk of AVM bleeding persists. The possible side effects of radiation also require regular follow-up examinations. If the AVM does not close completely due to the radiation, a second radiation may be necessary after several years, which, however, entails a higher risk of side effects.
Society and culture
- With the musical Nervensache (original title: A New Brain ), William Finn processed his experiences as an AVM patient and brought them to the stage in a staged manner. The German premiere was in 2008 at the Theater für Niedersachsen .
- In the American television series Six Feet Under (2001-2005), the series character Nate Fisher suffers from a cerebral AVM. The series addresses the psychological stress after diagnosis several times. The series character suffered a stroke in the last season due to the AVM and died a short time later.
- Cerebral AVM form the framework for individual episodes of various doctor series: Grey's Anatomy (episode 8), Hawthorne (TV series) (episode 5), Royal Pains (episode 6)
- In the English science fiction novel "Mindscan" by Robert J. Sawyer from 2005, the main character suffers from an AVM, which prompts him to be one of the first test patients to copy his consciousness into an artificial body and assign all his personal rights to the copy.
- The American brain researcher Jill Bolte Taylor suffered a stroke in 1996 due to a cerebral AVM. Taylor reported at the TED conference about her experiences during the stroke, the lecture is one of the most watched TED lectures.
Web links
- Patient information with images of cerebral AVM from the Greifswald University Hospital
- Audio contribution: Summary of the entire topic by the German Society for Neuroradiology as part of NeuroRAD 2012
Individual evidence
- ↑ a b c d e f Henkes, Berg-Dammer, Kühne: Arteriovenous malformations. In: Peter Berlit (Ed.): Clinical Neurology . 2nd Edition. Springer Medizin, Heidelberg 2006, ISBN 3-540-01982-0 , pp. 1040 ff. → limited preview in the Google book search. Retrieved December 13, 2011.
- ↑ Stapf, Mast, Sciacca, Berenstein, Nelson, Gobin, Pile-Spellman, Mohr: Research Report: The New York Islands AVM Study - Design, Study Progress, and Initial Results. In: Stroke , issue 34, e29-e33, 2003. PDF of the specialist article (English) . Retrieved December 13, 2011.
- ↑ Hassler, Schick: Arteriovenous malformations of the CNS. In: Moskopp, Wassmann (Hrsg.): Neurosurgery, manual for further training and interdisciplinary reference work. Schattauer, Stuttgart 2005, ISBN 3-7945-1991-4 , pp. 382-392.
- ^ Zeumer, Busch, Debus, Grzyska, v. Kummer, Seifert, Stapf, Westphal: DGN guidelines 2008: Cerebral arteriovenous malformations. German Society for Neurology V., Berlin 2008. PDF of the guidelines . Retrieved December 13, 2011.
- ↑ Stapf, Mast, Sciacca, Choi, Khaq, Connolly, Pile-Spellman, Mohr: Predictors of hemorrhage in patients with untreated brain arteriovenous malformation. In: Neurology Journal . Issue 66, 2006, pp. 1350-1355. Limited online version . Retrieved December 13, 2011.
- ↑ Stapf, Mast, Sciacca, Choi, Khaq, Connolly, Pile-Spellman, Mohr: Predictors of hemorrhage in patients with untreated brain arteriovenous malformation. In: Neurology Journal . Issue 66, 2006, pp. 1350-1355. Link to the appendix "E1" with the English model of the new risk assessment . Retrieved December 13, 2011.
- ↑ Dual Series - Radiology. 2006: Thieme.
- ↑ Official website of ARUBA study (English) . Retrieved December 13, 2011.
- ↑ Official interim results of the ARUBA study . Retrieved May 13, 2013.
- ↑ JP Mohr, Michael K Parides u. a .: Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, non-blinded, randomized trial. In: The Lancet. 2013, S., doi : 10.1016 / S0140-6736 (13) 62302-8 .
- ↑ a b S1 guideline for cerebral vascular malformations of the German Society for Neurology, updated version from 2014, valid until September 2017, PDF version (AWMF register number 030/088, not available online at AWMF at the time of linking)
- ↑ CG: AVM - short circuit in the brain. Surgery because of the risk of bleeding a boomerang? In: Medical Tribune . Volume 41, No. 29, 2009. Online version of the article . Retrieved December 13, 2011.
- ↑ MR: "A New Brain" in German in Hildesheim and Hanover . Online article at Musicalzentrale.de . Retrieved December 13, 2011.
- ↑ Robert J. Sawyer: Mindscan . Excerpt from the novel . Retrieved December 13, 2011.
- ↑ Short biography of Jill Bolte Taylor (English) . Retrieved December 13, 2011.
- ↑ Video: Jill Bolte Taylor tells TED about her stroke . Retrieved December 13, 2011.