Baxter neuropathy
| Classification according to ICD-10 | |
|---|---|
| G57.6 | Plantar nerve lesion |
| ICD-10 online (WHO version 2019) | |
The Baxter neuropathy is a compression syndrome of the nerve calcaneus inferior to the heel , which can lead to chronic painful nerve damage, a neuralgia . This neuropathy of a side branch of the tibial nerve was first described in 1984 by Donald E. Baxter in runners. It is said to be present in up to 20% of all patients with heel pain, often accompanied by other causes.
anatomy
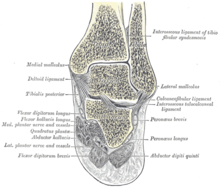
The inferior calcaneus nerve is the first branch of the lateral plantar nerve , which in turn emerges from the tibial nerve together with the medial plantar nerve . In English the nerve is sometimes also called "Baxter nerve". The nerve exit is usually found on the inner (medial) rear foot under the sustentaculum tali of the calcaneus . In the further course, the nerve usually runs medial to the quadratus plantae muscle and laterally to the abductor hallucis muscle , which it innervates, to the sole of the foot (plantarward). It then pivots laterally and runs below (plantar side) the medial process of the heel bone and above (dorsal) the flexor digitorum brevis muscle further towards the outside of the foot, where it usually innervates the abductor digiti minimi muscle .
In the vast majority of cases, the inferior calcaneus nerve branches off from the lateral plantar nerve , in 10% it forms an independent branch of the tibial nerve. Other variants are very rare. As a rule, it innervates both the abductor hallucis and the abductor digiti minimi muscles. In some variants, the nerve also supplies the quadratus plantae muscle , which is usually directly innervated by the lateral plantar nerve , or the flexor digitorum brevis muscle , which is usually innervated by the medial plantar nerve .
The sensitive innervation area of the nerve comprises the medial periosteum of the medial process of the calcaneus, the plantar fascia and the skin on the sole of the foot in the heel and metatarsal area as well as on the inner ankle .
The nerve compression occurs preferentially in two places: on the one hand in the course between the musculus abductor hallucis and the musculus quadratus plantae, on the other hand below the processus medialis of the calcaneus, where the insertion of the plantar fascia is located. Prolonged compression can lead to atrophy of the supplied muscles. The abductor hallucis muscle and the abductor digiti minimi muscle may be affected in the first-mentioned area, and only the latter located further distally in the second-mentioned area.
In contrast to Baxter's neuropathy is found in the (rear) tarsal tunnel syndrome , a compressed tibial nerve in the area of retinaculum behind the medial malleolus before it splits into the two plantar, sometimes at the level of branching. Posterior tarsal tunnel syndrome was known as jogger's foot back in the 1970s . But bottleneck syndromes of the Baxter nerve or the medial plantar nerve also occur more frequently in medium and long-distance runners and are sometimes also referred to as "runner's foot".
causes
The compression syndrome is caused by a narrowing of the nerve. This can appear as idiopathic with no external cause or other explanation. Much more often, however, the compression is based on a change in the vicinity of the nerve. In particular the so-called "heel spur", the plantar fasciitis, can put pressure on the nerves. Even with increased pronation of the foot or hypermobility of the foot, pressure on the nerves can occur; this occurs especially with medium to long distance runners.
In addition, bony changes or variations can lead to increased pressure, as can a stress fracture of the heel bone. An additional (accessory) muscle is rarely created that constricts the nerve. Joint changes, especially inflammation of the lower ankle, are also possible causes . The nerve passes close to the talus suture and the medial articular facet of the talocalcaneal (subtalar) joint located there. Also, obesity can lead to compression.
Symptoms
The symptoms of Baxter neuropathy are quite unspecific. In particular, pain under the heel in the area of the attachment of the plantar fascia and on the inside under the longitudinal arch as well as paresthesia (abnormal sensations) are important indications. Such paresthesias are often localized in a similar way: appearing on the inside under the longitudinal arch and pulling towards the inner ankle, as well as under the heel with radiation towards the outside of the foot. Paresthesia and pain are usually stress-dependent and sometimes only appear in athletes during the course of the race. Paresthesia, on the other hand, does not exist in plantar fasciitis , but it can also be present. Pain and paresthesia can also occur in the morning when you take your first steps or when you get up after sitting for a long time ("starting pain").
On palpation, pain is felt in the area of the attachment of the plantar fascia, similar to that of plantar fasciitis, but possibly with additional paresthesia. Decreased force in abduction of the little toe is seldom and difficult to determine because this movement cannot always be investigated selectively. A weakness of the abductor of the big toe is also difficult to determine during the examination, since this muscle function cannot be tested sufficiently selectively. In the case of nerve entrapment of the medial plantar nerve , the sensory disturbance lies under the longitudinal arch and radiates to the inside from the metatarsus and forefoot and typically on the sole of the foot (plantar) to the big toe.
Diagnosis
On X-rays on Baxter's neuropathy can not be identified, but possibly a kink , lowering or puncture as a risk factor, as well as rare bony changes or abnormalities as well as osteoarthritis . However, osteoarthritis of the lower ankle can be better identified with computed tomography . A heel spur is also apparent in the X-ray.
In ultrasound a plantar fasciitis can be described, but the nerve can hardly visualize because it has a small diameter and is deep. The denervation of the affected muscles can be documented with electromyography (EMG) .
Magnetic resonance imaging is the standard for diagnosis . This allows the compression and its possible cause to be shown, although not always clearly and reproducibly. In addition, the affected muscles show hyperintense neurogenic muscle edema in the acute phase in the fat-suppressed T2-weighting, in the chronic phase in the non-fat-suppressed T1-weighting a hyperintense fat vacuum, whereby the muscle tissue is replaced by adipose tissue. Magnetic resonance imaging can also rule out a rare neuroma.
therapy
As a conservative therapy, anti-inflammatory drugs can be administered, physiotherapy and insoles to support the longitudinal arch are also helpful, as are soft, thick shoe soles for cushioning, especially for runners. In addition, a cortisone injection can be effective for reducing inflammation.
If there is another cause, this should be treated primarily.
Only rarely and after unsuccessful conservative therapy will surgical therapy be considered, in the sense of neurolysis to open the constriction. Because of the anatomical location, surgical access from the sole of the foot is usually chosen for this. Associated with this is the risk of painful scarring under the sole of the foot. If there is an anatomical variant, a bony or an accessory muscle, surgical neurolysis may be more appropriate.
In 1992, Baxter described the course after unilateral or bilateral surgical exposure of the inferior calcaneus in 54 patients with chronic heel pain and previous conservative treatment at least every six months . With neurolysis, 89% of the 69 operated heels achieved good to very good results, and 83% were still pain-free after an observation period of 49 months on average.
literature
- ↑ Nico Hustings, Annemieke Milants, Adelard De Backer, Filip M. Vanhoenacker: Talagie avec paresthésies au bord du nioveau medial du pied. In: Ortho-Rheumatology. Volume 17, No. 3, 2019, pp. 19-21.
- ↑ Donald E. Baxter, CM Thigpen: Heel pain - operative results. In: Foot Ankle. Volume 5, No. 1, 1984, pp. 16-25.
- ↑ Michael N. Brown, Beth S. Pearce, Helen W. Karl: Inferior calcaneal nerve entrapment. In: Peripheral nerve entrapments: clinical diagnosis and management. 2016, pp. 859-870.
- ↑ S. Louisiana, AC Masquelet: The medial and inferior calcaneal nerves: an anatomic study. In: Surgical and radiologic anatomy. Vol. 21, No. 3, 1999, pp. 169-173, PMID 10431329 .
- ↑ MR Rask: Medial plantar neurapraxia (jogger's foot): report of 3 cases. In: Clinical Orthopedics and Related Research. Volume 134, July 1978, pp. 193-195.
- ^ Donald E. Baxter, Glenn B. Pfeffer, Treatment of Chronic Heel Pain by Surgical Release of the First Branch of the Lateral Plantar Nerve. In: Clinical Orthopedics and Related Research. Volume 279, July 1992, pp. 229-236; doi: 10.1097 / 00003086-199206000-00029 .