Lewy body dementia
| Classification according to ICD-10 | |
|---|---|
| G31.82 | Lewy body dementia |
| ICD-10 online (WHO version 2019) | |
The Lewy body dementia , Lewy body dementia or Lewy body dementia (LBD) is after Alzheimer's disease , the second most common neurodegenerative dementia in old age and can occur both as an independent disease and secondary as part of a pre-existing Parkinson's Disease . Lewy body dementia accounts for around 20% of all forms of dementia.
history
The disease is named after Friedrich H. Lewy (1885–1950), a German neurologist. In his book chapter on "Paralysis agitans" (today Parkinson's disease ) he first described the Lewy bodies that were later named after him . During his work at the Berlin Charité he found these changes in the nucleus basalis Meynert and nucleus dorsalis nervi vagi of Parkinson's patients.
Classification
- diffuse Lewy body disease or dementia with Lewy bodies
- Parkinson's disease with accompanying Alzheimer's pathology
- Lewy bodies variant of Alzheimer's disease
A clear differentiation can often only be made post mortem with the histological examination of the changes in the brain.
The division into the group dementia with the presence of diffuse cortical Lewy bodies took place for a long time according to the consensus criteria for Lewy body disease (McKeith et al. 1996), which state that at least two of the following three criteria must be met:
- fluctuating cognitive deficits (especially attention)
- repeated detailed visual hallucinations
- extrapyramidal motor disorders (involuntary motor disorders)
Pathogenesis
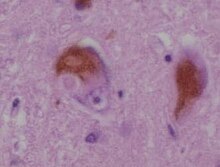
The Lewy bodies , which also make up this disease, were first discovered in Parkinson's disease. These are eosinophilic inclusions in the cytoplasm of nerve cells (neurons) in the cerebral cortex and in the brain stem . These inclusions are abnormal aggregates of protein that reduce the formation of the messenger substance ( neurotransmitter ) dopamine , which among other things leads to the typical Parkinson's symptoms.
According to the α-synuclein pathology, post mortem neuropathological staging in four stages is common today.
clinic
Lewy body dementia is typically characterized by strong fluctuations in symptoms. Attention, concentration, alertness ( vigilance ) and other cognitive performance can vary depending on the daily form. Memory performance is usually well preserved at the onset of the illness. Overall, the disease is progressive .
Core symptoms
- Fluctuation in cognitive performance (as above)
- visual hallucinations (which patients can often reproduce in detail)
- Parkinson-like symptoms
Common symptoms
- Disturbances of REM sleep , the motor acting out of dreams is often observed (lack of motor inhibition)
- high sensitivity to neuroleptics , paradoxical reactions (e.g. increased aggressiveness)
More symptoms
- Syncope and falls
- Depression and delusion
and further clinical findings in the EEG , MRT or SPECT .
diagnosis
The clinical diagnosis is based on the current consensus criteria according to McKeith et al. posed. Criteria for the clinical diagnosis of dementia with Lewy bodies (DLB; abbreviated from McKeith et al.): If two of the core characteristics are met, one speaks of a probable DLB, and one of the core characteristics of a possible DLB.
Obligatory characteristic : Increasing cognitive disorders that are associated with impairments in the social or professional environment.
Core characteristics : Cognitive fluctuations, especially of attention, recurring, mostly detailed visual hallucinations, motor Parkinson's symptoms
Indicative features : falls, syncope, temporary disturbances of consciousness, hallucinations in other sensory modalities, delusion, REM sleep behavior disorders , neuroleptic sensitivity, decreased dopamine transporter uptake in the striatum (SPECT = single photon emission computed tomography (single photon emission tomography), PET = positron emission tomography, SEM = rapid eye movement).
Differential diagnosis of Alzheimer's disease (AD): Visual hallucinations have a high specificity for differentiating between DLB and AD (99%), the visual-constructive restrictions have a high sensitivity (74%). Cognitive fluctuations also speak in favor of DLB and against AD.
The frequent behavioral disorders in dementia sufferers have recently been called BPSD (abbreviation for "Behavioral and Psychological Symptoms of Dementia"). These include apathy (76.0%), "deviant motor behavior" (e.g. wandering around aimlessly) (64.5%), eating disorders (eating inedible things) (63.7%), irritability / instability ( 63.0%), agitation / aggression (62.8%), sleep disorders (53.8%), depression / dysphoria (54.3%), anxiety (50.2%), madness (49.5%), Disinhibition (29.5%), hallucinations (27.8%), and euphoria (16.6%).
therapy
Drug therapy is always only symptomatic. Since it is assumed that there is a pathophysiological deficiency in acetylcholine in dementia , it is treated therapeutically by inhibiting the enzyme that breaks down acetylcholine. These acetylcholinesterase inhibitors such as rivastigmine , donepezil or galantamine , which in Germany are only approved for Alzheimer's dementia , represent a possible form of therapy. Therapy should generally be started early, as they only slow down the process, but do not reverse it can. So far, the effects have only been demonstrated in studies and complex test systems. These effects are not always noticeable for the patient and their relatives and do not always have an impact on their everyday life. In Lewy body dementia, however, a clinical improvement can very often be observed, especially with regard to visual hallucinations, especially in the early stages.
Neuroleptics are rather unsuitable as the patients usually react more intensely to them with side effects. If neuroleptics are nevertheless indicated, so-called atypical neuroleptics can be tried, but in principle they have no advantages.
In some cases, non-pharmacological interventions are also favored in behavioral disorders in dementia sufferers. Only if these are insufficient should medical help be used.
Web links
- of the German Society for Neurology - accessed on September 8, 2018
- Guide to dementia from the Federal Ministry for Families, Seniors, Women and Youth - accessed on May 3, 2020
Individual evidence
- ^ Friedrich H. Lewy . On: www.whonamedit.com
- ^ FH Lewy. "Paralysis agitans. I. Pathological Anatomy ". In: M. Lewandowsky (Ed.): Handbuch der Neurologie. Berlin: Springer Verlag 1912, 920-933.
- ↑ Holdorff B. Frederick Henry Lewy (1885-1950) and his work. J Hist Neurosci 2002; 11 (1): 19-28.
- ↑ McKeith et al. Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the consortium on DLB international workshop. Neurology. 1996 Nov; 47 (5): 1113-24.
- ↑ McKeith I et al. Diagnosis and management of dementia with Lewy bodies. Neurology 2005; 65: 1863-72.
- ↑ Stechl, E., Knüvener, C. et al .: Praxishandbuch Demenz. Recognize - understand - treat . 1st edition. Mabuse-Verlag, Frankfurt am Main 2012, ISBN 978-3-86321-038-0 , p. 222 f .
- ^ McKeith et al .: Diagnosis and management of dementia with Lewy bodies. Neurology 2005; 65: 1863-1872.
- ^ P. Tiraboschi, DP Salmon, LA Hansen, RC Hofstetter, LJ Thal, J. Corey-Bloom: What best differentiates Lewy body from Alzheimer's disease in early-stage dementia? Brain , March 2006, 129 (3): 729-735, 2006; doi : 10.1093 / brain / awh725 .
- ↑ Fermann TJ et al. DLB fluctuations. Neurology 2004; 62: 181-187
- ↑ JL Cummings: The Neuropsychiatry of AD and Related Dementias . Taylor & Francis, London, 2003.
- ↑ Cohen-Mansfield J. Nonpharmacologic interventions for inappropriate behaviors in dementia: a review, summary, and critique. At J Geriatr Psychiatry. 2001 case; 9 (4): 361-381.