Alzheimer's disease
| Classification according to ICD-10 | |
|---|---|
| G30.0 † F00.0 * | Dementia in Alzheimer's disease, with early onset (type 2) |
| G30.1 † F00.1 * | Dementia in Alzheimer's disease, with late onset (type 1) |
| G30.8 † F00.2 * | Dementia in Alzheimer's disease, atypical or mixed form |
| G30.9 † F00.9 * | Dementia in Alzheimer's disease, unspecified |
| ICD-10 online (WHO version 2019) | |
The Alzheimer's disease ( AK , latin disease Alzheimer ) is a neurodegenerative disorder that occurs in its most common form in people over the age of 65 and by increasing dementia is characterized. It is responsible for around 60 percent of the approximately 24 million cases of dementia worldwide. Alzheimer's disease or Alzheimer's dementia is often referred to as Alzheimer's for short .
The disease is named after the doctor Alois Alzheimer , who first described it in 1906 after discovering characteristic changes in the brain of a deceased patient.
Differentiation: "Alzheimer's" and "Dementia"
The terms Alzheimer's and dementia can and must be clearly distinguished from one another: Dementia is the generic term for various diseases of the brain and is clearly described in the scientific discussion based on diagnostic criteria, including in the ICD-10 . Common to all dementias is the increasing loss of cognitive, emotional and social skills. Alzheimer's dementia is a form of dementia, according to the current state of scientific knowledge the most common and generally the best known form. The scientific community largely agrees that at least 60% of all dementia are based on Alzheimer's disease. Equating the terms Alzheimer's and dementia is misleading and should be avoided.
Alzheimer's dementia is one of the so-called primary dementias, in which the dementia behavior (cognitive changes, etc.) can be traced back directly to changes in the brain. Secondary dementias, on the other hand, are caused by deficiency symptoms, injuries or poisoning ( drug abuse , alcohol abuse ). In contrast to some secondary dementias, Alzheimer's dementia, like the other primary dementias ( vascular dementia , Lewy body dementia, etc.) is not reversible according to the current state of knowledge.
Occurrence of Alzheimer's disease
Characterization and symptoms in humans
It is characterized by an increasing deterioration in cognitive performance, which is usually accompanied by a decrease in the ability to cope with everyday activities , with increasing behavioral abnormalities and increased neuropsychiatric symptoms.
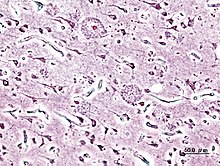
Many years before the first clinical symptoms become visible, plaques consisting of incorrectly folded beta-amyloid (Aβ) peptides form in the affected person's brain . Together with the plaques, neurofibrils , which are deposited in the neurons in the form of clusters , are characteristic ( pathognomonic ) for the disease. Alzheimer's disease is one of the tauopathies , as in this neurodegenerative disease defective tau proteins accumulate from the cell body to the axons and can no longer return to the cell body and restrict the cells to the point of inability.
The underlying changes are currently not treatable.
frequency
Alzheimer's disease almost exclusively affects people of older age. Due to the population development in the western industrial nations with aging citizens, the Alzheimer's prevalence is also increasing . About two percent of the 65-year-olds are affected, with the 70-year-olds it is already three percent, with the 75-year-olds six percent and with the 85-year-olds about 20 percent show symptoms of the disease. Over the age of 85, the proportion of those affected decreases again, as those previously ill rarely reach this age. The youngest known Alzheimer's patient fell ill at the age of 27 and died at 33. The neuronal ceroid lipofuscinosis that occurs in children and adolescents is often referred to as children's Alzheimer's, but it is a hereditary metabolic disease.
Women are significantly more likely to develop Alzheimer's than men. One reason for this is the higher life expectancy. In the last few years, the connections between fluctuations in the hormonal balance during menopause and the risk of developing Alzheimer's have been researched.
In Germany, around 1.7 million people are currently (2018) suffering from dementia, an increase to 3 million is forecast by 2050. More than 25,000 of them have not yet reached the age of 65. About 300,000 new types of dementia are diagnosed each year, at least two thirds of which are Alzheimer's.
In 2015, Alzheimer's Disease International estimates that around 46.8 million people worldwide were affected by dementia. Alzheimer's disease is also the most common form of dementia globally at around 65%. According to the evaluation of computer models, this number, which is based on population forecasts by the United Nations, is expected to increase to around 131.5 million patients by 2050.
Alzheimer's symptoms in animals
Thanks to improved veterinary care, pets are also reaching a higher age. Neuropathological changes (plaques and vascular amyloidosis ) e.g. B. in the brains of senile dogs resemble the findings of people suffering from Alzheimer's. The consequence of these processes are cognitive dysfunctions, which can lead to excessive fear, disorientation, seemingly baseless aggression, reduced or lacking learning ability and loss of house-training. The xanthine derivative propentofylline, which inhibits adenosine transport and improves hemodynamics, is used successfully in geriatric therapy with dogs.
causes
To date, the cause of Alzheimer's disease has not been fully clarified, even if there is broad, albeit not complete, consensus on the possible factors influencing the development of the disease.
Underactive in the flushing of waste materials from the brain
In the course of the discovery (2012) of the glymphatic system , a special microcircuit in the brain and spinal cord to flush out superfluous and harmful material, it became clear that this system played a key role in the development of AK - and possibly also in future prevention and treatment seems.
Deposits of beta-amyloids , the so-called senile plaques , in the cell space (interstitium) are transported away by the glyphatic system . In mice, the removal of beta-amyloids was twice as fast during sleep as during wakefulness. This has been linked to the increased risk of those with insomnia of developing Alzheimer's disease. The increase in the risk of disease in old age was also associated with the corresponding, age-related decline in performance of the glymphatic system . Certain pathogenic forms of tau proteins characteristic of Alzheimer's disease are also transported away from the intercellular space by the glyphatic system .
Genetic Risk Factors
At the genetic level, a variant in the gene for ApoE was identified, which represents a risk factor for the development of Alzheimer's disease. In addition, causal mutations were found in three different genes [ presenilin -1 and -2 and amyloid precursor protein ( APP , amyloid precursor protein)], which are considered to be the cause of the rare early subtype. The changes in all three genes mean that earlier than in the non-hereditary, sporadic form, large amounts of beta amyloid accumulate first in the association cortex (responsible for higher cognitive processes) and in the hippocampus (memory formation) and later in the entire brain. Their share in the development of Alzheimer's disease ( population attributable risk ) is estimated at a maximum of 30%. In a study of 1700 Icelandic patients, a natural mutation in the APP gene was discovered that was associated with the absence of Alzheimer's and dementia.
Inheritance
There is a genetic component in causing Alzheimer's disease. Approximately five to ten percent of these patients show a family history based on mutations of the presenilin -1 - gene (PSEN1) on chromosome 14 , the presenilin-2 gene (PSEN2) on chromosome 1 or the APP gene on chromosome 21 are due . In addition, a still unclear connection between Alzheimer's disease and the ε4 allele of apolipoprotein E (ApoE), a protein involved in cholesterol transport, could be established.
The Down syndrome with its triple complex of genetic material of chromosome 21 on which the APP gene is located, also increases the risk , of developing dementia, possibly Alzheimer's disease of developing, wherein the detection in people with this genome mutation is made more difficult by a mostly present cognitive impairment .
Furthermore, a mutation variant of the SORL1 gene has been mentioned as an increased risk factor for this disease.
A point mutation from GAA to GCA in exon 8 in the PSEN1 gene, which leads to an amino acid exchange from glutamic acid to alanine in the gene product , is responsible for an increased occurrence of FAD in the Colombian Department de Antioquia . The genetic defect is autosomal - dominant inherited. This mutation originated in a couple of Basque immigrants who settled in Colombia in the early 18th century. It is assumed that there are around 1,000 mutation carriers. The mutation is also called the paisa mutation after the name of the inhabitants of this area . The first symptoms of memory loss typically become noticeable as early as the third decade of life. Mild cognitive impairment begins at age 45 and dementia at age 50. A genetic test can be used to demonstrate the predisposition to Alzheimer's disease. These patients are particularly well suited as participants in clinical trials to test potential Alzheimer's drugs. An extensive, Phase II, long-term study has been started in patients with a Paisa mutation. They received the monoclonal antibody crenezumab prophylactically . Crenezumab is directed against beta-amyloid-40 and -42. The study started in 2013 and should run until 2020. In January 2019, however , Roche announced that the studies on crenezumab had been discontinued early because the intended effect had not been achieved.
Inflammatory processes or infection
The nun study by David Snowdon shows a strong deviation of the pathological findings in the brain (multiple Alzheimer's plaques) and the repeatedly ascertained psychological performance during lifetime. Pat McGeer suspects inflammatory processes in the brain to be the cause of the disease. Thomas Bayer sees the causal processes in the nerve cells.
Beta-amyloid proteins show a strong antimicrobial effect in vitro . One suspicion is that they arise as a defensive response to an as yet unknown infection.
A study published in January 2019 suggested a link between Alzheimer's disease and infections with the Porphyromonas gingivalis bacteria , which is associated with periodontal disease . Evidence for this is the presence of P. gingivalis and its metabolic products, the so-called gingipains, in the brains of Alzheimer's patients. Gingipaines are proteases that influence the structure of tau proteins in the study in vitro and in vivo . Infection of mice with Porphyromonas gingivalis resulted in amyloidosis . In the study, the gingipains could be inhibited with two protease inhibitors, which in turn reduced the number of bacteria in the brains of the test animals ( color mice ), blocked the production of Aβ1–42 and also reduced the inflammatory processes that led to neurodegenerative changes. The COR388 inhibitor used in the study has been in a phase I clinical study with healthy volunteers since December 2017 . Another, randomized, placebo- controlled, double-blind phase I study with Alzheimer's patients began in February 2018.
Prions as a trigger
Research suggests that Alzheimer's-like tauopathy in genetically engineered mice can be triggered by the introduction of synthetic tau fibrils into the brain.
Risk factors cholesterol, trauma, diabetes, and high blood pressure
In addition to unavoidable aging and genetic disposition, risk factors include a previous traumatic brain injury , metabolic diseases - insulin resistance and hyperinsulinemia , diabetes and high cholesterol levels, as well as diseases of the cardiovascular system - high blood pressure and strokes .
Aluminum in the brain: a consequence or cause of Alzheimer's?
Aluminum has been discussed controversially as a triggering factor in connection with Alzheimer's disease. It is a common element and, of course, may appear. a. as a trace element in food and drinking water. Additional exposures result from the use in e.g. B. Antacids ( magaldrate , hydrotalcite ), deodorants and aluminum cookware.
In an incident with aluminum sulphate in drinking water at Camelford, Cornwall, England, in July 1988, a number of people drank drinking water with high concentrations of aluminum sulphate . Studies of the long-term health effects after this incident are still not fully completed, but post-mortem studies have found particularly high levels of aluminum in the victims' brains and further studies have been commissioned to establish an association with it identify cerebral amyloid angiopathy .
In the French PAQUID cohort study from 1999 and later updates, a possible connection between aluminum deposits from contaminated drinking water and the likelihood of developing Alzheimer's was established. Accordingly, many senile plaques with elevated aluminum levels have been found in the brains of Alzheimer's patients.
According to a meta study by Ferreira et al. From 2008 out of 34 relevant studies, 68% found an association between aluminum and Alzheimer's, while 8.5% found no association. 23.5% did not come to a clear result.
The British Alzheimer's Society took the medical and scientific point of view on January 30, 2009, that the studies carried out up to 2008 had not convincingly demonstrated a causal relationship between aluminum and Alzheimer's disease.
A health assessment by the Federal Institute for Risk Assessment (BfR) from 2005 saw no connection between aluminum intake from food contact articles and Alzheimer's disease, nor did an update from 2007, but the recommendation was made that as a precaution, no acidic foods were in contact with Keep aluminum pots or foil. The results of a statement by the European Food Safety Authority (EFSA) on aluminum as a food ingredient (in the substance E131), which was published in April 2013, will be taken into account in a new statement by the BfR. Here, too, it is pointed out that the connection to Alzheimer's disease has not yet been proven, but the estimated intake amount of aluminum with daily use of aluminum-containing antiperspirants is above the weekly tolerable amount according to EFSA.
particulate matter
A study from 2018 shows a connection between fine dust (PM 2.5 ) and ozone (O 3 ) and Alzheimer's disease. 203 residents of Mexico City were examined. It was u. a. examined the incidence of tauopathies and beta amyloid . According to the study, exposure to particulate matter and ozone above the USEPA limit values can be associated with an increased risk of Alzheimer's disease.
Course of disease
Senile plaques and mitochondrial disorder

Senile plaques and fibrillary debris form in the brains of Alzheimer's patients . The protein deposits of the plaques mainly consist of the beta-amyloid peptide. The intracellularly located neurofibrillary tangles consist of the tau protein . This aggregates into fibrils if it phosphorylates more than normal, i.e. H. is occupied with phosphoric acid residues ("hyperphosphorylation"). It is not clear whether this tau phosphorylation is of a secondary nature or whether it causes disease.
In the course of the disease, the brain mass decreases due to the death of neurons; one speaks of brain atrophy . In addition, the messenger substance acetylcholine is no longer produced in sufficient quantities (among other things by a reduction in the enzyme choline acetyltransferase , which occurs in the nucleus basalis Meynert and which catalyzes the composition of acetyl-CoA and choline ), which leads to a general weakening of the brain's performance.
The beta-amyloid peptide is made from a precursor protein, the amyloid precursor protein (APP), which is an integral membrane protein . Most of this protein protrudes from the cell (located extracellularly; see extracellular matrix ), while only a small portion is located inside the cell (intracellularly). It is a type I transmembrane protein : the amino terminus is on the outside of the cell, the carboxyl terminus is inside the cell. APP is broken down by protein-splitting enzymes called secretases ( alpha-secretases , beta-secretase and gamma-secretase ), which can lead to the release of the beta-amyloid peptide from the precursor protein. There are basically two ways in which APP can be split:
- The non-amyloidogenic route: APP is cut by an α-secretase. This cut takes place within the part of APP that contains beta amyloid. This prevents the formation of beta amyloid. A large extracellular portion is released, the function of which has not yet been finally clarified.
- The amyloidogenic pathway: APP is cut first by β-secretase and then by γ-secretase. This cut, which occurs within the transmembrane domain, results in the release of beta-amyloid.
Both processes can take place in parallel in nerve cells . The beta-amyloid peptides formed by β- and γ-secretase vary in length. The main type is beta amyloid-40 (40 amino acids long) while a small fraction, beta amyloid-42, is 42 amino acids long. The length of the beta-amyloid is of central pathological importance, since the longer beta-amyloid-42 has a much higher tendency to aggregate than the smaller beta-amyloid-40.
Candidates for α-secretase are the proteases ADAM 10, ADAM17 / TACE and for β-secretase BACE1. The γ-secretase consists of a high molecular weight complex of the proteins presenilin 1 or 2, PEN-2 , APH-1 and nicastrin , although it is not clear whether other proteins are involved.
In Alzheimer's disease, the function of the mitochondria is disturbed. A blockage of the respiratory chain at complex IV leads to an excessive production of radicals , which can damage the cell. Whether this blockade is a consequence of the excessive beta-amyloid production or whether beta-amyloid is excessively produced as an antioxidant against this newly created oxidative stress remains open to this day.
early detection
As early Alzheimer's detection, u. a. an examination of the brain's performance using various tests is offered or an magnetic resonance tomography (MRI). Both are private services, i.e. IGeL (Individual Health Service). The IGeL monitor of the MDS ( Medical Service of the Central Association of Health Insurance Funds ) has rated the brain performance check for the early detection of dementia as “generally negative”, as no real benefit is discernible. Detecting it early cannot prevent or reduce dementia, and since only half of people with mild dementia develop severe later, patients may become unnecessarily concerned. The S3 guideline “Dementia” from 2016 also speaks out against an examination of people without symptoms or symptoms.
For similar reasons, the IGeL-Monitor also rated magnetic resonance imaging (MRI) for the early detection of Alzheimer's dementia with a “negative tendency”. Magnetic resonance imaging (MRI) is a valuable procedure that can help diagnose Alzheimer's disease. But there are no studies on the benefit of early detection by MRI.
If you suspect Alzheimer's dementia, the statutory health insurance companies will pay for the clarification of the suspicion, possibly also with an MRI. A brain performance check is a health insurance benefit for people who have a reasonable suspicion of dementia, for people between 70 and 80 years of age with certain other diseases, and for people over 80 years of age in general. The offers of self-pay service were taken up critically in various media.
Recognizing the disease through people's behavior
First warning signs
The American National Institute on Aging has formulated seven warning signs that can indicate the onset of Alzheimer's disease and that should prompt people in the immediate vicinity to seek medical advice:
- The sick person repeats the same question over and over again.
- The sick person tells the same short story over and over again.
- The sick person no longer knows how certain everyday tasks such as cooking, playing cards, handling the TV remote control work.
- The sick person has lost the safe handling of money, transfers, bills and the like.
- The sick person can no longer find many objects or he puts them in unusual places (unintentional hiding) and suspects other people to have taken the missing object away.
- The sick person persistently neglects his appearance, but denies this.
- The sick person answers questions by repeating the question asked.
The course is divided into different stages, in each of which different physical and psychological restrictions are in the foreground.
Pre-dementia stage
Already eight years before Alzheimer's can be diagnosed with certainty, minor abnormalities can be detected in neuropsychological tests. Short-term memory problems and related problems grasping new information are easiest to spot. Under certain circumstances, there may already be slight impairments in understanding speech and in pursuing personal goals. Affect impairments such as depression and indifference are common.
Recognizing the disease through scientific methods
In April 2011, the National Institute on Aging and the US Alzheimer's Society published new recommendations for diagnosing Alzheimer's disease. However, these revised diagnostic criteria are still considered unsuitable for everyday clinical practice and should therefore be reserved for specialized centers. The updated guidelines distinguish between three progressive stages:
- The preclinical stage of Alzheimer's disease,
- the stage of mild cognitive impairment (“Mild Cognitive Impairment”, MCI) and
- the stage of dementia as a result of Alzheimer's disease.
A relatively reliable in-vivo diagnosis has so far only been possible in the stages of dementia and MCI - through a combination of anamnestic findings, neuropsychological tests, laboratory tests (liquor biomarkers) and imaging findings. However, this only applies to a very limited extent for the MCI stage, since the imaging methods required here, especially direct amyloid imaging using positron emission tomography (PET and radioactive tracers such as Florbetaben ) and the various functional magnetic resonance imaging (fMRI) methods, are very promising apply, but are usually too complex and expensive for everyday clinical use. Many questions about the interpretation of the findings have also not yet been answered. Diagnosis using positron emission tomography (PET) is now still in clinical development. Certain substances, so-called PET tracers , can attach to the amyloid beta aggregates, which are increasingly formed in the brain in Alzheimer's patients. The first tracer to be investigated in clinical studies was the substance Pittsburg B with the carbon isotope C-11. Because of its short half-life of 20 minutes, tracers based on fluorine-18 with a half-life of 109 minutes were developed. The promising tracers with this isotope are florbetapir and flutemetamol in addition to florbetaben. The measurement of biomarkers (beta amyloid, total tau protein, phosphorylated tau, amyloid precursor proteins) in the CSF requires a lumbar puncture , i.e. an invasive procedure. There is no standardized, everyday blood test.
Retinal vascular analysis could offer a possibility of early detection . In 2019, an Italian study was published in which the reaction of the smallest arteries and veins in the retina to the light stimulus differed in a characteristic way from that of the healthy study participants in Alzheimer's patients and in study participants in the early stages of the disease. The behavior of the small retinal vessels evidently reflects the vascular situation in other organs. In patients with Alzheimer's disease and MCI, the significantly changed behavior of the retinal vessels showed an inverse correlation with the level of beta-amyloid proteins in the spinal fluid ( cerebrospinal fluid ).
In everyday clinical practice, the suspected diagnosis of Alzheimer's disease is made through special tests to assess the memory, through the so-called external anamnesis, the clinical course and generally available imaging methods such as computed tomography or magnetic resonance tomography . However, the diagnosis can only be definitively confirmed after the patient's death by performing a histological examination of the brain.
The ICD-10 diagnosis code differentiates between G30.0 Alzheimer's disease with an early onset and G30.1 Alzheimer's disease with a late onset based solely on age when recognizable symptoms appear.
Alzheimer's disease must always be differentiated from other, similar psychological and neurological disorders, such as
- normal age-related forgetfulness
- Denial or avoidance behavior
- mild cognitive disorder of old age (classified under the code ICD-10 F06.7 organic mental disorders )
- Depression in older people with inhibited thinking (possibly with additional cognitive disorders in the sense of a second illness)
- Deprivation symptoms or hospitalism and regression in old people's homes
- simple aphasia
- simple mutism
- severe autism ( Kanner syndrome ) with mutism
- severe neurological syndromes such as Apallic syndrome , locked-in syndrome or akinetic mutism
- Brain tumors , brain injuries that led to organic amnesia syndrome (ICD-10 F04)
- Disorders of metabolism (e.g., hypoglycemia in diabetics )
- stroke
- Normal pressure hydrocephalus
- delirium
- Psychoses and delusions (for example, schizophrenia , mania, or psychotic depression )
- other forms of dementia
- Speech disorders, word finding disorders and total loss of language.
Early and intermediate stages
In most patients, deficits in learning and memory retention lead to the diagnosis. While in long-term memory familiar activity processes and emotional experiences are mostly still present, learning and short-term memory are the most restricted.
The linguistic ability of those affected is reduced overall, which is expressed in the flow of language and a reduced vocabulary. In principle, however, they are able to communicate their thoughts and ideas to other people in a suitable manner.
Fine motor skills already show certain insecurities that can be seen in activities such as writing, painting or dressing. When the disease transitions to the intermediate stage, some patients are still able to organize their everyday lives independently, but they are already dependent on support for complicated or complex activities. A typical symptom in this phase are triple steps.
Advanced stage
In the advanced stage, the patients forget well-known skills and no longer recognize people close to them and everyday objects.
Even with patients who were peaceful before the illness, outsiders can experience outbursts of anger and violence that are seemingly unfounded. Feelings of guilt and general inner self-reflection decrease more and more in the further course, just as many human behavior patterns only seem to run automatically.
The muscles continuously break down, which leads to further language problems, urinary or fecal incontinence and an ever-decreasing mobility up to bedridden. Without support, those affected can no longer cope with their everyday lives and need support even with simple activities. The disease progresses to death, which in so debilitated patients is often triggered by pneumonia or a heart attack .
forecast
After the diagnosis of Alzheimer's has been made, the remaining life expectancy is about seven to ten years, although there are also cases in which the end stage is reached after four to five years. On the other hand, there were patients who lived for over 20 years.
Preventing the disease
Research on future vaccines
There is much research into a vaccination that is supposed to prevent the disease or at least prevent the progression of the disease.
So one is beta amyloid immunotherapy based on the monoclonal antibody Bapineuzumab already in clinical trials investigated. The US companies Johnson & Johnson and Pfizer announced in August 2012 that they were discontinuing clinical development of bapineuzumab. The monoclonal antibody, which was supposed to remove the beta-amyloids from the brains of dementia patients, did not meet expectations in a second phase III study either.
A research group from Göttingen has shown that vaccination with the new monoclonal antibody (9D5) prevents the disease from progressing in mice. This antibody is directed against a certain molecular structure in the brain and prevents it from producing the protein pyroglutamate-Abeta. This protein forms toxic clumps ( oligomers ) that accumulate in the nerve cells and blood vessels of the brain of people with Alzheimer's disease and thus cause the damage that causes the disease. Use in humans is the subject of further research.
Blood pressure, exercise, diet and environmental influences
Various preventive measures against typical lifestyle diseases also seem to reduce the likelihood of developing Alzheimer's. The data situation and scientific acceptance of various food supplements, behavioral guidelines, diet suggestions, environmental influences and initial illnesses as the cause of the disease vary. It is important that measures that are able to prevent the occurrence of the disease are not necessarily suitable for positively influencing the course of an Alzheimer's disease that has already been diagnosed. There are many observational studies, but only a few controlled randomized studies , which prove the effectiveness of the measures. Until 2006, according to these strict study criteria, a significant reduction in the risk of Alzheimer's was only found for controlling blood pressure. In the same way, there is still a lack of proven preventive drugs.
Sufficient exercise , a healthy diet with a high proportion of phytochemicals such as the antioxidant quercetin , unsaturated fatty acids, B vitamins - especially folic acid - as well as not using nicotine could have a positive effect. The vitamins folic acid, B6 and B12 break down the toxic amino acid homocysteine into harmless substances. Scientific studies show that homocysteine is a decisive contributor to arteriosclerosis and causes the brain to age more intensely: People with high homocysteine levels are twice as likely to develop Alzheimer's disease. In addition, a low vitamin B12 level is associated with a higher rate of brain atrophy. The atrophy rate of the brain in patients with mild cognitive impairment can, however, be reduced by 29.6 percent through treatment with folic acid, vitamins B12 and B6.
In a follow-up study from January 2013, the researchers from Oxford University found that the external intake of high-dose vitamin B12 in conjunction with folic acid significantly slowed the reduction in brain volume in people with an increased Alzheimer's risk compared to the control group over a period of two years could be. David Smith, Professor Emeritus of Pharmacology at Oxford University who led the study, said, "It's a big effect, much bigger than we dared dream." Mental activity appears to be just as beneficial as mentally demanding activity. High blood pressure should be detected as early as possible and treated well to reduce the risk of dementia. Scientific studies ( Beyreuther et al.) Have shown that an elevated cholesterol level increases the risk of developing Alzheimer's.
According to the Berliner Zeitung, there should be indications that caffeine (coffee, tea, etc.) has a protective effect against the development of Alzheimer's disease.
Antioxidants, green and black tea
In vitro studies showed that the antioxidant epigallocatechin gallate (EGCG) found in green tea can prevent plaque formation. Other studies suggest that EGCG can also dissolve the plaques. In animal experiments with mice it could be shown that after six months of EGCG treatment the plaque load in the cortex, hippocampus and in the entorhinal cortex was reduced by 54%, 43% and 58% respectively. Another study examining the effects of EGCG on Alzheimer's disease is being carried out at the Charité in Berlin. Studies from 2011 showed that theaflavin components of black tea can also prevent the formation of plaques and dissolve existing plaques.
Medical treatment of sick people
There is currently no cure for Alzheimer's disease. The positive effect of the drugs currently approved for the treatment of dementia on existing symptoms is only relatively minor; they cannot stop the disease from progressing. In 2006, the American Association for Geriatric Psychiatry published a consensus paper on the treatment of Alzheimer's disease. According to a preclinical study by Case Western Reserve University in February 2012, the chemotherapy drug bexarotene was able to dissolve up to 75% of the β-amyloid plaques in mice and also to revise symptoms of the disease, such as memory loss. Subsequent pre-clinical trials by other research groups could not confirm the promising results. Bexarotene is not approved for the treatment of Alzheimer's disease.
Acetylcholinesterase inhibitors
The drugs ensure that acetylcholine is broken down more slowly in the brain and is therefore present in higher concentrations. This is to counteract the reduction in the acetylcholine level caused by the death of neurons that produce this messenger substance. Acetylcholine is a neurotransmitter which occurs in many cases in the association cortex and which sends out efferent nerve connections to the hippocampus (responsible for memory formation which is damaged in Alzheimer's patients). This explains why the hippocampus itself is not cholinergic , but therapy with acetylcholinesterase inhibitors still stimulates its activity. Representatives of this group of active ingredients are galantamine , donepezil , rivastigmine and the active ingredient huperzine A , which is currently (as of 2018) being clinically researched. The acetylcholinesterase inhibitors are approved for mild to moderate Alzheimer's dementia, not for severe. The effectiveness of the therapy is discussed. The ideal study shows that both the application of patches and the oral administration of rivastigmine significantly improve the cognitive abilities of patients compared to placebo. But there are also studies that show that acetylcholinesterase inhibitors have little effect. The extent of the benefits of the preparations is therefore controversial among German psychiatrists.
Ibuprofen and other nonsteroidal anti-inflammatory drugs
In 1995 retrospective studies found that rheumatism patients have a significantly reduced risk of developing Alzheimer's disease, or that the disease breaks out later in them than in non-rheumatoid patients. It was concluded that this effect on the non-steroidal anti-inflammatory drugs (in English language publications (NSAIDs) nonsteroidal anti-inflammatory drugs called (NSAID)) is due to taking these patients.
In some transgenic animal models , a reduction in amyloid beta plaques was found when ibuprofen was administered .
In humans, there are no data from randomized double-blind studies that show a reliable mode of action of ibuprofen and other nonsteroidal anti-inflammatory drugs. Due to the not insignificant side effects that are to be expected with a long-term prophylactic intake of ibuprofen, uncontrolled intake is not recommended. The doses of nonsteroidal anti-inflammatory drugs necessary for the possible prevention of Alzheimer's disease are considerably higher than for normal pain treatment. The non-steroidal anti-inflammatory drugs are suspected of causing cardiovascular problems if they are taken long-term and in high doses.
A number of clinical studies in Alzheimer's patients are currently ongoing with ibuprofen and derivatives of ibuprofen.
Activation of ABC transporters
Using the mouse model , it could be shown that the use of thiethylperazine and thiethylperazine derivatives with an ABC transporter activating effect enables the treatment of neurodegenerative diseases as well as the function of the transporter ABCC1 for diagnosis and therapy monitoring of M. Alzheimer's (and M. Parkinson ). These active ingredients could delay the course of Alzheimer's dementia and Parkinson's disease by several years. The drug is in clinical phase II under EudraCT Number: 2014-000870-20.
NMDA receptor antagonist
The influencing of the messenger substance glutamate , the most common excitatory messenger substance in the central nervous system that is involved in learning processes and memory functions, was approved throughout Europe in 2002 and in the USA in 2003. The only representative of this class of active ingredients to date is memantine . This is an NMDA receptor - antagonist ( N -methyl- D aspartate receptor antagonist) and to normalize the increased in Alzheimer's dementia glutamatergic signaling. Study results show that memantine leads to an overall slight improvement in cognitive disorders and impaired everyday activities after six months in moderate to severe illness. Memantine is approved for moderate to severe Alzheimer's dementia, not mild.
Ginkgo biloba
The special extract EGb 761 is approved for the symptomatic treatment of "brain-organically caused mental performance losses in dementia syndromes". The standard dose is 240 milligrams per day. In addition to this extract, there are a number of other preparations containing ginkgo biloba, which differ in their exact composition. A meta-analysis of the available study results from 2007 came to the conclusion that the indications that ginkgo preparations had a beneficial effect on the cognitive abilities of Alzheimer's patients were inconclusive and not very convincing; in a previous publication the same authors had described ginkgo as promising.
A large, double-blind, long-term study (GEM study) was conducted in the United States to determine whether ginkgo can be used effectively to prevent Alzheimer's disease. The results published in 2008 showed no significant difference between the ginkgo preparation (120 mg twice daily) and placebo - while 246 people in the placebo group developed dementia, it was 277 people in the ginkgo group. Another analysis of the GEM study, published at the end of 2009, also showed that the special extract could not stop a mental loss of performance in the average age of almost 80-year-old patients. In their discussion of the results, the authors of the study point out, on the one hand, that the cognitive tests used may not have been suitable for recognizing the effects of the preparation. On the other hand, the study participants are said to have been unusually healthy and educated, which makes the occurrence of cognitive weaknesses relatively unlikely. A literature analysis by scientists at the Charité in 2010 came to the conclusion that the special extract was more effective than placebo, but the effect was moderate and the clinical significance of this effect, as in general with antidementia drugs, was very difficult to determine.
In 2008, the German Institute for Quality and Efficiency in Health Care examined publicly accessible studies as part of a drug evaluation as well as data provided by drug manufacturers on the ginkgo-containing preparations available in Germany. It came to the conclusion that there is proof of a benefit for the therapy goal “activities of daily living”, provided that 240 mg of extract are taken daily. For the therapy goals “cognitive abilities” and “general psychopathological symptoms” as well as for the relatives-relevant therapy goal “quality of life of the (caring) relatives” (measured by the emotional stress of the relatives) there is only one indication of a benefit with the same dosage .
Further studies suggest that ginkgo leaves contain more pharmacologically effective substances that may allow a causal treatment of preclinical Alzheimer's disease.
cannabis
A systematic review published by the Cochrane Collaboration in 2009 concluded that there was no evidence that cannabinoids were effective in preventing or ameliorating symptoms of Alzheimer's disease. The status at that time has not changed since then (status January 2016).
insulin
Noteworthy is the effect that insulin , administered as a nasal spray (presumably through direct contact with the central nervous system), can positively influence the course of Alzheimer's disease.
Vitamins and food supplements
A new randomized clinical study shows that high doses of vitamin E can slightly delay the progression of the need for care. In contrast, the antidementia drug memantine disappointed in this study. The primary endpoint was the ADCS-ADL (Alzheimer's Disease Cooperative Study - Activities of Daily Living), which records everyday practical skills. Vitamin E was able to delay the decline in ADCS-ADL somewhat, even if the significance was only reached after an adjustment. In addition, 128 of 613 participants died before the study was completed. The study is part of a series of studies with different statements on the effectiveness of vitamin E in Alzheimer's disease. Because of the minor effect and the possible increased mortality , high-dose vitamin E administration cannot yet be generally recommended.
In a two-year European LipiDiDiet study at eleven clinics with 311 patients in 2017, it was possible to prove that the combined addition of the omega-3 fatty acids docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA), various vitamins ( B 12 , B 6 , C , E and folic acid ) and other nutrients such as choline , uridine monophosphate and selenium for the food of sick people have significantly improved cognitive and functional performance in everyday life. Compared to the control group, the researchers observed a 45% lower deterioration in the clinical assessment of dementia. MRI imaging showed 26% less hippocampal shrinkage in supplemental patients compared to control patients.
Psychotherapeutic treatment
Symptoms such as restlessness, depressive mood or agitation and aggressiveness that may occur in the course of the illness can be treated with the help of psychotherapy and psychotropic drugs. In addition, since the beginning of the 21st century, non-pharmacological interventions in behavioral disorders have been favored by dementia patients.
Code of Conduct
An American study found that people who did a less mentally demanding job between the ages of 20 and 50 were more likely to develop Alzheimer's disease. The threshold at which symptoms are noticeable may be lowered.
Current scientific work suggests that even light but regular physical activity (walking, gardening) may protect against the development of Alzheimer's disease. It is assumed that the positive effects of movement on vascular risk factors (high blood pressure, lipid metabolism disorders and diabetes mellitus) reduce vascular damage in the brain and thus - indirectly - hinder the occurrence of dementia symptoms.
The adaptation of living spaces to the changed possibilities and needs can make everyday life easier for those affected and caregivers. The simplification of work processes and the labeling of objects help the patient to obtain a higher degree of independence. Changes in familiar processes or the environment often annoy the patient unnecessarily, while well-lit rooms, appropriate breaks and limited demands make the patient feel safe. Appropriate social and visual stimulation can lead to an improvement in attention and orientation ; for example, an increase in food intake can be achieved if strikingly colored table accessories are used, which Alzheimer's patients can better perceive with reduced contrast recognition.
Advice and support in everyday life
Specialized nurses
Specialized nurses can offer specific support in everyday life at home or in the home.
Occupational therapy
The goal of occupational therapy is the greatest possible independence in everyday life. On home visits, occupational therapists can train relatives and give recommendations on fall prevention in the home. In the home, occupational therapists can support those affected in continuing to carry out meaningful activities. In occupational therapy group therapies, those affected can train cognitive skills.
history
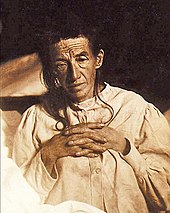
In November 1906, the German psychiatrist and neuropathologist Alois Alzheimer described the first case of what later became known as Alzheimer's disease in a lecture to colleagues. He had already met the patient Auguste Deter in November 1901 after she was admitted to the Frankfurt neurological clinic. He carefully accompanied the then 51-year-old patient and recorded her behavior. When Auguste Deter died in April 1906, Alois Alzheimer had meanwhile become laboratory manager at Emil Kraepelin in Munich. As he was interested in research into dementia, he had Emil Sioli's brain of the deceased patient sent to him and examined it. His lecture in November 1906 caused no reactions. The next year he published his findings in the article About a strange disease of the cerebral cortex in the Allgemeine Zeitschrift für Psychiatrie .
In the following five years, eleven similar cases were reported in the medical literature; some already using the term Alzheimer's disease . The official name goes back to the psychiatrist Emil Kraepelin. In the eighth edition of his textbook on psychiatry from 1910, he named the disease after Alois Alzheimer.
Since the patient being cared for by Alois Alzheimer was relatively young, he described the disease as a presence of dementia . Only later did it become apparent that the same histological changes also occur in older dementia patients. To distinguish it from real (present) Alzheimer's disease , the form of the disease in older people is called senile dementia of the Alzheimer's type (SDAT or DVAT).
In 1997, original microscope preparations from Alois Alzheimer's work in Munich were rediscovered and re-evaluated. In 2012, a presenilin mutation was detected in the material .
Social perception
Prominent Alzheimer's sufferers
In the 1970s people began to talk more openly about age-related diseases. In 1976 Harold Wilson (1916-1995) announced his resignation as Prime Minister of England because he had noticed that he was suffering from the onset of Alzheimer's. This became known in the 1980s. The diseases of Rita Hayworth († 1987), the boxer Sugar Ray Robinson (1921–1989), the footballer Helmut Schön (1915–1996), the long-time director of the New York Metropolitan Opera Rudolf Bing (1902–1997), Iris Murdoch (1919–1999), Charles Bronson († 2003), Helmut Zacharias († 2002) and Peter Falk († 2011) made it clear that it can affect anyone. Ronald Reagan (1911–2004), US President from 1981 to 1989, admitted to his Alzheimer's disease in a letter to the American public in 1994 (at the age of 83): “I am now starting the journey that will take me to the sunset of my life with the certainty that a bright dawn will dawn over America again and again. "
After the English fantasy author Terry Pratchett († March 12, 2015) was diagnosed in 2007, he donated one million US dollars to the 'Alzheimer Research Trust'. In this context, Pratchett led a campaign against the ban on euthanasia in Great Britain, and he also produced the BBC documentary Choosing to Die .
In March 2008, Tilman Jens made his father Walter Jens (1923-2013) dementia of the Alzheimer's type public. Two months later Ursula von der Leyen made the Alzheimer's disease of her father, the former Prime Minister of Lower Saxony Ernst Albrecht (1930-2014), public.
The suicide of Gunter Sachs in May 2011 again drew public attention to the subject of Alzheimer's. In February 2012, Rudi Assauer went public with his Alzheimer's diagnosis.
In July 2012, the Colombian writer Gabriel García Márquez , who was awarded the 1982 Nobel Prize for Literature, declared that he had dementia. Márquez died on April 17, 2014. In October 2015, FC Bayern Munich announced in a press release that footballer Gerd Müller suffered from Alzheimer's disease and had been cared for in a specialist nursing home since February 2015.
literature
In literary terms, the writer Arno Geiger processed his father's Alzheimer's disease in the non-fiction book The Old King in His Exile , for which the author was nominated for the Leipzig Book Fair Prize in 2011 and which earned him an honorary award from the German Hospice and Palliative Care Association .
The novel Hirngespinste by J. Bernlef , first published in 1984 under the title Until it is bright again and reissued in 2007, describes the inner world of experience of an Alzheimer's patient.
In 1997, the author Martin Suter published the novel Small World on the subject of senile dementia , which was made into a film with Gérard Depardieu and Alexandra Maria Lara in 2010.
John Bayley, Iris Murdoch's widower, published his memories of Alzheimer's disease in 1999 in "Elegy for Iris", which was filmed in 2001 with Kate Winslet and Judi Dench as Iris Murdoch.
The activist Helga Rohra (* 1953), who was diagnosed with Lewy body dementia at the age of 54, campaigns for the rights of people with dementia and in 2011 published the book Stepping Out of the Shadow - Why I stand up for our rights as people with dementia .
The Spanish artist Paco Roca drew a comic about an Alzheimer's story under the title Head in the Clouds , this graphic novel was published in 2013 by Reprodukt-Verlag in Berlin . The book is about sick people in an old people's home. “The story thrives on authentic details that Roca collected from his friends and relatives as well as through research in a retirement home. A narrative unfolds that takes comic sides from the disease without downplaying its tragedy, ”said Ralph Trommer in his review in the daily newspaper (taz) on November 4, 2013. There is a cartoon adaptation of Kopf in den Wolken with the Title Wrinkles .
Sarah Leavitt brought out the comic The big mess - Alzheimer's, my mother and I in 2013 at Beltz-Verlag in Weinheim .
The Austrian author and social pedagogue Maria Seisenbacher worked on the subject of Alzheimer's disease in the form of poetry with her volume of poems Sitting calmly with sturdy shoes (2015).
In March 2016 the journalist Inge Jens published the non-fiction book Slow Disappearance: From Living with a Dementia Sufferer about the dementia of her husband Walter Jens, a former Tübingen rhetoric professor, in Rowohlt Verlag .
Film and theater
In the play I have to see if I'm there , developed by the director Barbara Wachendorff, older actors with dementia play on stage. The focus of the piece, which was nominated for the Der Faust Prize in 2006, is the world of those affected, their perception of the present and the past. Barbara Wachendorff also wrote the play Anderland - A trip without oars to the land of dementia , which premiered in May 2012 in the Stollwerck community center (Cologne).
In 2009, the director Iain Dilthey released the episode film One Day… , comprising three stories of dementia , with the actors Horst Janson , Annekathrin Bürger and Heinrich Schafmeister . The feature film is part of a film guide DVD box from the LVR Center for Media and Education in Düsseldorf.
From an old couple who cope with the stroke, and the consequent progressive dementia of the wife must, the film tells Amour - Love from director Michael Haneke , 2012 for the relationship drama at the film festival in Cannes , the Palme d'Or was awarded.
The episode film When yesterday comes tells four different stories on the subject of dementia in 77 minutes, realized by the four Taiwanese directors Hsiu Chiung Chiang, Singing Chen, Wi Ding Ho and Ko Shang Shen.
In the documentary Forget Mine not from 2012, the director David Sieveking portrayed his mother who had Alzheimer's disease.
In his play Dementia, Depression and Revolution , which premiered in 2013 at the Maxim Gorki Theater in Berlin, the director Armin Petras also thinks about age-related amnesia, in fragmentary sentences that symbolize mental decay, playing with statements about dementia Patients, relatives and medical professionals. "He pours coffee on the plate, bread in the coffee, newspaper is dipped into the soda," reads an excerpt from the theater text.
The television film Die Auslöschung tells the story of a great late love between a restorer, played by Martina Gedeck , and an art historian, played by Klaus Maria Brandauer . Their relationship changed when he was diagnosed with Alzheimer's disease. A foster relationship gradually emerges from an equal partnership, but the loving bond between the two remains (broadcast on Das Erste on May 8, 2013).
The director Thomas Liesen produced in 2013 under the title of life, love, forget ... a three-year long-term documentation of the first . A family of three was portrayed confronted with the genetic Alzheimer's disease of their 42-year-old mother. The film deals with the development of the disease from the diagnosis in the early stage to the final stage and describes the resulting stresses and restrictions on the family in everyday life.
In the German tragic comedy Honig im Kopf (2014) by and with Til Schweiger , Schweiger deals with the topics of Alzheimer's and dementia together with his daughter Emma Schweiger and Dieter Hallervorden .
Still Alice - My Life Without Yesterday (Original Title: Still Alice) with Julianne Moore in the lead role is an American-French film drama from 2014 (released in Germany in 2015). It is based on the novel of the same name by the writer Lisa Genova and deals with the course of an early onset variant of Alzheimer's disease.
Challenge for politics and society
By now, many know that Alzheimer's disease is the most common form - responsible for 50 to 80 percent of cases - is mental decline. In second place is vascular dementia: circulatory disorders caused by strokes or narrowed and calcified arteries can destroy the brain to the point that dementia occurs. The two types of dementia often overlap.
Alzheimer's disease is also considered to be a burden on the health system . Since the number of very old people has risen sharply and continues to grow, the number of sick people continues to increase. Treatment costs are a growing financial challenge for health and long-term care funds.
See also
literature
- Alois Alzheimer: About a strange disease of the cerebral cortex. Lecture (November 3rd) at the meeting of south-west German insane doctors in Tübingen on November 3rd and 4th, 1906. Alzheimer's report in Allg. Journal of Psychiatry and Mental Forensic Medicine, 1907, pp. 146–148.
- TA Bayer, O. Wirths: Alzheimer's dementia. Molecular pathology, animal models, and therapeutic strategies. In: The neurologist. 79 (Suppl 3), pp. 117-128.
- Anne Eckert: Alois Alzheimer and Alzheimer's disease. In: Pharmacy in our time . Volume 31 (4), 2002, pp. 356-360.
- Hans Förstl, Alexander Kurz, Tobias Hartmann: Alzheimer's dementia. In: Hans Förstl (Ed.): Dementia in theory and practice . 3. Edition. Springer, Berlin a. a. 2011, ISBN 978-3-642-19794-9 , pp. 47-72.
- Kurt Jellinger (Ed.): Alzheimer's - Milestones from a hundred years of scientific and clinical research. Akademische Verlagsgesellschaft AKA, Berlin 2006, ISBN 3-89838-077-7 .
- Frank Jessen (Ed.): Manual Alzheimer's Disease. Basics - Diagnostics - Therapy - Care - Prevention. De Gruyter, Berlin 2018, ISBN 978-3-11-040345-9 .
- Cornelia Stolze : Forget Alzheimer's! The truth about a disease that isn't. Kiepenheuer & Witsch, Cologne 2011, ISBN 3-462-04339-0 .
- Randall J. et al .: Clinical and Biomarker Changes in Dominantly Inherited Alzheimer's Disease. In: New England Journal of Medicine . 2012, p. 120723122607004, doi: 10.1056 / NEJMoa1202753 .
- Michael Jürgs : Alzheimer's: Searching for clues in no man's land. Bertelsmann Taschenbuch, Munich 2006, ISBN 978-3-570-00934-5 .
- Margret Lock: The Alzheimer Conundrum: Entanglements of Dementia and Aging. Princeton University Press 2013, ISBN 978-0-691-14978-3 .
Web links
- Macroscopic specimen of an Alzheimer's patient and histological specimen
- Guide to dementia from the Federal Ministry for Families, Seniors, Women and Youth
- Infoportal Dementia Website of the Alzheimer Society Baden-Württemberg
- The major common diseases: Alzheimer's TV documentary by ARD as a YouTube video (41:36 min.), Description at 3sat.de
Individual evidence
- ↑ CP Ferri et al .: Global prevalence of dementia: a Delphi consensus study. In: Lancet , Volume 366, Number 9503, December 2005, pp. 2112-2117, doi: 10.1016 / S0140-6736 (05) 67889-0 . PMID 16360788 . PMC 2850264 (free full text).
- ↑ Elisabeth Stechl, Catarina Knüvener et al .: Praxishandbuch Demenz. Recognize - understand - treat . Mabuse-Verlag, Frankfurt am Main 2012, ISBN 978-3-86321-038-0 .
- ↑ R. Mahlberg, H. Gutzmann (Ed.): Recognize, treat and care for dementia diseases . Deutscher Ärzte-Verlag, Cologne 2009, ISBN 978-3-7691-0563-6 .
- ^ Sabine Engel: Alzheimer's and dementias. Support for relatives . Trias-Verlag, Stuttgart 2012, ISBN 978-3-8304-3983-7 .
- ↑ R. Mahlberg, H. Gutzmann (Ed.): Recognize, treat and care for dementia diseases . Deutscher Ärzte-Verlag, Cologne 2012, ISBN 978-3-7691-0563-6 .
- ↑ Script ( Memento from September 21, 2008 in the Internet Archive ) (PDF; 612 kB) of the program Quarks & Co on the subject of Alzheimer's
- ↑ Alexandra Bröhm: Why women get Alzheimer's more often. In: welt.de. Axel Springer SE, May 31, 2016, accessed on December 30, 2019 .
- ↑ Jane Gilmore: A possible 'link' between menopause and Alzheimer's is scaring women, including me. In: The Sydney Morning Herald. June 7, 2019, accessed December 30, 2019 .
- ↑ German Alzheimer's Society e. V .: The frequency of dementias. (PDF) Info sheet 1. In: deutsche-alzheimer.de. June 2018, accessed August 9, 2019 .
- ^ World Alzheimer Report 2015. The Global Impact of Dementia. (PDF) An analysis of prevalence, Incidence, cost and trends. Alzheimer's Disease International (ADI), August 2015, accessed August 9, 2019 .
- ↑ D. Kapl, KA Rudolphi: New pharmacological aspects to the neurological profile of propentofylline. In: Tierärztliche Praxis (26) (K), 1998, pp. 317–321
- ↑ "The causes of Alzheimer's disease have not yet been fully clarified. Research so far shows that several factors are involved in its development." In: Elisabeth Stechl, Catarina Knüvener et al .: Praxishandbuch Dementia. Recognize - understand - treat . Mabuse-Verlag, Frankfurt am Main 2012, ISBN 978-3-86321-038-0 . , P. 192
- ↑ "Although the etiology of Alzheimer's dementia must ultimately still be described as unexplained, there has been a significant increase in knowledge in the pathology of the disease in recent years, primarily on the basis of genetic and molecular biological studies." In: R. Mahlberg, H. Gutzmann (Ed.): Recognize, treat and care for dementia diseases . Deutscher Ärzte-Verlag, Cologne 2009, ISBN 978-3-7691-0563-6 . , P. 11 f.
- ↑ a b J. J. Iliff et al .: Impairment of glymphatic pathway function promotes tau pathology after traumatic brain injury. In: The Journal of neuroscience: the official journal of the Society for Neuroscience. Volume 34, number 49, December 2014, pp. 16180–16193, doi: 10.1523 / JNEUROSCI.3020-14.2014 , PMID 25471560 , PMC 4252540 (free full text).
- ↑ JM Tarasoff-Conway et al .: Clearance systems in the brain-implications for Alzheimer's disease. In: Nature reviews. Neurology. Volume 11, number 8, August 2015, pp. 457-470, doi: 10.1038 / nrneurol.2015.119 , PMID 26195256 , PMC 4694579 (free full text) (review).
- ↑ Dementia of the Alzheimer's type (DAT) - diagnosis and therapy
- ^ T. Jonsson et al .: A mutation in APP protects against Alzheimer's disease and age-related cognitive decline. In: Nature. Volume 488, number 7409, August 2012, pp. 96-99, doi: 10.1038 / nature11283 . PMID 22801501 .
- ↑ E. Rogaeva et al .: The neuronal sortilin-related receptor SORL1 is genetically associated with Alzheimer's disease. In: Nature genetics. Volume 39, Number 2, February 2007, pp. 168-177, doi: 10.1038 / ng1943 . PMID 17220890 . PMC 2657343 (free full text).
- ↑ F. Lopera et al .: Clinical features of early-onset Alzheimer's disease in a large kindred with an E280A presenilin-1 mutation. In: JAMA. Volume 277, Number 10, March 1997, pp. 793-799, PMID 9052708 .
- ↑ Pam Belluck: Alzheimer's Stalks a Colombian Family. In: nytimes.com. June 1, 2010, accessed July 27, 2015 .
- ↑ PSEN1 E280A (Paisa). In: alzforum.org. Retrieved July 27, 2015 .
- ^ Andreas Kleinschmidt: Alzheimer early detection. In: siemens.com. April 15, 2013, accessed July 27, 2015 .
- ↑ F. Panza et al .: Amyloid-based immunotherapy for Alzheimer's disease in the time of prevention trials: the way forward. In: Expert review of clinical immunology. Volume 10, number 3, March 2014, pp. 405-419, doi: 10.1586 / 1744666X.2014.883921 , PMID 24490853 (review).
- ^ F. Panza et al .: Is there still any hope for amyloid-based immunotherapy for Alzheimer's disease? In: Current opinion in psychiatry. Volume 27, Number 2, March 2014, pp. 128-137, doi: 10.1097 / YCO.0000000000000041 , PMID 24445401 (review).
- ↑ Clinical Study (Phase II): A Study of Crenezumab Versus Placebo in Preclinical PSEN1 E280A Mutation Carriers to Evaluate Efficacy and Safety in the Treatment of Autosomal-Dominant Alzheimer Disease, Including a Placebo-Treated Noncarrier Cohort. at Clinicaltrials.gov the NIH
- ↑ Roche stops studies on Alzheimer's drug. In: tagesanzeiger.ch . January 30, 2019, accessed January 30, 2019 .
- ↑ SJ Soscia et al .: The Alzheimer's disease-associated amyloid beta-protein is an antimicrobial peptide. In: PloS one. Volume 5, number 3, 2010, p. E9505, doi: 10.1371 / journal.pone.0009505 . PMID 20209079 . PMC 2831066 (free full text).
- ↑ Stephen S. Dominy et al .: Porphyromonas gingivalis in Alzheimer's disease brains: Evidence for disease causation and treatment with small-molecule inhibitors In: Science Advances. Volume 5, Number 1, 2019,
- ↑ Clinical study (phase I): Study of COR388 HCl in Healthy Subjects at Clinicaltrials.gov of the NIH
- ↑ Clinical Study (Phase I): A Multiple Ascending Dose Study of COR388 at Clinicaltrials.gov of the NIH
- ↑ Michiyo Iba, Jing L. Guo, Jennifer D. McBride, Bin Zhang, John Q. Trojanowski and Virginia M.-Y. Lee: Synthetic Tau Fibrils Mediate Transmission of Neurofibrillary Tangles in a Transgenic Mouse Model of Alzheimer's-Like Tauopathy In: The Journal of Neuroscience . No. 33, January 16, 2013, pp. 1024-1037.
- ^ R. Mayeux, R. Ottman, M. Tang, L. Noboa-Bauza, K. Marder, B. Gurland, Y. Stern: Genetic susceptibility and head injury as risk factors for Alzheimer's disease among community-dwelling elderly persons and their first-degree relatives . In: Ann Neurol . . 33, No. 5, 1993, pp. 494-501. PMID 8498827 .
- ^
- ↑ JS Roriz-Filho, TM Sá-Roriz, I. Rosset, AL Camozzato, AC Santos, ML Chaves, JC Moriguti, M. Roriz-Cruz: (Pre) diabetes, brain aging, and cognition . In: Biochim Biophys Acta . 2009, pp. 432-443. PMID 19135149 .
- ↑ WQ Qiu, MF Folstein: insulin, insulin-degrading enzymes and amyloid-beta peptides in Alzheimer's disease: review and hypothesis . In: Neurobiol Aging . No. Feb; 27 (2), 2006, pp. 190-198. PMID 19135149 .
- ^ OS Kofman, VH Macmillan: Diffuse cerebral atrophy. In: Applied therapeutics. Volume 12, Number 4, April 1970, pp. 24-26, PMID 5446326 .
- ↑ M Crisby, L. Carlson, B. Winblad: Statins in the prevention and treatment of Alzheimer's disease . In: Alzheimer Disease & Associated Disorders . 16, No. 3, 2002, pp. 131-136. PMID 12218642 .
- ↑ P. Kehoe, G. Wilcock: Is inhibition of the renin-angiotensin system a new treatment option for Alzheimer's disease? . In: Lancet neurology . 6, No. 4, 2007, pp. 373-378. PMID 17362841 .
- ^ "Why stroke ups Alzheimer's risk" BBC, June 4, 2007
- ^ Nigel Hawkes: Alzheimers linked to aluminum pollution in tap water. In: The Times. April 20, 2006, accessed April 7, 2010 .
- ↑ Virginie Rondeau, Daniel Commenges, Hélène Jacqmin-Gadda, Jean-François Dartigues: Relation between Aluminum Concentrations in Drinking Water and Alzheimer's Disease: An 8-year Follow-up Study. . In: Am J Epidemiology . 2000. PMID 10901330 .
- ↑ V. Rondeau, H. Jacqmin-Gadda, D. Commenges, C. Helmer, J.-F. Dartigues: Aluminum and Silica in Drinking Water and the Risk of Alzheimer's Disease or Cognitive Decline: Findings From 15-Year Follow-up of the PAQUID Cohort . In: American Journal of Epidemiology . 169, No. 4, 2008, pp. 489-496. doi : 10.1093 / aje / kwn348 . PMID 19064650 . PMC 2809081 (free full text).
- ↑ Sakae Yumoto, Shigeo Kakimi, Akihiro Ohsaki, Akira Ishikawa: Demonstration of aluminum in amyloid fibers in the cores of senile plaques in the brains of patients with Alzheimer's disease . In: Journal of Inorganic Biochemistry . 103, No. 11, 2009, pp. 1579-84. doi : 10.1016 / j.jinorgbio.2009.07.023 . PMID 19744735 .
- ^ PC Ferreira, A. Piai Kde, AM Takayanagui, SI Segura-Muñoz: Aluminum as a risk factor for Alzheimer's disease . In: Rev Lat Am Enfermagem . 16, No. 1, 2008, pp. 151-157. doi : 10.1590 / S0104-11692008000100023 . PMID 18392545 .
- ^ Alzheimer's Society: Aluminum and Alzheimer's disease. (PDF) In: The Learning Exchange. June 2002, accessed August 9, 2019 .
- ↑ Federal Institute for Risk Assessment : No Alzheimer's Risk from Aluminum from Consumer Goods (PDF; 8 pages, 65 kB), on October 4, 2013.
- ↑ Federal Institute for Risk Assessment : Antiperspirants containing aluminum contribute to the absorption of aluminum. (PDF; 15 pages), March 10, 2014
- ↑ Lilian Calderón-Garcidueñas et al .: Hallmarks of Alzheimer's disease are evolving relentlessly in Metropolitan Mexico City infants, children and young adults. APOE4 carriers have higher suicide risk and higher odds of reaching NFT stage V at ≤ 40 years of age. In: Environmental Research , 164, 2018, p. 475, doi: 10.1016 / j.envres.2018.03.023 .
- ↑ Brain performance check for early detection of dementia . IGeL monitor; Retrieved January 15, 2019. Main sources therein: Meta-Analysis Tsoi 2016 . - KK Tsoi, HW Hirai, JY Chan, TC. Kwok: Time to Treatment Initiation in People With Alzheimer Disease: A Meta-Analysis of Randomized Controlled Trials . In: Journal of the American Medical Directors Association , 2016, 17, pp. 24-30, PMID 26392193 ; and systematic review Lin et al. 2013 - JS Lin, E. O'Connor, RC Rossom, LA Perdue, E. Eckstrom: Screening for cognitive impairment in older adults: A systematic review for the US Preventive Services Task Force . In: Annals of internal medicine , 2013, 159, pp. 601-612, PMID 24354019 . More on the justification for the assessment in Evidence compact . (PDF) accessed on January 15, 2019.
- ↑ MRI for early detection of Alzheimer's dementia . IGeL monitor; Retrieved January 15, 2019. Main sources therein: NICE guideline from 2011 . (National Institute for Health and Clinical Excellence of the British health authority NHS) and meta-analysis Schmand et al. 2010 . - B. Schmand, HM Huizenga, WA van Gool: Meta-analysis of CSF and MRI biomarkers for detecting preclinical Alzheimer's disease . In: Psychological Medicine , January 2010, 40 (1): pp. 135-145, PMID 19863841 . More on the justification for the assessment in the evidence synthesis . (PDF) accessed on January 15, 2019.
- ↑ Article from the Tagesspiegel . from February 21, 2018 or from the Ärzte-Zeitung . dated December 5, 2017.
- ^ National Institute on Aging: The Seven Warning Signs of Alzheimer's Disease. ( Memento of March 12, 2009 in the Internet Archive )
- ^ RT Linn et al .: The 'preclinical phase' of probable Alzheimer's disease. A 13-year prospective study of the Framingham cohort . In: Arch Neurol . . 52, No. 5, 1995, pp. 485-490. PMID 7733843 .
- ^ J. Saxton et al .: Preclinical Alzheimer disease: neuropsychological test performance 1.5 to 8 years prior to onset . In: Neurology . 63, No. 12, 2004, pp. 2341-2347. PMID 15623697 .
- ↑ EW Twamley, SA Ropacki, MW Bondi: Neuropsychological and neuroimaging changes in preclinical Alzheimer's disease . In: J Int Neuropsychol Soc . 12, No. 5, 2006, pp. 707-735. doi : 10.1017 / S1355617706060863 . PMID 16961952 .
- ^ CR Jack et al .: Introduction to the recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. In: Alzheimer's & dementia: the journal of the Alzheimer's Association. Volume 7, number 3, May 2011, pp. 257-262, doi: 10.1016 / j.jalz.2011.03.004 . PMID 21514247 . PMC 3096735 (free full text).
- ^ GB Frisoni et al .: Revised criteria for Alzheimer's disease: what are the lessons for clinicians? In: The Lancet. Neurology. Volume 10, Number 7, July 2011, pp. 598-601, doi: 10.1016 / S1474-4422 (11) 70126-0 . PMID 21683925 .
- ^ RA Sperling et al .: Toward defining the preclinical stages of Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. In: Alzheimer's & dementia. Volume 7, number 3, May 2011, pp. 280-292, doi: 10.1016 / j.jalz.2011.03.003 . PMID 21514248 . PMC 3220946 (free full text).
- ↑ a b M. S. Albert et al .: The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. In: Alzheimer's & dementia: the journal of the Alzheimer's Association. Volume 7, number 3, May 2011, pp. 270-279, doi: 10.1016 / j.jalz.2011.03.008 . PMID 21514249 . PMC 3312027 (free full text).
- ↑ GM McKhann et al .: The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. In: Alzheimer's & dementia: the journal of the Alzheimer's Association. Volume 7, number 3, May 2011, pp. 263-269, doi: 10.1016 / j.jalz.2011.03.005 . PMID 21514250 . PMC 3312024 (free full text).
- ↑ H.-J. Gertz, A. Kurz: Diagnosis without therapy. Early diagnosis of Alzheimer's disease in the stage of mild cognitive impairment. In: The neurologist. Volume 82, Number 9, 2011, doi: 10.1007 / s00115-010-3213-3
- ↑ H. Barthel et al .: Cerebral amyloid-β PET with florbetaben (18F) in patients with Alzheimer's disease and healthy controls: a multicentre phase 2 diagnostic study. In: The Lancet. Neurology. Volume 10, Number 5, May 2011, pp. 424-435, doi: 10.1016 / S1474-4422 (11) 70077-1 . PMID 21481640 .
- ↑ Benefit assessment of drugs with new active ingredients according to § 35a SGB V - Florbetaben , decision of the G-BA "new examination method" of February 20, 2014, accessed on March 6, 2014
- ↑ Thomas Hauser et al ..: Mild cognitive impairment. Diagnostic value of various MRT techniques. In: The Radiologist. 2011; 51: pp. 285-292 doi: 10.1007 / s00117-010-2094-6
- ↑ Marcus Bauser, Lutz Lehmann: positron emission tomography . In: Chemistry in Our Time . tape 46 , no. 2 , 2012, p. 94 , doi : 10.1002 / ciuz.201200564 .
- ↑ G. Querques et al .: Functional and morphological changes of the retinal vessels in Alzheimer's disease and mild cognitive impairment. Nature Scientic Reports 2019; 9:63
- ^ L. Mucke: Neuroscience: Alzheimer's disease . In: Nature . 461, 2009, pp. 895-897. PMID 19829367 .
- ↑ a b H. Förstl, A. Short: Clinical features of Alzheimer's disease . In: European Archives of Psychiatry and Clinical Neuroscience . tape 249 , no. 6 , 1999, p. 288-290 , PMID 10653284 .
- ^ GA Carlesimo, M. Oscar-Berman: Memory deficits in Alzheimer's patients: a comprehensive review . In: Neuropsychology Review . tape 3 , no. 2 , 1992, p. 119-169 , PMID 1300219 .
- ↑ M. Jelicic, AE Bonebakker, B. Bonke: Implicit memory performance of patients with Alzheimer's disease: a brief review . In: International psychogeriatrics / IPA . tape 7 , no. 3 , 1995, p. 385-392 , PMID 8821346 .
- ^ EM Frank: Effect of Alzheimer's Disease on Communication Function . In: Journal of the South Carolina Medical Association (1975) . tape 90 , no. 9 , 1994, pp. 417-423 , PMID 7967534 .
- ↑ JT Becker, AA Overman: [The semantic memory deficit in Alzheimer's disease] . In: Revista De Neurologia . tape 35 , no. 8 , 2002, p. 777-783 , PMID 12402233 .
- ↑ JR Hodges, K. Patterson: Is semantic memory consistently impaired early in the course of Alzheimer's disease? Neuroanatomical and diagnostic implications . In: Neuropsychologia . tape 33 , no. 4 , 1995, p. 441-459 , PMID 7617154 .
- ↑ T. Benke: Two forms of apraxia in Alzheimer's disease . In: cortex; a Journal Devoted to the Study of the Nervous System and Behavior . tape 29 , no. 4 , 1993, p. 715-725 , PMID 8124945 .
- ↑ Liz Kumru: Getting Lost in Alzheimer's . UNMC; accessed on July 22, 2007 unmc.edu ( Memento from May 10, 2001 in the Internet Archive )
- ↑ Tom Rickey: Road Skills Hint At "Motion Blindness" Of Alzheimer's. University of Rochester Medical Center, January 31, 2002, accessed March 25, 2016 .
- ↑ Concepts for Alzheimer's vaccinations in the test laboratory. In: Deutsches Ärzteblatt. November 9, 2017, accessed August 9, 2019 .
- ↑ Antibody dissolves amyloid in Alzheimer's patients. Doctors newspaper , May 21, 2010, accessed November 6, 2010 .
- ↑ rme / aerzteblatt.de: Alzheimer's: Second study on antibody therapy canceled. In: aerzteblatt.de . August 7, 2012, accessed December 27, 2014 .
- ↑ Oliver Wirths et al .: Identification of low molecular weight pyroglutamate A {beta} oligomers in Alzheimer's disease: a novel tool for therapy and diagnosis . In: The Journal of Biological Chemistry . tape 285 , no. 53 , 2010, p. 41517-41524 , doi : 10.1074 / jbc.M110.178707 , PMID 20971852 , PMC 3009878 (free full text). .
- ↑ Stefan Weller: Therapy against Alzheimer's: Göttingen researchers develop a new approach for passive immunization. Universitätsmedizin Göttingen - Georg-August-Universität, press release from November 5, 2010 at the Informationsdienst Wissenschaft (idw-online.de), accessed on November 6, 2010.
- ^ Gary W. Small: What we need to know about age related memory loss. In: British Medical Journal . June 22, 2002, accessed November 5, 2006 .
- ↑ MZ Scalco, R. van Reekum: Prevention of Alzheimer's disease. Encouraging evidence. In: Canadian family physician Médecin de famille canadien. Volume 52, February 2006, pp. 200-207, PMID 16529393 . PMC 1479722 (free full text). (Review).
- ↑ Sam Norton et al .: Potential for primary prevention of Alzheimer's disease: an analysis of population-based data . In: The Lancet Neurology . 13, No. 8, 2014, pp. 788-794. doi : 10.1016 / S1474-4422 (14) 70136-X .
- ↑ KA Ginis et al .: Formulation of evidence-based messages to promote the use of physical activity to prevent and manage Alzheimer's disease . In: BMC Public Health . tape 17 , no. 1 , February 2017, p. 209 , doi : 10.1186 / s12889-017-4090-5 , PMID 28212648 , PMC 5316179 (free full text).
- ↑ Apples for the brain. On: Wissenschaft.de from November 19, 2004.
- ↑ With fish oil against oblivion. On: Wissenschaft.de from September 2, 2004.
- ↑ M. Morris, J. Schneider, C. Tangney: Thoughts on B vitamins and dementia . In: J Alzheimers Dis . 9, No. 4, 2006, pp. 429-433. PMID 16917152 .
- ↑ Inna I. Kruman et al .: Folic Acid Deficiency and Homocysteine Impair DNA Repair in Hippocampal Neurons and Sensitize Them to Amyloid Toxicity in Experimental Models of Alzheimer's Disease . In: The Journal of Neuroscience . 22, No. 5, March 1, 2002. PMID 11880504 . A simplified report can be found here: www.alzheimers.org.uk
- ^ Folate May Lower Alzheimer's Risk In: CBS news , reporting from WebMD.
- ↑ NIH Press Release: Folic Acid Possibly A Key Factor In Alzheimer's Disease Prevention. (No longer available online.) In: nih.gov. January 3, 2002, archived from the original on June 24, 2014 ; accessed on December 29, 2019 .
- ↑ Kathleen Fackelmann: USATODAY.com - Folate shows promise in preventing Alzheimer's. In: usatoday.com. August 14, 2005, accessed December 27, 2014 .
- ^ Smoking excuse refuted. On: Wissenschaft.de from February 8, 2005.
- ↑ DE Zylberstein et al .: Midlife homocysteine and late-life dementia in women. A prospective population study. In: Neurobiology of aging. Volume 32, number 3, March 2011, pp. 380-386, doi: 10.1016 / j.neurobiolaging.2009.02.024 . PMID 19342123 .
- ^ AD Smith et al .: Homocysteine-lowering by B vitamins slows the rate of accelerated brain atrophy in mild cognitive impairment: a randomized controlled trial. In: PloS one. Volume 5, number 9, 2010, p. E12244, doi: 10.1371 / journal.pone.0012244 . PMID 20838622 . PMC 2935890 (free full text).
- ↑ G. Douaud et al .: Preventing Alzheimer's disease-related gray matter atrophy by B-vitamin treatment. In: Proceedings of the National Academy of Sciences . Volume 110, number 23, June 2013, pp. 9523-9528, doi: 10.1073 / pnas.1301816110 . PMID 23690582 . PMC 3677457 (free full text).
- ↑ The miracle weapon against Alzheimer's. In: vitamin-b12-mangel.org. July 2013, accessed December 27, 2014 .
- ↑ Andrea Gerlin: Vitamins That Cost Pennies a Day Seen Delaying Dementia - Businessweek. In: businessweek.com. May 20, 2013, accessed December 27, 2014 .
- ^ Education May Not Protect Against Dementia as Previously Thought. Rush University, February 6, 2019, accessed August 9, 2019 .
- ^ Roy Eccleston: Think or sink. (PDF) (No longer available online.) In: The Weekend Australian Magazine. December 2, 2006, archived from the original on July 23, 2008 ; Retrieved January 3, 2009 .
- ↑ Solving crossword puzzles is not enough. (No longer available online.) In: GesundheitPro.de. November 8, 2007, archived from the original on July 10, 2009 ; Retrieved January 3, 2009 .
- ↑ Blood pressure lowering agents can prevent dementia. On: Wissenschaft.de from October 14, 2002.
- ^ A. Brüning: How cholesterol increases the risk of Alzheimer's. In: Berliner Zeitung of October 11, 2005.
- ↑ Berliner Zeitung of October 24, 2013, p. 12.
- ^ JP Guo, S. Yu, PL. McGeer: Simple in vitro assays to identify amyloid-beta aggregation blockers for Alzheimer's disease therapy . In: J Alzheimers Dis . 19, No. 4, 2010, pp. 1359-1370. PMID 20061605 .
- ↑ S, Abbas, M. Mink: Epigallocatechin gallate inhibits beta amyloid oligomerization in Caenorhabditis elegans and affects the daf-2 / insulin-like signaling pathway . In: J Alzheimers Dis . 17, No. 11, 2010, pp. 902-909. PMID 20382008 .
- ↑ DE Ehrnhoefer et al .: EGCG redirects amyloidogenic polypeptides into unstructured, off-pathway oligomers . In: Nat Struct Mol Biol . . 15, No. 5, June 2008, pp. 558-566. PMID 18511942 .
- ↑ J. Bieschke et al .: EGCG remodels mature α-synuclein and amyloid-β fibrils and reduces cellular toxicity . In: Proc Natl Acad Sci USA . 107, No. 17, April 2010. PMID 20385841 .
- ↑ F. Meng et al .: The flavanol (-) - epigallocatechin 3-gallate inhibits amyloid formation by islet amyloid polypeptide, disaggregates amyloid fibrils, and protects cultured cells against IAPP-induced toxicity . In: Biochemistry . 49, No. 37, September 2010. PMID 20707388 .
- ↑ K. Rezai-Zadeh et al .: Green tea epigallocatechin-3-gallate (EGCG) reduces beta-amyloid mediated cognitive impairment and modulates tau pathology in Alzheimer transgenic mice . In: Brain Res. . 12, No. 1214, June 2008, pp. 177-186. PMID 18457818 .
- ↑ "How does EGCG intervene in the mechanism of amyoid formation?"
- ↑ G. Grelle et al .: Black Tea Theaflavins Inhibit Formation of Toxic Amyloid-β and α-Synuclein Fibrils . In: Biochemistry . November 2011. PMID 22054421 .
- ^ PE Cramer et al .: ApoE-directed therapeutics rapidly clear β-amyloid and reverse deficits in AD mouse models. In: Science. Volume 335, number 6075, March 2012, pp. 1503–1506, doi: 10.1126 / science.1217697 . PMID 22323736 . PMC 3651582 (free full text).
- ↑ Jessica Studeny: Drug quickly reverses Alzheimer's symptoms in mice . Case Western Reserve University publication , February 9, 2012.
- ↑ Drug Quickly Reverses Alzheimer's Symptoms in Mice . Reported to Neurosciencenews.com on February 10, 2012.
- ↑ Harald Frater: Cancer drug reverses Alzheimer's symptoms: active ingredient bexarotene removes memory disorders and protein plaques in mice. In: go.de. February 10, 2012, accessed December 27, 2014 .
- ^ E. O'Hare et al .: Lack of support for bexarotene as a treatment for Alzheimer's disease. In: Neuropharmacology. [Electronic publication before printing] May 2015, doi: 10.1016 / j.neuropharm.2015.04.020 , PMID 26025659 .
- ↑ C. Balducci et al .: The Continuing Failure of Bexarotene in Alzheimer's Disease Mice. In: Journal of Alzheimer's disease: JAD. [Electronic publication before printing] March 2015, doi: 10.3233 / JAD-150029 , PMID 25777514 .
- ↑ B. Tousi: The emerging role of bexarotene in the treatment of Alzheimer's disease: evidence current. In: Neuropsychiatric disease and treatment. Volume 11, 2015, pp. 311-315, doi: 10.2147 / NDT.S61309 , PMID 25709453 , PMC 4327563 (free full text) (review).
- ↑ Web link for paper Paul T. Francis, Gordon K. Wilcock et al .: The cholinergic hypothesis of Alzheimer's disease: a review of progress In: J Neurol Neurosurg Psychiatry (1999)
- ^ Huperzine A Alzheimer Research Forum
- ↑ BS Wang, H. Wang, ZH Wei, YY Song, L. Zhang, HZ Chen: Efficacy and safety of natural acetylcholinesterase inhibitor huperzine A in the treatment of Alzheimer's disease: an updated meta-analysis . In: Journal of Neural Transmission . 116, No. 4, 2009, pp. 457-465. doi : 10.1007 / s00702-009-0189-x . PMID 19221692 .
- ↑ B. Winblad, J. Cummings, N. Andreasen et al .: A six-month double-blind, randomized, placebo-controlled study of a transdermal patch in Alzheimer's disease - rivastigmine patch versus capsule. In: International Journal of Geriatric Psychiatry Vol. 22, No. 5, pp. 456-467, May 2007 doi: 10.1002 / gps.1788 PMID 17380489
- ↑ H. Kaduszkiewicz, T. Zimmermann, HP Beck-Bornholdt, Hendrik van den Bussche : Cholinesterase inhibitors for patients with Alzheimer's disease: systematic review of randomized clinical trials . In: BMJ (Clinical Research Ed.) . 331, No. 7512, August 2005, pp. 321-327. PMID 16081444 . PMC 1183129 (free full text).
- ↑ T. Lempert, T. Bschor: [Treatment of Alzheimer's disease according to the S3 guidelines on dementia. Choline esterase inhibitors for all and for ever?]. In: The neurologist. Volume 82, Number 1, January 2011, pp. 90-91, doi: 10.1007 / s00115-010-3233-z . PMID 21274696 .
- ↑ JC Breitner, KA Welsh et al .: Delayed onset of Alzheimer's disease with nonsteroidal anti-inflammatory and histamine H2 blocking drugs. In: Neurobiology of Aging Volume 16, Issue 4, Pages 523-530, July 1995 PMID 8544901
- ↑ T. Wyss-Coray, L. Mucke: Ibuprofen, inflammation and Alzheimer's disease. In: Nature medicine. Volume 6, Number 9, September 2000, pp. 973-974, doi: 10.1038 / 79661 . PMID 10973311 .
- ↑ D. Dokmeci: Ibuprofen and Alzheimer's disease. In: Folia medica. Volume 46, Number 2, 2004, pp. 5-10, PMID 15506544 . (Review).
- ↑ T. Morihara et al .: Ibuprofen suppresses interleukin-1beta induction of pro-amyloidogenic alpha1-antichymotrypsin to ameliorate beta-amyloid (Abeta) pathology in Alzheimer's models. In: Neuropsychopharmacology: official publication of the American College of Neuropsychopharmacology. Volume 30, Number 6, June 2005, pp. 1111-1120, doi: 10.1038 / sj.npp.1300668 . PMID 15688088 .
- ^ AC McKee et al .: Ibuprofen reduces Abeta, hyperphosphorylated tau and memory deficits in Alzheimer mice. In: Brain research. Volume 1207, May 2008, pp. 225-236, doi: 10.1016 / j.brainres.2008.01.095 . PMID 18374906 . PMC 2587244 (free full text).
- ↑ M. Sastre et al .: Nonsteroidal anti-inflammatory drugs repress beta-secretase gene promoter activity by the activation of PPARgamma. In: Proceedings of the National Academy of Sciences . Volume 103, Number 2, January 2006, pp. 443-448, doi: 10.1073 / pnas.0503839103 . PMID 16407166 . PMC 1326151 (free full text).
- ↑ N. Tabet, H. Feldmand: Ibuprofen for Alzheimer's disease. In: The Cochrane database of systematic reviews. Number 2, 2003, S. CD004031, doi: 10.1002 / 14651858.CD004031 . PMID 12804498 . (Review).
- ↑ B. De Strooper, G. König: An inflammatory drug prospect. In: Nature. Volume 414, Number 6860, November 2001, pp. 159-160, doi: 10.1038 / 35102656 . PMID 11700538 .
- ↑ Gregor Larbig: Studies to identify & optimize potential active ingredients for the treatment of Alzheimer's disease. Dissertation, TU Darmstadt, 2007
- ↑ T. Müller: New ways against the amyloid in the brain. In: Doctors newspaper on December 7, 2007
- ↑ M. Krohn et al .: Cerebral amyloid-β proteostasis is regulated by the membrane transport protein ABCC1 in mice. In: The Journal of clinical investigation. Volume 121, number 10, October 2011, pp. 3924-3931, doi: 10.1172 / JCI57867 . PMID 21881209 . PMC 3195473 (free full text).
- ^ R. McShane, A. Areosa Sastre, N. Minakaran: Memantine for dementia. In: The Cochrane database of systematic reviews. Number 2, 2006, p. CD003154, doi: 10.1002 / 14651858.CD003154.pub5 . PMID 16625572 . (Review).
- ^ J. Birks, Evans J. Grimley: Ginkgo biloba for cognitive impairment and dementia . In: Cochrane Database Syst Rev . No. 2, 2007, p. CD003120. doi : 10.1002 / 14651858.CD003120.pub2 . PMID 17443523 .
- ↑ J. Birks, E. Grimley, M. Van Dongen: Ginkgo biloba for cognitive impairment and dementia. . In: Cochrane Database Syst Rev . August, p. CD003120. PMID 12519586 .
- ↑ ST DeKosky, A. Fitzpatrick, DG Ives, J. Saxton, J. Williamson, OL Lopez, G. Burke, L. Fried, LH Kuller, J. Robbins, R. Tracy, N. Woolard, L. Dunn, R Kronmal, R. Nahin, C. Furberg: The Ginkgo Evaluation of Memory (GEM) study: design and baseline data of a randomized trial of Ginkgo biloba extract in prevention of dementia . In: Contemp Clin Trials . 27, No. 3, 2006, pp. 238-253. doi : 10.1016 / j.cct.2006.02.007 . PMID 16627007 .
- ↑ Ginkgo Biloba Does Not Reduce Dementia Risk, Study Shows. In: sciencedaily.com. November 19, 2008, accessed December 27, 2014 .
- ↑ BE Snitz et al .: Ginkgo biloba for preventing cognitive decline in older adults: a randomized trial. In: JAMA. Volume 302, Number 24, December 2009, pp. 2663-2670, doi: 10.1001 / jama.2009.1913 . PMID 20040554 . PMC 2832285 (free full text).
- ↑ Stefan Weinmann et al .: Effects of Ginkgo biloba in dementia: systematic review and meta-analysis. In: BMC Geriatrics 2010, 10:14 doi: 10.1186 / 1471-2318-10-14
- ^ Institute for Quality and Efficiency in Health Care: Final report "Ginkgo-containing preparations in Alzheimer's dementia". Published on November 21, 2008 (PDF file) (PDF)
- ^ B. Kastenholz: Phytopharmaceuticals in the therapy of younger Alzheimer patients . WebmedCentral AGING 2011; 2 (7): WMC002011.
- ^ S. Krishnan, R. Cairns, R. Howard: Cannabinoids for the treatment of dementia. In: The Cochrane database of systematic reviews. Number 2, 2009, S. CD007204, doi: 10.1002 / 14651858.CD007204.pub2 , PMID 19370677 (Review).
- ↑ S. Craft et al .: Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment: a pilot clinical trial. In: Archives of neurology. Volume 69, number 1, January 2012, pp. 29-38, doi: 10.1001 / archneurol.2011.233 . PMID 21911655 . PMC 3260944 (free full text).
- ↑ MW Dysken et al .: Effect of vitamin E and memantine on functional decline in Alzheimer's disease: the TEAM AD VA cooperative randomized trial. In: JAMA. Volume 311, number 1, January 2014, pp. 33-44, doi: 10.1001 / jama.2013.282834 . PMID 24381967 . PMC 4109898 (free full text).
- ↑ M. Sano et al .: A controlled trial of selegiline, alpha-tocopherol, or both as treatment for Alzheimer's disease. The Alzheimer's Disease Cooperative Study. In: The New England Journal of Medicine . Volume 336, Number 17, April 1997, pp. 1216-1222, doi: 10.1056 / NEJM199704243361704 . PMID 9110909 .
- ↑ R. C. Petersen et al .: Vitamin E and donepezil for the treatment of mild cognitive impairment. In: The New England Journal of Medicine . Volume 352, Number 23, June 2005, pp. 2379-2388, doi: 10.1056 / NEJMoa050151 . PMID 15829527 .
- ^ JH Kang et al .: A randomized trial of vitamin E supplementation and cognitive function in women. In: Archives of internal medicine. Volume 166, Number 22, 2006 Dec 11-25, pp. 2462-2468, doi: 10.1001 / archinte.166.22.2462 . PMID 17159011 .
- ↑ JH Kang et al .: Vitamin E, vitamin C, beta carotene, and cognitive function among women with or at risk of cardiovascular disease: The Women's Antioxidant and Cardiovascular Study. In: Circulation. Volume 119, Number 21, June 2009, pp. 2772-2780, doi: 10.1161 / CIRCULATIONAHA.108.816900 . PMID 19451353 . PMC 2752297 (free full text).
- ↑ ER Miller et al .: Meta-analysis: high-dosage vitamin E supplementation may increase all-cause mortality. In: Annals of internal medicine. Volume 142, Number 1, January 2005, pp. 37-46, PMID 15537682 .
- ↑ Hilkka Soininen et al .: 24-month intervention with a specific multinutrient in people with prodromal Alzheimer's disease (LipiDiDiet): a randomized, double-blind, controlled trial . In: The Lancet Neurology . tape 0 , no. 0 , ISSN 1474-4422 , doi : 10.1016 / S1474-4422 (17) 30332-0 ( thelancet.com [accessed November 11, 2017]).
- ↑ Doctors newspaper: European study: Does nutrient combination help with Alzheimer's in the early stages? Retrieved November 11, 2017 .
- ^ J. Cohen-Mansfield: Nonpharmacologic interventions for inappropriate behaviors in dementia: a review, summary, and critique. In: Am J Geriatr Psychiatry. 9 (4), 2001, pp. 361-381. PMID 11739063 (Review)
- ↑ ( BBC News August 2004 )
- ^ LE Middleton et al .: Activity energy expenditure and incident cognitive impairment in older adults. In: Archives of internal medicine. Volume 171, number 14, July 2011, pp. 1251–1257, doi: 10.1001 / archinternmed.2011.277 . PMID 21771893 . PMC 3923462 (free full text).
- ↑ MN Vercambre et al .: Physical activity and cognition in women with vascular conditions. In: Archives of internal medicine. Volume 171, number 14, July 2011, pp. 1244-1250, doi: 10.1001 / archinternmed.2011.282 . PMID 21771894 . PMC 3153432 (free full text).
- ↑ TE Dunne, SA Neargarder, PB Cipolloni, A. Cronin-Golomb: Visual contrast Enhances food and liquid intake in advanced Alzheimer's disease . In: Clin Nutr . 23, No. 4, 2004, pp. 533-538. PMID 15297089 .
- ^ S3 guideline dementias . 2017, doi : 10.1007 / 978-3-662-53875-3 .
- ↑ A. Alzheimer's: About a strange disease of the cerebral cortex . In: Allg. Z. psychiatrist. Psych. Court Med. . 64, No. 1-2, 1907, pp. 146-148.
- ↑ Konrad Maurer, Ulrike Maurer: Alzheimer: the life of a physician and the career of a disease . Columbia University Press, New York 2003, ISBN 0-231-11896-1 .
- ^ Fred H. Hochberg, David Rottenberg: Neurological classics in modern translation . Hafner Press, New York 1977, ISBN 0-02-851180-8 .
- ^ NC Berchtold, CW Cotman: Evolution in the conceptualization of dementia and Alzheimer's disease: Greco-Roman period to the 1960s . In: Neurobiol. Aging . 19, No. 3, 1998, pp. 173-189. PMID 9661992 .
- ^ Emil Kraepelin: Textbook of Psychiatry 1910.
- ^ MB Graeber et al .: Rediscovery of the case described by Alois Alzheimer in 1911: historical, histological and molecular genetic analysis. In: Neurogenetics. Volume 1, Number 1, May 1997, pp. 73-80, PMID 10735278 .
- ↑ U. Müller, P. Winter, MB Graeber: A presenilin 1 mutation in the first case of Alzheimer's disease. In: The Lancet. Neurology. Volume 12, Number 2, February 2013, pp. 129-130, doi: 10.1016 / S1474-4422 (12) 70307-1 . PMID 23246540 .
- ^ Award-winning biography Iris from 2001. It tells the story of her decline from the point of view of her husband, John Bayley. Murdoch was portrayed by Kate Winslet and Judi Dench .
- ↑ Jochen Wittmann: Pratchett's "Choosing to die: Suicide at prime time. In: derstandard.at . June 15, 2011, accessed on December 27, 2014 .
- ↑ Tilman Jens: Father's Forgetting. In: FAZ.net . March 4, 2008, accessed December 27, 2014 .
- ↑ Paul Wolff: Von der Leyen and her father's illness. In: welt.de . May 27, 2008, accessed December 27, 2014 .
- ↑ For example, the cover story in "Die Zeit" from May 12, 2011: The fear of Alzheimer's
- ^ Gabriel García Márquez: Nobel laureate in literature suffers from dementia. In: Spiegel Online . July 8, 2012, accessed December 27, 2014 .
- ^ Bitter irony of Alzheimer's for Nobel laureate Marquez as his symptoms mimic masterpiece
- ↑ Gerd Müller turns 70. In: fcbayern.de. October 6, 2015, accessed October 6, 2015 .
- ^ DHPV honorary award to Arno Geiger on www.dhpv.de, October 10, 2011
- ↑ Step out of the shadows - Why I stand up for our rights as a person affected by dementia by Helga Rohra at www.demenz-support.de
- ↑ Ralph Trommer: Master of the quiet tones. In: taz.de . November 4, 2013, accessed December 27, 2014 .
- ↑ Theater maker Barbara Wachendorff with a play about dementia
- ↑ Interview with director Barbara Wachendorff. In: Sommerblut - Festival of Multipolar Culture. May 7, 2012, accessed August 9, 2019 .
- ↑ Anderland - dementia play
- ↑ One day ... Official homepage for the feature film
- ↑ DVD box dementia. In: LVR-Klinikverbund. Landschaftsverband Rheinland (LVR), accessed on August 9, 2019 .
- ↑ By Johan Dehoust: Maxim Gorki Theater: Stuhlkreis mit Kater. In: Spiegel Online . January 2, 2013, accessed December 27, 2014 .
- ↑ Thomas Liesen (script and direction), Ulrike Schweitzer (editor): Leben, Lieben, Vergessen… Längengrad-Filmproduktion, 2013 online on YouTube .
- ↑ Film drama "Still Alice", information and rating on score11.de , accessed on September 12, 2015.
- ↑ We have to win the battle against Alzheimer's
- ↑ Alzheimer's disease burden on health systems and the economy (PDF) In: Medical Tribune , 36/2009