Senile plaques
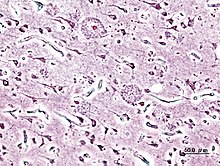
Senile plaques (syn. Neuritic plaques, senile drusen, cerebral glands) are extracellular deposits of beta-amyloid in the gray matter of the brain. The deposits are associated with degenerative neural structures and increased occurrence of cells ( microglia , astrocytes ). In Alzheimer's disease they occur in great density.
proof
Usually the senile plaques are detected by light microscopy after silvering, staining with Congo red , thioflavine , cresyl violet , PAS reaction , by fluorescence and immunofluorescence microscopy.
Occurrence
Senile plaques are found in both human and animal brains (including mammals , birds ). Artificially, a strain of mice (transgenic) could be created by introducing human genes , which forms the precursor protein of the Aβ peptides and develops plaques. The occurrence in humans without symptoms of dementia can speak for clinically not yet manifest, compensated early stages of a pathological process. However, a small number of senile plaques also appear in the physiological process of aging. Beyond the age of 60 years (approx. 10%), the proportion of those affected increases almost linearly up to around the age of 80 (approx. 60%). Women are affected slightly more often than men. The plaques occur particularly often in the tonsil nucleus and in the convoluted valleys of the cerebral cortex .
history
Paul Oscar Blocq and Gheorghe Marinescu described plaques in the gray matter of the brain in 1892 . Because of their microscopic resemblance to Actinomyces drusen, the plaques were called drusige necroses by O. Fischer at the beginning of the 20th century . The appearance of plaques in connection with dementia was described by Alois Alzheimer in 1906. As early as 1911, Bielschowsky suspected amyloid deposits to be important for their formation. Relationships between Alzheimer's disease , the occurrence of senile plaques, fibril changes and angiopathic changes have been established since the beginning of the 20th century . Wisniewski named the deposits in 1973 "neuritic plaques". Also in the 1970s, hypotheses arose about immunological and genetic factors in plaque formation (Katenkamp, Op den Velde and Stam). Elaborate statistical studies from this period come from JAN Corsellis and M. Franke. Franke proved that a plaque density of over 200 / mm³ frontal cortex is likely to cause dementia. It also supports the hypothesis that hormonal factors play a role in plaque formation (women with tumors have reduced plaque formation). It was not until the end of the 20th century that the main components of plaques had been extensively researched (e.g. the Aβ peptides were identified biochemically in 1985), but there are still many questions about their formation and significance, and above all questions about how these processes can be influenced open.
Origin and description
The plaques vary in shape and size (50 µm on average). The senile plaques can be further differentiated according to their variable appearance and composition.
The amyloid of senile plaques is formed by the deposition of Aβ peptides (39 to mainly 42 amino acids ). These polypeptides tend to aggregate and are neurotoxic in appropriate concentrations . The formation of aggregates in brain tissue seems to be the result of years of interplay between deposition and degradation processes. It is unclear why the deposition takes place in the brain and not in other organs despite the presence of the peptides in the entire organism. In laser scanning microscopy, the three-dimensional structure of plaques is described with a porous core and a shell that decreases in density towards the periphery. In certain cases, especially in younger patients (e.g. in trisomy 21 / Down syndrome ), the formation has a genetic background (e.g. faulty coding of the amyloid precursor protein APP due to point mutation on chromosome 21 , faulty coding of the Secretases presenilin 1 and 2 on chromosome 14 and chromosome 1 ). The epsilon-4 allele of apolipoprotein E is considered a genetic risk factor . If there are disruptions in the degradation of the APP, the Aβ peptides are deposited in vessels or in the form of plaques. However, other factors play a role in plaque formation, e.g. Sometimes unknown factors, probably also hormonal, immunological, inflammatory processes, diseases of the fat and sugar metabolism play a role.
In a new study it was shown that beta-amyloid is deposited in the brain even after a severe head trauma . Interestingly, it is not the lesion that is primarily affected by the deposits , but rather other areas of the brain, especially the striatum . There are also frequent changes in Alzheimer's disease . However, a connection between severe head trauma and later dementia has not yet been proven.
meaning
In addition to pathological neurofibrils, neuropil threads and vacuolar degeneration, cerebral atrophic changes with hydrocephalus e vacuo, the senile plaques are important criteria for the neuropathological-histological post-mortem detection of Alzheimer's disease. The emergence and distribution pattern of neurofibrils and neuropil threads follows a certain regularity (Braak and Braak) and enables a division into stages. Together with the appearance of many senile plaques, the diagnosis of Alzheimer's disease is very likely. Theoretically, this would lay the foundations for a brain biopsy examination, but the intervention is not justified if the therapeutic options and diagnostic alternatives such as positron emission tomography are still unsatisfactory .
literature
- Manfred Franke: Statistical studies on the senile drusen in the human brain (on the problem of cerebral gland disease). Diss. B 1975. Akad. Für Ärztl. Advanced training d. GDR, Berlin 1976. (German national biography, signature: DBF H 76/10016, IDN: 801313783 theses on the dissertation ( Memento from December 31, 2006 in the Internet Archive ))
- H. Braak, E. Braak, J. Bohl: Staging of Alzheimer-related cortical destruction. In: European Neurology. Basel, 33, 1993, pp. 403-408.
- KA Jellinger: Neurodegenerative Diseases (CNS) - A current overview. In: Journal of Neurology, Neurosurgery and Psychiatry. 6 (1), 2005, pp. 9-18.
- L. Cruz, B. Urbanc: Aggregation and disaggregation of senile plaques in Alzheimer's disease. In: Proc. Natl. Acad. Sci. UNITED STATES. Neurobiology. Vol. 94, July 1997, pp. 7612-7616.
Individual evidence
- ↑ Young T. Hong, Tonny Veenith, Deborah Dewar, Joanne G. Outtrim, Vaithianadan Mani, Claire Williams, Sally Pimlott, Peter JA Hutchinson, Adriana Tavares, Roberto Canales, Chester A. Mathis, William E. Klunk, Franklin I. Aigbirhio , Jonathan P. Coles, Jean-Claude Baron, John D. Pickard, Tim D. Fryer, William Stewart, David K. Menon: Amyloid Imaging With Carbon 11-Labeled Pittsburgh Compound B for Traumatic Brain Injury. In: JAMA Neurology. , S., doi : 10.1001 / jamaneurol.2013.4847 .