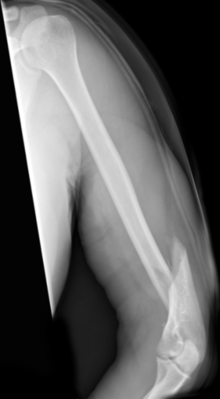
Humeral shaft fracture
| Classification according to ICD-10 | |
|---|---|
| S42.3 | Fracture of the humeral shaft |
| ICD-10 online (WHO version 2019) | |
The humeral shaft fracture , medical terminology ( jargon ) as a humeral shaft fracture , humeral shaft fracture or diaphyseal fracture of the humerus called, is a fracture of the humerus bone ( humerus ) in the region of the shaft ( diaphysis ), ie outside the area of the adjoining joints (elbow and shoulder joint). The anatomy of the upper arm , especially the close proximity to nerves ( radial nerve ) and blood vessels, causes the special problems of treating these fractures.
Origin and fracture forms
On the one hand, fractures of the upper arm can occur as a result of direct violence such as a hit with a hard object, a traffic accident (side impact of another vehicle) or a fall on a hard object; indirect violence such as falling on the bent arm, twisting against resistance or bending over a pivot point is more common ( Hypomochlion ). The course of the accident has a direct influence on the shape of the fracture: While indirect force causes mainly spiral or torsion fractures, possibly also with the formation of a flexible wedge, direct force tends to lead to transverse fractures or fractures, often with extensive debris. Only a small proportion of humerus shaft fractures (6.3% according to an AO collective study) are open fractures.
Upper arm fractures are very rare in children with around 0.75% of all bone fractures, unlike the fractures near the elbow. Since they occur far from the growth zones, there is no threat of growth disturbance. Side-to-side shifts are usually well balanced in further growth - depending on age - but axial deviations of more than 10 ° in the frontal and sagittal planes should be corrected. Delayed bone fracture healing or pseudarthroses practically do not occur in children.
Accompanying injuries
The extent of the possible accompanying injuries also depends on the course of the accident: In the case of direct trauma, there may be significant injuries to the muscles and subcutaneous fatty tissue in the form of tears, décollement or hemorrhages, which in individual cases can also lead to a compartment syndrome .
In the case of indirect trauma, injuries to the radial nerve or the large blood vessels due to sharp-edged fragments or trapping in the fracture gap must be expected. The radial nerve is fixed in a bony groove in the middle third of the shaft, which predominantly leads to overstretching with neuropraxia . Studies found a frequency of radial paralysis between 10.3% and 27% in upper arm fractures. In a study with 28 primary and 7 secondary nerve damage, six overextensions, seven contusions, six hemorrhages in the nerve and only one impaling were found.
Diagnosis
Basic diagnostics
The clinical diagnosis is usually easy to make: pain in the fracture area, lost active mobility in the elbow joint, sometimes also in the shoulder joint, as well as the abnormal mobility in the shaft area of the upper arm, combined with palpable crepitations ("crunching") during passive movement, are all sufficient clinical evidence of the presence of a humeral fracture. The X-ray image in two planes provides final certainty and shows the course of the fracture sufficiently reliably for treatment planning. Additional examinations such as computed tomography are only necessary in rare exceptional cases - unless joint involvement cannot be ruled out with certainty on the basis of the X-ray images.
The clinical examination also extends to the blood circulation and nerve supply of the forearm and hand. In particular, the function of the radial nerve is usually assessed and documented during the first clinical examination.
Additional diagnostics
If there is no pulse in the radial artery and / or ulnar artery , if there are clinical signs of ischemia (insufficient blood flow), an ultrasound Doppler or duplex examination may be necessary. If there are indications of insufficient blood flow in these arteries, angiography is usually performed in case of doubt to determine the type and location of the vascular damage.
Damage to the radial nerve can be visualized using EMG . In practice, this is usually not done due to time constraints, since the nerve lesion is usually well recognizable clinically (→ radial paralysis ).
treatment

“The humerus shaft fracture is the most benign of all shaft fractures of the long tubular bones. With the appropriate dressing technique, apart from very rare exceptions, it can almost always be treated conservatively in the simplest way. You just have to know that creating a corresponding shortening of 1–10 mm is the most important task of bone fracture treatment and that, for example, in the case of transverse fractures, displacements by the full shaft width with shortening are functionally and cosmetically insignificant if there is no significant axis buckling and twisting. "
Since the development of new intramedullary osteosynthesis procedures in the 1990s, this long-standing principle of Böhler can now be put into perspective, but should not be forgotten. The astonishingly rapid healing tendency of upper arm fractures, especially spiral fractures, is still offset by the risks of nerve injuries caused by surgical therapy.
Since the mid-1990s, conservative therapy can no longer be regarded as the standard therapy for uncomplicated upper arm fractures. The modern intramedullary surgical procedures have established themselves here.
“To date, there are no evidence-based therapy schemes or guidelines. Prospective randomized studies are largely lacking. The randomized prospective studies that have now appeared in the more recent literature show a trend towards conservative therapy. However, the study collectives are small and do not yet allow direct implementation. While anatomical reduction and osteosynthetic stabilization should be aimed for in younger patients, primary prosthetic restoration is also discussed in older patients. Depending on the procedure, shoulder stiffness, humeral head necrosis, pain, infections, loss of reduction and “cutting-out” can occur. Based on the current data, the treatment of the proximal humerus fracture remains individualized. A therapy decision must always be made with the patient in view of their individual needs and characteristics. "
Conservative therapy
Conservative therapy is still important for patients with a greatly increased risk of surgery or for those who refuse surgery.
If carried out correctly, good to very good healing rates can be achieved with conservative treatment. A short inpatient or even primarily outpatient treatment is often sufficient. The complication rate is low, and iatrogenic damage to the radial nerve (caused by medical intervention) is rare. The cosmetic and functional result is - in the absence of surgical scars - good, the treatment costs are low.
The disadvantages of the conservative approach are the risk of elbow or shoulder stiffness due to weeks of restriction of mobility, misalignment of the axes and restrictions in personal hygiene. Pseudarthroses (false joint formation) due to insufficient bone fracture healing can occur with conservative as well as surgical treatment; their frequency is stated very differently in the literature.
A number of procedures have been specified for the conservative treatment of humerus shaft fractures:
- Simple immobilization by fixation on the thorax with a Desault or Gilchrist bandage
- Application of an upper arm plaster splint with shoulder and elbow inclusion ( coaptation splint )
- Immobilization in a forearm cast with elbow inclusion ( hanging cast ); Here, the treatment principle consists of using the dead weight of the plaster of paris and forearm to prevent shortening and fixing the wrist with a sling to avoid rotation errors
- Immobilization on a thoracic abduction splint: here the upper arm is fixed on a splint in about 90 ° abduction (lateral spreading) with 90 ° flexion in the elbow joint; this method is hardly practiced any more due to the severely limited patient comfort.
The most modern approach is the functional treatment using a Sarmiento brace . This is a made-up plastic sleeve that is precisely adapted to the upper arm. The brace exerts gentle pressure on the soft tissue jacket and thus holds the fracture in an axially aligned position. Elbow and shoulder joints remain free, which prevents the joints from stiffening. The brace is put on as soon as the first connective tissue contact of the fracture surfaces can be assumed, ie about 10-14 days after the trauma. Until then, the patient is immobilized by means of a Desault or Gilchrist bandage.
Operative therapy
Indications for surgical treatment
The absolute indication for surgical treatment are:
- Open fractures or closed fractures with severe soft tissue damage
- Multiple fractures on the same arm ("chain fractures")
- Fractures of the opposite arm
- Endangerment of muscles, blood vessels or nerves from insufficiently repositioned fracture fragments
- Concomitant chest injuries or pre-existing breathing disorders due to concomitant diseases
- Restriction of movement of a neighboring joint due to previous damage
- Upper arm fractures near the joint, both in the humeral head area and in the area near the elbow
- Fractures as part of a multiple trauma
- Poor reduction results, for example, due to the entrapment of muscles in the fracture gap or due to widely blown fragments
Most authors do not consider primary damage to the radial nerve, which is not all too seldom caused by crushing or pulling on the nerves, to be a mandatory indication for surgery, since it is often a matter of temporary functional disorders without substantial damage to the nerve; up to 90% of these pareses resolve spontaneously in the further course. In contrast to this, the secondary paresis of the radial nerve, which shows up after the fracture has been established for conservative treatment, is an absolute indication for surgery, since it must be feared that the nerve will become trapped between the fragments during the reduction. A wide range of procedures is available for the surgical treatment of upper arm fractures, which are specifically applied taking into account the shape of the fracture and the soft tissue conditions, but also the accompanying circumstances and diseases as well as the patient's ability to cooperate. Basically, all of these osteosynthesis procedures can be assigned to two main groups, the extramedullary and the intramedullary procedures.
Extramedullary surgical procedures
Plate osteosynthesis and the external fixator are mainly used as extramedullary surgical procedures . Angle-stable plates have also been used for special fracture forms, especially for fractures very close to the joint, since the 1990s.
The plate fixation , which was usually carried out with TLC plates (dynamic compression plates), was the standard procedure for the surgical treatment of humeral shaft fractures in German-speaking countries from the late 1970s to the 1990s. The large-scale application of the process also made its method-specific problems clear:
- The radial nerve runs below the triceps brachii muscle and crosses the humerus shaft, directly on top of it, approximately at the transition from the distal to the middle third. The nerve must be exposed with subtle dissection and safely protected. This is already difficult with a fresh piece fracture, as bleeding into the muscles and connective tissue often makes reliable identification difficult. The search for the nerve becomes even more problematic when removing the osteosynthesis material, as it crosses the plate and is often encased in very coarse scar tissue.
- The "watertight" and therefore very rigid plate fixation preferred from the 1970s to the late 1980s can lead to circulatory disorders of the bone in the fracture area, which favors an increased incidence of delayed bone fracture healing up to the formation of pseudarthroses (false joints). In this context, material breakage or plate breakouts can also occur.
For these reasons, plate osteosynthesis has largely been abandoned in favor of modern, intramedullary procedures.
An exception are distal and proximal shaft fractures, which do not allow a secure locking of a nail due to the lever relationship. Plate osteosynthesis is therefore still used in the distal area, while angle-stable titanium plates have increasingly been used in the proximal area since the 1990s .
- The locking plate on the proximal humeral shaft
Intramedullary procedure
The principle of medullary splinting was established by several surgeons in the middle of the 20th century: In 1940 Küntscher introduced the slotted intramedullary nail he had developed in the treatment of shaft fractures of long tubular bones; a similar nail was developed by Seidel and has been in use for a long time. Since 1939, Rush has been stabilizing shaft fractures with a special, strong wire (“Rush pin”); the procedure is now increasingly used again with highly elastic titanium wires ("Prévot nails"), especially for fractures in children.
Bundle nailing
Hackethal took a different approach , which brought in a bundle of several elastic, approximately 2 mm thick steel wires that were jammed in the medullary canal. The Ender nailing follows the same principle.
Locking nail
The treatment of humeral shaft fractures with intramedullary nails such as the Küntscher nail presented various problems: rotational stability could not be guaranteed, only in the central shaft area was it possible to achieve adequate clamping of the nail in the medullary canal, and fractures or fissures occurred at the nail entry points Overheating damage found when reaming the medullary canal. When the nails were introduced from the humeral head, impingement of the shoulder joint occurred in many cases .
Therefore, methods have been developed to alleviate these problems. A number of nails have been developed that lock proximally and distally. One example is the Seidel nail, which has been in use for a long time: it had a cloverleaf-shaped profile, was locked with 2 screws in the area of the impact point and had three expanding lamellae at the distal end that fixed the nail in the medullary canal with a cone. It could be introduced from both the elbow (distal) and the humeral head (proximal). The results with this nail type were assessed differently in different studies; In addition to very good functional results - even with pathological fractures and pseudarthroses - complications such as fractures at the impact site, impingement syndromes on the humeral head and loosening of the locking screws and the expansion mechanism occurred.
These problems could also be observed with other, similar systems and, in the late 1970s to early 1990s, led to the preference for plate osteosyntheses, which were also common for many other fractures at this time. Only the development of locking nails made of titanium , which can be inserted undrilled with a slim cross-section and ensure rotational stability by means of secure proximal and distal locking, has led to increasing use of these intramedullary procedures since the 1990s. The stable lock in the humeral head prevents the nail from protruding proximally and thus the development of an impingement. Damage to the radial nerve when inserting the locking bolts is largely avoided by the design of these nails with the appropriate technique.
In children, two opposing metaphyseally inserted dynamic intramedullary nails (ESIN) are often used for intramedullary stabilization.
External fixator
The external fixator ("external tensioner") is used less frequently to treat humerus shaft fractures than the aforementioned internal fixation methods. However, it offers undisputed advantages in certain situations:
- With open fractures with significant destruction of the soft tissue, there is a greatly increased risk of bone infections. This can largely be avoided by using the fixator, whose nails are inserted far from the fracture zone via minimal skin incisions. The soft tissue injury remains accessible for surgical repair without the ostesynthesis material in the wound area being able to promote the occurrence of infections.
- This also applies to fractures in the area of other skin and soft tissue injuries, such as burn injuries.
- The external fixator can be attached easily and without any special demands on the position. Therefore, it is often given preference in the care of multiple injured patients (multiple trauma ): The high achievable stability facilitates the care of the patient and enables early passive and active exercise treatment.
- Comminuted fractures near or beyond the joint sometimes do not allow stable treatment using screws, (angle-stable) plates or intramedullary procedures. In these cases, good external stability is primarily achieved with a cross-joint fixator.
As with other fractures, the external fixator is often only used as a primary stabilizing measure and the fracture is definitively treated at a later point in time as a change of procedure.
Individual evidence
- ↑ A. Rüter et al. (Ed.): Accident surgery. 1st edition. Urban & Schwarzenberg, Munich / Vienna / Baltimore 1995, ISBN 3-541-17201-0 , p. 497.
- ↑ a b L. von Laer: fractures and dislocations in growing age. 3. Edition. Georg-Thieme-Verlag, Stuttgart 1996, ISBN 3-13-674303-2 .
- ↑ B. Weigel, M. Nerlich: Praxisbuch Unfallchirurgie . Springer-Verlag, Berlin 2005, Volume I, ISBN 3-540-41115-1 , p. 308 f.
- ↑ O. Kwasny et al. a .: Procedure for humerus shaft fractures with primary or secondary radial damage. In: Trauma Surgery. 1992. 18, pp. 168-173.
- ↑ Lorenz Böhler In: Against the operative treatment of fresh upper arm fractures. 1964; quoted from: A. Rüter et al. (Ed.): Unfallchirurgie. 1st edition. Urban & Schwarzenberg, Munich / Vienna / Baltimore 1995, ISBN 3-541-17201-0 , p. 496
- ↑ Burkhart KJ, Dietz SO, Bastian L, Thelen U, Hoffmann R, Müller LP: The treatment of proximal humeral fracture in adults. Dtsch Arztebl Int 2013; 110 (35-36): 591-7. doi : 10.3238 / arztebl.2013.0591
- ↑ Ch. V. Goldammer: The therapy of the humeral shaft fracture - a retrospective study to evaluate conservative and operative treatment results. (PDF; 1.83 MB) (No longer available online.) 2001, pp. 12–13 , formerly in the original ; Retrieved February 21, 2010 . ( Page no longer available , search in web archives ) Info: The link was automatically marked as defective. Please check the link according to the instructions and then remove this notice.
- ↑ Scharf, Rüter: Orthopedics and trauma surgery. 2009, p. 487.
- ↑ K. Brehme: The therapy of humeral shaft fracture results with special consideration of the UHN. (PDF; 1.86 MB) (No longer available online.) 2004, p. 7 , formerly in the original ; Retrieved February 21, 2010 . ( Page no longer available , search in web archives ) Info: The link was automatically marked as defective. Please check the link according to the instructions and then remove this notice.
- ↑ a b c Ch. V. Goldammer: The therapy of the humeral shaft fracture - a retrospective study to evaluate conservative and operative treatment results. (PDF; 1.83 MB) 2001, accessed on May 4, 2014 .
- ^ Karl Heinz Hackethal : The bundle nailing: Experimental u. clin. Study on e. novel method d. Medullary canal splinting of long tubular bones. Guide d. Technology , Springer-Verlag, Berlin / Göttingen / Heidelberg 1961, DNB 451751809 .
literature
- H.-P. Scharf, A. Rüter (Ed.): Orthopedics and trauma surgery. Elsevier Urban & Fischer, Munich / Jena 2009, ISBN 978-3-437-24400-1 .