Screening
Under screening is a systematic test method, which is used to filter elements within a defined test area having certain properties. The method can consist of a test or a series of coordinated tests that the persons or samples tested undergo. The challenge of screening tests is to "find the needle in the haystack".
Origin of the term is the English. “To screen”, which can be paraphrased as: “bringing something onto the screen”, with the transferred meaning “bringing something to attention”. A medical screening examination is also referred to in German as a filter examination, a police examination as a raster search .
The term is used in the following areas:
- Preventive medicine : Screening is used here to search for diseases in a defined population group.
- Psychological diagnostics and empirical social research : Using questionnaire tests, people with certain characteristics are "filtered out".
- Pharmaceutical research , biotechnology and chemical research: Screening is used to filter out individual substances with specific properties from a large number of possible substances, genes or organisms ( high-throughput screening ).
- General language: Both in everyday life and in any specialist field, the term is used to describe the process of looking through a large number of elements to identify certain elements from them or from gaps, see e.g. B. Accession Conference #accession procedure .
Medicine / psychology
In preventive medicine, screening is partly carried out in the form of series examinations , partly continuously in the medical and nursing practice. For as many people as possible, the earliest possible information about the probability of the presence of certain diseases or risk factors should be made possible. This is usually referred to as a check -up. If abnormal values are present, the presence of the disease must be confirmed by subsequent diagnostic examinations .
If a person visits a doctor because of existing symptoms, one no longer speaks of screening. If an illness is to be detected or ruled out due to often unspecific symptoms, a comprehensive medical examination is always necessary. Sometimes the everyday meaning of screening is used here.
target
The aim of a screening program in preventive medicine is to extend the life expectancy of the population group with an increased risk of disease. In order to achieve this goal, the largest possible number of test subjects must be examined in order to discover as many sick people as possible and to be able to provide treatment. As part of the newborn screening , an attempt is even made to identify all carriers of a certain disease in order to enable them to lead a normal life.
In the context of precise questions, as many asymptomatic people with existing problems who did not know about these problems before the screening examination should be identified and given treatment or encouraged to change their lifestyle.
Screening challenges
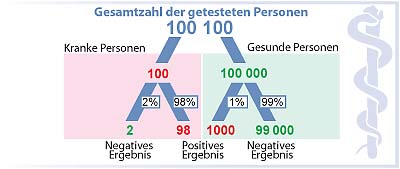
A schematic example is intended to illustrate the challenges that arise when individual asymptomatic carriers of the disease are to be identified with a test in a large group of healthy people:
- 100 out of 100,100 people (the basic proportion in this case corresponds to one in 1001) are asymptomatic carriers of an illness. The disease is detected correctly with a test to 98% ( sensitivity ), the healthy are recognized to 99% ( specificity ) as healthy. So the test is very reliable. It was positive for you. Is there reason to be seriously concerned (see also positive predictive value )? The representation takes place with a decision tree .
The test result :
The test result is positive : 98 people are rightly recognized as sick - 1,000 healthy people are wrongly identified ( false positive ). The test found 1098 people in this example, of which 98 can be helped, but you do not know which 98 of the 1098 people; further clarifying investigations are necessary for this (see also: conditional probability ).
- So 99,000 are rightly recognized as healthy - 2 sick but wrongly ( false negative ). In this example, if the test is negative, the majority can assume that they are not sick. Two of them will get sick later.
In a real screening, both the frequency of the disease in the population ( prevalence ) and the sensitivity and specificity can differ from this example. The benefit of a screening can be clearly described by the number of tests that are necessary to save a life. With any screening, knowing the frequency of the disease is critical in order to be able to interpret the test results. If this is unknown, the question of false positive and false negative test results cannot be answered.
Requirements for screening programs
Medical screening is aimed at the whole population, i. H. to all men and / or women of a certain age, most of them in intact health. Therefore, the principle of " no harm" in medical ethics is very important and screening programs must meet high requirements:
- the disease must be of concern to the health of the population
- it must be treatable and the prognosis must be significantly better if treatment begins earlier in the course of the disease.
- the test procedure should have a high sensitivity and specificity , d. H. the test should be able to detect or exclude the disease you are looking for (the existing risk factors) with the greatest possible certainty.
- the examination should be time and cost effective.
- the examination should burden the person to be examined as little as possible.
Each of these points must be fulfilled so that a screening program can be carried out meaningfully. The last point is particularly important: screening programs in preventive medicine must be accepted by patients in order to be successful. The quality assurance of screening programs is of particular importance here.
advantages
- A disease is discovered at an early stage that is easy to treat: it can be cured more often or with less effort
- Treatment at an early stage affects the quality of life to a lesser extent (in the early stage it is often possible to avoid radical surgery or chemotherapy ).
- Treatment of the early stage has lower costs.
- Consequential damage is often prevented.
- The examined person is reassured by an inconspicuous result.
disadvantage
- The possible burden of the examination itself or unavoidable statistical uncertainties, so-called false negative results. Here, both examiners and examiners are wrongly reassured, possible signs of the disease may be misinterpreted or the purpose of early diagnosis of a disease is simply missed.
- When false positive results patients are troubled unjustly, and expensive, the patient and the health care onerous follow-up studies are the result.
- Early stages of a disease may be diagnosed, the early detection of which does not extend the lifespan, but whose unnecessary treatment reduces the quality of life (see ductal carcinoma in situ in mammography and deaths from therapy in neuroblastoma screening)
Examples of screening tests
- Newborn screening among others
- Chlamydia screening
- Mammography screening
- Cervical cancer using the Pap test
- Prostate cancer , using PSA test ( prostate-specific antigen )
- Colon cancer using the haemoccult test or colonoscopy
- Hearing loss in children
Further tests from clinical practice
- Microbial Screening
- Periodontal Screening Index (PSI code for determining gum disease)
- Risk factors for cardiovascular disease
- Glaucoma Screening
- Cataract (medicine) screening as part of an eye camp
- Triple test
- First trimester screening
- NT screening
Evaluation of screening studies
The objective of a screening initially seems plausible: a disease or disorder can be detected earlier and thus there is a better chance of recovery. The risks have to be carefully weighed against those inherent in the consequences of false negative and false positive results. Before starting a screening program, it must be determined whether the program will generate more benefits than costs. This is done by means of scientific studies that must meet rigorous criteria, for example must be randomized . The benefit must be proven in the form of an absolute risk reduction .
The results of a screening study can be falsified by various factors and lead either to falsely better results or to false, worse results that cannot be implemented in daily practice.
Some authors suggest that the potential benefits of screening methods are generally overestimated and the harm is underestimated.
Lead time adulteration
The lead time falsification can lead to an overestimation of the positive effects of screening. The purpose of screening is to identify a disease as early as possible. However, if cases of illness are recorded and treated, the carriers of which would have lived as long or longer without treatment, this is called overdiagnosis. This harms the person in several ways: diagnostic and therapeutic interventions reduce their quality of life; from then on she had to live with a diagnosis of a fatal disease; the costs of medical care are unnecessarily increased. The lead time falsification cannot be proven in individual cases, as it cannot be proven in retrospect how the course would have turned out without treatment. This effect can only be assessed in controlled studies and if the natural course of a disease is known.
Adulteration by the type of disease being examined
Many screenings include early detection of certain cancers. It is believed that slowly growing tumors have a better chance of survival for the patient than fast growing tumors. However, this means that screenings are far more likely to detect slow- growing tumors than those that have a more drastic impact on the patient's life - because rapidly growing tumors can cost the patient their life before they have the opportunity to be screened.
As a result, screenings tend to detect cancers that are less likely to be life-threatening for the patient. A non-life-threatening tumor disease often means that the patient dies of something other than the tumor itself - so the screening in such a case did nothing to prolong life (see also indolent tumor and tumor Dormancy ).
Falsification by the selection of subjects
Not all men and women participate in screening - therefore study participants must be carefully selected to ensure the statistical significance of the results. People who know they are at greater risk because of cancer deaths in their families, for example, take part in a screening study more often than others. As a result, screening studies present the population's health situation worse than it actually is.
The same problem can work in the opposite direction: if a test is more likely to be available to richer or younger people, then those people are more likely to participate - for example, if a long trip to the screening center puts off frail and poorer people. In this case, fewer diseases are diagnosed in percentage terms than in reality because the rich can afford better health care anyway and because younger people suffer less from cancer or cardiovascular problems.
Falsification through superfluous diagnoses
Screening can identify abnormalities that would never play a role in a person's life. An example is prostate cancer - this cancer doctors say "Most men die with prostate cancer, but not in prostate cancer." Autopsies on deceased men have shown that a large proportion of the deceased had microscopically detectable prostate cancer cells, but without dangerous tumor formation until the time of death.
Apart from the risk of a patient receiving unnecessary treatment - cancer therapies can have a massive impact on the patient's quality of life - too frequent, superfluous diagnoses can mean that screening appears to be more effective than it is, measured in terms of the effective life extension of the test subjects , is. The discovery of a harmless abnormality in a patient therefore makes no sense from either an economic or a medical point of view.
Reduction of falsifications
In order to be able to solve these screening challenges, screening tests must be checked by controlled randomized studies before a screening program is introduced across the board. The studies have to be strictly random and the number of participants has to be very large. The methodology of the examination must be strictly defined so that the diagnoses made by different doctors in different hospitals are qualitatively equivalent. The exact description of the working method in clinical studies is often recorded in a standard operating procedure manual.
Individual evidence
- ↑ Angela Raffle, Muir J. Gray: Screening ., German annotated translation, Ernst Huber Verlag, Bern 2009, ISBN 978-3-456-84698-9 .
- ↑ Venereal disease: chlamydia - the underrated infection. In: Spiegel online. August 30, 2017. Retrieved August 30, 2017 .
- ↑ Mühlhauser, I. (2014). To overestimate the benefits of prevention. Journal for Evidence, Education and Quality in Health Care, 108 (4), 208–218. P. 3.
- ^ Frankfurter Rundschau The price of early diagnosis, July 30, 2010, accessed on October 24, 2013.
Web link
- Spix, C .; Blettner, M .: Screening . In: Dtsch Arztebl Int . No. 109 (21) , 2012, p. 385-90 ( review article ).