Symptothermal method
The Symptothermal Method is a contraceptive method of natural family planning that is based on determining the fertile days of the woman's menstrual cycle . Cyclical fluctuations in basal temperature and changes in the cervical mucus or the cervix are evaluated. The Symptothermal Method is a combination of the Temperature Method and the Billings Method .
The contraceptive reliability of the Symptothermal method is very high in the case of sexual abstinence during the fertile days, in the case of the Sensiplan method with a Pearl index of 0.4. The logging and interpretation of the measurement results can be supported by software or a contraceptive computer .
Conversely, the symptothermal method is also suitable for determining the fertile days in the event of a desire to have children and for maximizing the probability of conception.
Explanation of the methodology
Ovulation occurs about twelve to sixteen days before the onset of menstrual bleeding , during which an egg cell passes into the fallopian tube and is capable of fertilization for about six to twelve hours . If there is no fusion with a sperm during this time , the egg cell dies and pregnancy does not occur in this cycle . Sperm can generally remain fertile in the uterus and the cervix for up to three days, and in exceptional cases for up to five days. Therefore, fertilization can only occur up to five days before and twelve hours after ovulation. The aim of the symptothermal method is to determine as precisely as possible the short fertility window that results from the survival time of the sperm and egg cell.
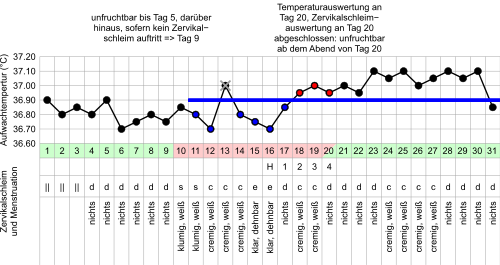
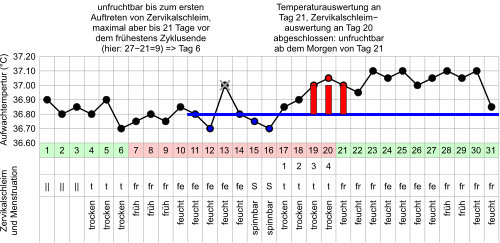
The basal temperature fluctuates depending on the menstrual cycle and increases by a few tenths of a degree shortly after ovulation due to the action of progesterone (see graphic). The rise in temperature divides the cycle into a low level, which roughly corresponds to the follicular phase , and an high level, which roughly corresponds to the luteal phase .
If the temperature method is used exclusively , high demands are placed on the way in which the measurement results are evaluated. With the symptothermal method, these requirements are somewhat lower, as it is secured by another body sign, the cervical mucus or the cervix.
As with the Billings Method , the nature of the cervical mucus is used to determine when ovulation is approaching. The cervix secretes mucus, which is subject to characteristic changes in the course of the cycle: In the first half of the cycle, cervical mucus is viscous, creamy, sticky, of a sticky consistency - one also speaks of inferior or poor quality cervical mucus. A mucous plug can act as a natural barrier to close the cervix. When the estrogen level is high , however, it becomes thin, (glass) clear and possibly stringy - it is then cervical mucus of the best quality. In the second phase of the menstrual cycle, the spinnability is reduced again under the influence of progesterone . The course in the cycle differs from woman to woman, and the characteristic changes in the cervical mucus are not always observed.
If the assignment of the cervical mucus causes difficulties, the woman can fall back on the observation of the cervix instead. Around the time of ovulation it is soft, slightly open and high in the vagina because of the high level of estrogen. In the second phase of the cycle it is hard, closed and deep. Some contraceptive computers supplement the measurement of temperature and cervical mucus on about four to eight days of the cycle with the determination of the FSH or LH peak using test strips to determine hormones in the morning urine.
If it can be determined with certainty that ovulation has occurred, the second phase of the cycle is sterile. Depending on the length of the luteal phase, which is between ten and sixteen days, eight to thirteen days are sterile even with very irregular cycles. The time before ovulation is generally considered to be potentially fertile. However, there is another infertile phase at the beginning of the cycle, well before ovulation. It is determined by the estrogen symbol in combination with elements of the calendar method. In the case of irregular or short cycles, the rules mean that no sterile phase may be assumed at the beginning of the cycle. With regular cycles of at least 27 days, the infertile period is often five to ten days long. There are adapted rules for very long or irregular cycles during breastfeeding and menopause.
The temperature evaluation can be made more difficult by infections , alcohol consumption , stress , jet lag , lack of sleep or shift work . The result of the cervical mucus observation can be falsified by drugs. However, the user can learn to assess these disruptive factors. They do not make the method more unsafe, but they reduce the number of days that can be considered sterile.
Overview of different symptothermal methods
The symptothermal methods were preceded by the development of the Knaus-Ogino or calendar method , Billings method and the temperature method . In 1965 Rötzer published the first symptothermal method. Another method from Thyma followed in 1973. During the same period, different authors combined elements of the billings, temperature and calendar method. Today there are a large number of symptothermal methods in different countries, the rules of application of which differ in details and whose contraceptive safety has been studied to varying degrees.
The method rules according to sensiplan, Rötzer, Weschler and Nofziger are common in German-speaking countries. For some time now, they have been supplemented by contraceptive computers and evaluation software for PCs or smartphones, some of which follow their own and unknown sets of rules.
The method rules differ for the temperature evaluation and the cervical mucus evaluation. They give different instructions for temperature measurement with regard to measurement duration and time. When evaluating the temperature, there are differences in the height at which an auxiliary line is drawn; the last six measurements or the last six days are sometimes used as reference values. The different names for the auxiliary line (coverline, baseline etc.) are also used as trademarks for the different sets of rules. In particular, whether and under what conditions individual measured values from the lower elevation may be ignored during the evaluation differs depending on the set of rules. The number and position of the higher measured values up to the end of the evaluation also differ.
In the case of cervical mucus, the main difference is the division into different categories. The individual methods have a different number of categories (usually four or five) and individual properties are not always assigned to the same high or low categories. In agreement, cervical mucus, like raw egg white (transparent and elastic), belongs to the best mucus category in all regulations, and cervical mucus, whose color and consistency is reminiscent of Niveacreme , to a lower category. With other observations, however, there are contradicting classifications. Aqueous-liquid cervical mucus, such as slightly thickened milk or very liquid sunscreen, belongs to the lower mucus category at NGK and TCOYF, while at sensiplan, sympto and Rötzer liquid cervical mucus always belongs to the highest category. A runny sensation inside the vagina belongs to the very low category f with Rötzer, whereas with sensiplan a runny sensation at the vaginal entrance belongs to the highest category S + and with NGK to the second highest category “moist”. Spotting is one of the highest cervical mucus categories at sensiplan, but is ignored for sympto and NGK. The forms of observation also differ. Mucus in the underwear or the sensation inside the vagina is not included in the evaluation in all methods.
Some methods have a strong medical-scientific background, others have developed from feminist or ecological to esoteric circles or with the aim of marketing a contraceptive computer. Separate studies on contraceptive safety do not exist for all regulations. However, the existing studies are often used as an argument for the safety of other methods.
Sensiplan
Sensiplan was developed at the Heinrich Heine University in Düsseldorf from 1981 and has been taught since 1987 by the NFP working group of the Maltese under the control of the then Federal Ministry for Youth, Family, Women and Health through courses or the book Naturally and Safe . Today the scientific supervision is at the Ruprecht-Karls-Universität Heidelberg . Originally the method was called Natural Family Planning , the Maltese had the brand name sensiplan protected for their method, which has been used since 2010. There are targeted attempts to make the method better known among gynecologists in private practice.
One study found a Pearl Index of 0.4 with two pregnancies in 6,022 cycles in which the couples were abstinent. Another two pregnancies occurred in 4375 cycles in which barrier methods were used (Pearl index 0.6). After adjusting the rules for the end of the infertile period at the beginning of the cycle, three pregnancies in 7866 cycles with abstinence (Pearl index 0.5) and one pregnancy in 2917 cycles with barrier methods (Pearl index 0.4) were determined. The safety of use, which also includes incorrect use, was 15 pregnancies in 12386 cycles with a Pearl index of 1.6.
According to the sensiplan set of rules, the web software and smartphone app MyNFP, developed by Christian Korscheck, as well as the smartphone app Lady Cycle offer an automatic evaluation of the cycles.
Method rules (shortened):
The temperature measurement takes three minutes and takes place before getting up. If the woman breaks her night's sleep, the woman must have rested for at least an hour before the measurement. Increased measured values may only be ignored if they both protrude from the underground level and can be explained by a known disruptive factor. The regulations at sensiplan are more precise and stricter than the other regulations. Any number of measurement gaps are possible. The auxiliary line is drawn through the highest of the last six measured values not in parentheses. The temperature evaluation is completed on the evening of the third day when all three measured values are above the auxiliary line, the third of which at least 0.2 ° C above the auxiliary line. There are two exception rules for a slower temperature rise.
There are five categories of cervical mucus (t, Ø, f, S, S +) and another category for women for whom the classification into S and S + is too rough. The visible mucus at the vaginal entrance, the tactile sensation at the vaginal entrance and the sensation at the vaginal entrance flow into the observation. The evaluation is completed on the evening of the third day after the change to a poorer mucus quality.
A new cycle is started with each bleeding at normal menstrual strength. An infertile period at the beginning of the cycle only exists if ovulation occurred in the previous cycle. It ends when cervical mucus at least category f is observed for the first time, but no later than eight days before the first day of increased temperature in the previous cycles (diagram: day 15). If no values of at least twelve cycles are available, the fifth day of the cycle is assumed as an alternative. Special rules for the assessment apply after discontinuation of hormonal contraceptives, pregnancy or if a menstrual calendar has already been kept.
Natural conception regulation (NER) according to Rötzer
The Austrian doctor Josef Rötzer developed natural conception regulation from 1951, financed by the Austrian Bishops' Conference. He was the first to combine cervical mucus and temperature. This method was first published in the book Kinderzahl und Liebesehe . This book was continuously developed and is now only called Natural Conception Control . The method is taught today by the Institute for Natural Conception Control (INER), founded in 1986. In one study, two pregnancies occurred in 3542 cycles (Pearl index 0.7). In the case of an extended sterile period at the beginning of the cycle including user errors, a Pearl index of 0.9, determined from over 30,000 cycles, is given. If the 6-day rule is restricted, less than one pregnancy for 6,000 cycles (Pearl index 0.2) is stated. In over 200,000 cycles, not a single pregnancy occurred during the infertile period of the second cycle phase (Pearl Index 0).
Method rules (shortened):
The temperature measurement takes five minutes and takes place in the morning after at least six hours of sleep. Elevated values may be excluded. The baseline is drawn through the highest of the last six (or less, if parentheses are found below) readings up to and including the day the mucus peaked. The temperature evaluation is completed on the evening of the day on which three successive measured values are above the auxiliary line, the third of which at least 0.2 ° C above the auxiliary line. There are two exception rules for a slower temperature increase and a special rule for a temperature increase before the mucus peak.
There are four categories of cervical mucus (t, Ø, f, S), whereby S is additionally divided into two categories (w, mi, cr, kl, g, gbl) and (EW, gl, fl, ns) by means of an abbreviation. The visible mucus at the vaginal entrance, the tactile sensation at the vaginal entrance and the sensation at the vaginal entrance and inside the vagina flow into the observation. Since the temperature evaluation was carried out depending on the peak of the mucus (change to a worse category), there is no need for an independent mucus evaluation.
A new cycle is only started with a menstruation that follows ovulation. The first six days of the cycle are considered sterile unless cervical mucus is observed. Women who are capable of so-called fine sensation inside the vagina (cervical mucus category f) can extend this time until the first sensation of f.
Taking Charge of Your Fertility (TCOYF) according to Weschler
Toni Weschler, MPH, has been teaching fertility awareness since 1982 and has written the book Taking Charge of your Fertility . It is based on existing method rules, but changes them. Because of the wide range of information on women's health and fertility, this American book is also widespread in the German-speaking world. There is no separate safety study.
Method rules (shortened):
The temperature measurement with digital thermometers takes 60 to 90 seconds and takes place before you get up. A coverline is drawn 0.05 ° C above the highest of the last six low-lying values. A single higher temperature value may be ignored. The temperature evaluation is completed on the evening of the day on which three consecutive values are above the coverline. There is a stricter rule in the application in order to have greater security (at least one of the three values must be 0.2 ° C above the coverline) and one for a slow increase.
There are four categories of cervical mucus (dry, viscous, creamy, albumen). The visible mucus at the vaginal entrance, the tactile sensation at the vaginal entrance and the sensation at the vaginal entrance and stains in the underwear flow into the observation. The evaluation was completed on the evening of the fourth day after the change to a poorer mucus quality.
A new cycle begins with every bleeding at normal menstrual strength. There is an infertile period at the beginning of the cycle only if ovulation occurred in the previous cycle. The first five days of the cycle are considered sterile if there was ovulation in the previous cycle. In addition, the woman can assume infertility as long as she does not observe cervical mucus.
Natural birth control (NGK) according to Nofziger
The American Margaret Nofziger, one of the wives of Stephen Gaskin, who founded the large commune "the Farm" in Tennessee in 1997, wrote the book A cooperative method of natural birth control in 1976 to give women a natural and spiritual method of contraception. It was particularly common in hippie circles. The method is based on existing method rules, but changes them. There is no separate safety study.
Method rules (shortened):
The temperature is measured after waking up after at least three hours of sleep. The temperature evaluation is completed on the morning of the day on which the temperature is 0.2 ° C above the last six low-lying values for three consecutive days. One of the six values can be ignored even without a known disruptive factor. An additional 12 hours of fertility can be assumed for increased safety.
There are four categories of cervical mucus (dry, early, moist, spinnable). The visible mucus at the vaginal entrance, the tactile sensation at the vaginal entrance and the sensation at the vaginal entrance and inside the vagina, as well as stains in the underwear flow into the observation. The evaluation was completed on the evening of the fourth dry day.
The last sterile day at the beginning of a cycle is calculated from the shortest previous cycle minus 21. In the first six months, the fifth day of the cycle applies as an alternative. Until then, the woman is considered sterile unless she observes cervical mucus. After observing cervical mucus for the first time, in this phase she is again considered sterile from the evening of the fourth dry day.
Sympto (internet software and smartphone app)
Sympto, developed by the Swiss Fondation SymptoTherm, is internet software, is also available as a smartphone app and automatically evaluates the curves. In addition, the detailed presentation of the set of rules used, which is based on sensiplan, Rötzer and Huneger, also enables an independent evaluation. The software only requests the woman to measure the temperature on a few days in the cycle and also asks the goal of the cycle observation (desire for children, contraception, observation).
Method rules (shortened):
There are three categories of sensation inside the vagina and sense of touch at the vaginal entrance (T, F, G) and three categories of visible cervical mucus (E, sE, gE). They are grouped into four categories of cervical mucus. The day before the change to a worse category is called the high point day.
The baseline is drawn through the highest reading from the last six underground locations. The measurement may be missing or excluded on two of the six days. The evaluation is completed on the evening of the fourth day after the peak day, if by then three temperature values are above the auxiliary line. If the third value is already 0.2 ° C above the auxiliary line, the temperature evaluation will be completed earlier.
In addition, there is a special rule if the cervical mucus is not observed or the high day is absent or too far away from the rise in temperature. Operation in billing mode without temperature measurement is also possible.
A new cycle only begins with menstrual bleeding after ovulation. The first fertile day at the beginning of the cycle is the Döring-Rötzer cut-off date, seven days before the earliest temperature increase in previous cycles, provided that no cervical mucus has been observed by then.
cyclotest 2 plus (contraception computer)
In addition to a pure temperature method, the Uebe Medical contraceptive computer also allows symptothermal use in combination with cervical mucus or LH tests. Cyclotest 2 plus requires the temperature to be measured after at least five hours of sleep in a four-hour window. The measurement time is 60 to 90 seconds. Values raised by fever are ignored, no further handling of disruptive factors takes place. The cervical mucus observation is reduced compared to other methods; only the occurrence of spinnable cervical mucus is entered in the cycle computer. The manufacturer does not specify the exact evaluation routine. A separate safety study does not exist; the Pearl index for use in the pure temperature method is given by the manufacturer as 3, for symptothermal use with Pearl index 1. In a study on 15 cycles, the Cyclotest gave 2 plus 1.7% of the days incorrectly as sterile and 22.7% of the days as falsely fertile.
Safety of the symptothermal method
As with all contraceptive methods that require reliability in use, the possible safety of the method when used correctly and consistently and the actual pregnancy rate differ from one another.
The reliability of the symptothermal method is very high with a Pearl index of up to 0.4. The vast majority of unwanted pregnancies when using the symptothermal method result from sexual intercourse during the fertile period without using an additional contraceptive method or from the failure of the alternative contraceptive used during the fertile period.
Acceptance, advantages and disadvantages
The symptothermal method is non-invasive, it does not affect the hormonal balance , does not involve any health risks and does not cause any additional costs other than the purchase price for a thermometer . Both a clinical thermometer and a basal thermometer can be used for measurement, but only differs from a conventional clinical thermometer in that it has a larger scale and is therefore easier to read. It is important that the thermometer shows two places after the decimal point. The use of the symptothermal method cannot be determined and does not require the consultation of a doctor or the consent of the parents. In addition, regular observation of your own body makes it possible to gain insight into the functioning of your own cycle. If you want to have children later, the same methodology can also be used to optimize the chances of conceiving and also enables the early detection of pregnancy in the form of a permanent increase in the basal temperature at the beginning of the pregnancy.
The symptothermal method requires a certain amount of learning and the willingness to deal with your own body on a daily basis. The method is unsuitable for women in whom the partner does not support the decision for this method.
Some studies have found increased libido in women whose natural hormonal cycle is not suppressed by hormonal contraceptives during the fertile period just before ovulation. This is explained by evolutionary optimization, but could not be proven in all studies. In the days before the LH peak and on the day of the LH peak itself, sexual activity was more pronounced in women. The coitus frequency also increases in the follicular phase, passes through a maximum on the day of ovulation and then drops abruptly. Other studies found no cycle dependency. Objective parameters of sexual excitability were constant over the menstrual cycle. Other studies show that outside influences sometimes have a greater influence than the menstrual cycle. Couples deal with the fertile period very differently, in one study 34% were abstinent, 25% used barrier methods, 13% had unprotected intercourse (often limited to the beginning of the fertile period, where there is a lower probability of conception), 7% protected and unprotected sex, 6% genital contact or coitus interruptus . The Pearl index when using barrier methods was not significantly worse than the Pearl index for couples who were abstinent.
See also
- Natural family planning
- Temperature method
- Contraceptive computer
- Billings Method
- Knaus-Ogino contraceptive method
Web links
- Guidelines (PDF) of the German Society for Gynecology and Obstetrics
- Symptothermal method : Familienplanung.de - Information portal of the Federal Center for Health Education (BZgA)
Individual evidence
- ^ Gerhard Thews , Peter Vaupel: Vegetative Physiology. 5th edition. Springer, Heidelberg 2005. p. 542
- ^ A b c Elisabeth Raith-Paula, Petra Frank-Herrmann, Günter Freundl, Thomas Strowitzki: Natural family planning today: Modern cycle knowledge for advice and application. 4th edition. Springer, Berlin / Heidelberg 2008, ISBN 3-540-73439-2 .
- ↑ a b c Maltese working group NFP (Ed.): Natural & Safe: The Practice Book. Safe conception management with no side effects. Family planning with sensiplan. With the right timing to the desired child. 18th edition. Trias, 2011, ISBN 3-8304-3558-4 .
- ↑ a b Josef Rötzer: Number of children and love marriage. A Guide to Regulating Conception . Herder, Vienna / Freiburg / Basel 1965.
- ↑ Paul Thyma: Fertile and Infertile days in married life . Raritan Printing, Fall River MA 1973.
- ↑ Paul Thyma: The Double-Check Method of Natural Family Planning . Raritan Printing, Fall River MA 1976.
- ^ Anna M Flynn, Melissa Brooks: A manual of natural family planning . Hemel Hempstead, Allen and Unwin, 1984, ISBN 0-04-176004-2 .
- ↑ M. Pharand-Lapointe, F. Kavanagh Jazrawy: Planning yourfamily the ST-way . Serena, Ottawa, 1980.
- ↑ RJ Huneger: Comprehensive fertility awareness and natural family planning learning activities packet . St John's NFP Program, Milwaukee 1981
- ↑ JJ McCarthy, MC Martin, M. Gildenhorn M (1977) The sympto-thermal method. An instructional program with charts and test. Human Life Foundation of America, Washington DC
- ↑ Gerhard Döring: Natural methods of family planning: model project for scientific review and controlled communication (= series of publications by the Federal Ministry for Youth, Family, Women and Health . Volume 239 ). Kohlhammer Verlag, Stuttgart 1988, ISBN 3-17-010593-0 .
- ↑ Press release: NFP is now called sensiplan
- ^ Register information from the German Patent and Trademark Office
- ^ G. Freundl, P. Frank-Herrmann and E. Raith-Paula: Natural family planning . In: The gynecologist . 31, No. 5, 1998, pp. 398-409. doi : 10.1007 / PL00003132 .
- ^ P. Frank-Herrmann, C. Gnoth, S. Baur and T. Strowitzki: Natural family planning . In: The gynecologist . 39, No. 9, 2006, pp. 671-677. doi : 10.1007 / s00129-006-1876-4 .
- ↑ P. Frank-Herrmann, U. Sottong, G. Freundl and T. Strowitzki: CME further education • Certified further education: Natural family planning . In: The gynecologist . 43, No. 4, 2010, pp. 341-350. doi : 10.1007 / s00129-010-2541-5 .
- ↑ P. Frank-Herrmann, U. Sottong, G. Freundl and T. Strowitzki: Key topic: Natural family planning Sensiplan® - a modern, reliable method . In: The gynecologist . 44, No. 1, 2011, pp. 17-22. doi : 10.1007 / s00129-010-2659-5 .
- ↑ Petra Frank-Herrmann, Günter Freundl: Natural family planning: As safe as the pill? Archived from the original on November 2, 2012. Info: The archive link was automatically inserted and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. In: gynecology + obstetrics . 2, 2007, pp. 30-34. Retrieved October 14, 2012.
- ↑ a b c P. Frank-Herrmann et al .: The effectiveness of a fertility awareness based method to avoid pregnancy in relation to a couple's sexual behavior during the fertile time: a prospective longitudinal study . In: Human Reproduction . 22, No. 5, 2007, pp. 1310-1319. doi : 10.1093 / humrep / dem003 . PMID 17314078 .
- ↑ Josef Rötzer: On the history of natural conception regulation (From the calendar methods to the sympto-thermal methods) Taking into account the question: What is a real sympto-thermal method? 1997, http://online-zyklen.net/INFORMATION/geschichte_der_ner.pdf
- ↑ a b Josef Rötzer: Natural conception regulation. The partnership way - the sympto-thermal method . 30th edition. Herder, Freiburg 2006, ISBN 3-451-23983-3 .
- ↑ Roetzer Josef: Sympto-thermal method and family planning . In: Acta Med Rom. . 16, No. 30, 1978, pp. 339-348. PMID 12309198 .
- ^ Josef Rötzer: A prospective Sympto-Thermal Trial in Austria, Germany and Switzerland . Presentation, III International Congress IFFLP / FIDAF, Hong Kong, Nov 20-30 1983
- ↑ Roetzer Josef: The symptothermal Therman Method: Ten Years of Change . In: Linacre Quarterly . 45, 1978, pp. 358-374.
- ↑ Toni Weschler: Taking Charge of Your Fertility . William Morrow Paperbacks, 2006, ISBN 0-06-088190-9 .
- ↑ Margaret Nofziger: Natural Birth Control - A Cooperative Method . 17th edition. Irisiana, 1993, ISBN 3-88034-713-1 .
- ↑ Harri Wettstein, Christine Bourgeois: When Sex and Fertility Form Friendship - The Complete Symptothermal Method . Fondation SymptoTherm, 2012 ( online [PDF]).
- ↑ Cyclotest 2 plus - Instructions for use . UEBE Medical, 2015 ( cyclotest.de ).
- ↑ Peter Andreas Kern: Safety and acceptance of the cycle computer and the symptothermal method . Heinrich Heine University, Düsseldorf 2003 ( online ).
- ↑ M Guida, GA Tommaselli, M Pellicano, S Palomba, C. Nappi: An overview on the effectiveness of natural family planning . In: Gynecol Endocrinol . 11, No. 3, 1997, pp. 203-219. doi : 10.3109 / 09513599709152535 . PMID 9209901 .
- ^ Robert A. Hatcher: Contraceptive Technology . Ardent Media, New York 2004, ISBN 0-9664902-6-6 .
- ↑ SB Bullivant, SA Sellergren, K Stern, NA Spencer, S Jacob, JA Mennella, MK. McClintock: Women's sexual experience during the menstrual cycle: identification of the sexual phase by noninvasive measurement of luteinizing hormone. . In: J Sex Res. . 41, No. 1, 2004, pp. 82-93. PMID 15216427 .
- ↑ AJ Wilcox, DD Baird, DB Dunson, DR McConnaughey, JS Kesner, CR Weinberg: On the frequency of intercourse around ovulation: evidence for biological influences. . In: Hum Reprod. . 19, No. 7, 2004, pp. 1539-1543. PMID 15190016 .
- ↑ I Meuwissen, R Over: sexual arousal across phases of the human menstrual cycle . In: Arch Sex Behav. . 21, No. 2, 1992, pp. 101-119. PMID 1580784 .
- ^ AK Slob, CM Bax, WC Hop, DL Rowland, JJ. van der Werff ten Bosch: Sexual arousability and the menstrual cycle. . In: Psychoneuroendocrinology . 21, No. 6, 1996, pp. 545-558. PMID 8983090 .