WHO drinking solution
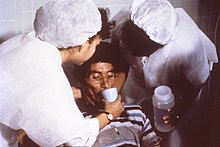
The WHO drinking solution is an aqueous solution of grape sugar ( glucose ), table salt ( sodium chloride ) and other electrolytes , which is used as a simple, inexpensive and effective treatment measure for severe diarrheal diseases such as cholera or dysentery . It is also known under the term “oral rehydration solution ” (ORL, English WHO-Oral Rehydration Solution or WHO-ORS ). The concept and composition were implemented by the World Health Organization (WHO) .
The drinking solution, which was originally developed for the treatment of cholera from 1961 , is an essential pillar of therapy when epidemic infectious diseases of the gastrointestinal tract occur , especially in countries with limited resources . If available in sufficient quantities, it can make a decisive contribution to reducing the death toll. An adult should drink about three liters of this drinking solution per day in the event of illness.
Working principle
The drinking solution takes advantage of the fact that in many diarrheal diseases the ability of the intestinal wall to absorb glucose and amino acids is retained, which occurs in the so-called co-transport with sodium in a stoichiometric ratio of 1: 2. If glucose and sodium are supplied in the same ratio, this mucosal-bound transport system is stimulated and an active transport into the body takes place with energy consumption. This is associated with a shift in the osmotic gradient , which means that water now diffuses from the intestinal lumen into the body . In addition to improving the hydration status, this also causes a thickening of the intestinal contents and thus a reduction in diarrhea.
Contraindications
If the intestine has a reduced ability to absorb glucose ( malabsorption ), the solution must not be used, as the water losses into the intestine are increased.
composition
The WHO recommends the following composition for one liter of water:
- 13.5 g glucose
- 2.9 g sodium citrate
- 2.6 g sodium chloride
- 1.5 g potassium chloride
In contrast to older formulas , the glucose concentration has been reduced somewhat. Furthermore, the use of sodium citrate instead of sodium hydrogen carbonate has been recommended since 1984 in order to increase the stability of the solution in tropical regions.
The WHO drinking solution is also available as granules in pharmacies .
history
The following research history is based essentially on the statements of JN Ruxin.
In the 1920s, the loss of water and blood salts (electrolytes) - i.e. dehydration - was recognized as the cause of the high mortality rate in cholera and an effective rehydration therapy using intravenous infusions was developed. However, this therapy proved to be practically impracticable in developing countries , as millions of sick people had no access to an effective therapy due to a lack of infrastructure . In the 1940s, Daniel Darrow of Yale University researched electrolyte losses in diarrhea and developed the physiological basis of rehydration. As a result of this research, he developed rehydration solutions that mainly contained sodium, potassium and glucose. Darrow concluded that such a solution, given orally, could help to make up for the loss of water and electrolytes and thus shorten the long infusion therapy. With this intravenous / oral combination therapy, the mortality rate of severe diarrhea in infants could be reduced to less than 5%.
In 1961 a cholera pandemic broke out in the Philippines . The head of Naval Medical Center Research Unit 2 , Captain Robert Allan Phillips (1906–1976), sent a team from Taipei to Manila . With the intravenous / oral combination therapy he developed, the mortality rate in patients treated in hospitals was reduced to 3.4%. In the course of this task, he also discovered the improved oral salt intake through a combination solution of glucose and common salt. When attempting to introduce oral rehydration therapy, however, he failed because he used solutions that were too concentrated - probably in ignorance of the research results now available on physiology - as a result of which several patients died as a result of heart failure due to overhydration (in the sense of "excessive therapeutic success").
In 1962 a group of doctors began working with students in Dhaka and Calcutta on an effective therapy for cholera-induced diarrhea . Their goal was to develop a simple solution of sugar, salt, and water to save the lives of seriously dehydrated adults, adolescents, and children. Within 6 years the physiological proof of effectiveness was provided and thus the established paradigms for the therapy of diarrhea were turned upside down. In particular, the previously valid hypothesis that “poisoning” of the sodium-potassium pump in the cell membranes of the intestinal mucosa was the cause of the high electrolyte losses was refuted. Glucose has been shown to improve the uptake of sodium by cells.
In 1966, Norbert Hirschhorn conducted a clinical study with eight cholera patients who were not given the improved solution orally, but rather through a gastrointestinal tube.
In 1968, Nalin and co-workers published a study on oral rehydration alone in the Lancet , but initially only recommended this type of treatment for mild and moderate cases. At the end of 1968 Nalin and Cash successfully carried out the first large field test in Matlab (East Pakistan) under the real conditions of a developing country and proved the efficiency of ORT ("Oral Rehydratation Therapy") in terms of both lethality and practicability under adverse infrastructural conditions.
In 1971, the efficiency was demonstrated in the context of the Bangladesh war under the most adverse circumstances; Here family members administered the drinking solution, while in Matlab only trained medical staff were used. It was recognized that the patients, especially the children, could independently adjust the amount of drink they needed to meet their needs. From the early 1970s, UNICEF and WHO produced huge quantities of ORS parcels and distributed them in all endemic areas . ORT has been shown to be effective in most other forms of diarrhea, and oral rehydration therapy has found its place in the treatment of diarrhea in First World countries .
Since then, the use of ORS has saved the lives of millions of people every year who do not have access to modern medical infrastructure. In 2006 the proportion of fatal outcomes of all cholera cases reported to the WHO was 2.6%.
Classification
The ATC code for electrolytes for oral rehydration is A07CA.
Web links
- Preparation instructions for oral rehydration salts from the WHO (PDF; 2.3 MB, English)
- Infection prophylaxis when traveling long-distance. AWMF recommendation
Individual evidence
- ↑ Freely translated and summarized from: Joshua Nalibow Ruxin: Magical Bullett: The History of Oral Rehydratation Therapy . In: Medical History , 1994, 38, pp. 363-397. PMID 7808099
- ↑ Hirschhorn et al .: Decrease in net stool output in cholera during intestinal perfusion with glucose-containing solutions . In: N Engl J Med. , 1968, 279 (4), pp. 176-181, PMID 4968807
- ↑ Nalin et al .: Oral maintenance therapy for cholera in adults . In: Lancet , 1968, 2 (7564), pp. 370-373. PMID 4173788
- ↑ WHO Cholera annual report 2006 . (PDF; 1.37 MB) WHO
- ↑ Official version of the ATC index with DDD information for Germany in 2011. (PDF; 1.3 MB) published by the German Institute for Medical Documentation and Information

