Lung function
As lung function (formerly known as respiratory functions called) is the physiological ability of the lungs as an organ for gas exchange with the external respiration of lung-breathing snails , amphibians , reptiles , birds and mammals , including humans , respectively. In everyday medical practice, the term lung function (abbreviation Lufu ) has also become (short for lung function test ) as a collective and generic term for the various examination methods of lung volumes (see also measured variables ) and other parameters of lung function, for example spirometry ("small lung function ") And body plethysmography (" great lung function ").
Physiological lung function
The physiological function of the lungs consists of so-called gas exchange, the absorption of oxygen into the body and the release of carbon dioxide from the body. The lungs thus also play an important role in regulating the acid-base balance .
Investigation procedure
The usual examination procedures known as lung function deal less with gas exchange than with the structure of the bronchial system . The most common disorders are found in this system of the lungs. Bronchial asthma and chronic obstructive pulmonary disease primarily affect the bronchi. The blood gases are only checked in special cases , for example in patients who are ventilated with apparatus. Diffusion measurements are also rare.
Spirometry
The most commonly performed lung function measurement is spirometry. A flow sensor is used to measure the airflow while breathing. In addition to breathing at rest, maximum exhalation and inhalation is required in spirometry. Since this constant flow is measured, can be in addition to the flow values such as peak flow (Engl. Peak expiratory flow, PEF) and different expiratory flow strengths (eg mid expiratory flow, MEF) and lung volumes as vital capacity (VC), expiratory reserve volume (ERV ) and resting breath volume (VT, also TV from English Tidal Volume ). A very popular measured variable is the one-second capacity (FEV 1 ). FEV 1 is of great importance as a progression parameter, particularly in the case of chronic lung diseases . The measurement of one-second capacity in relation to vital capacity is also known as the Tiffeneau index .
In contrast, measured values for inhalation are of secondary importance.
In addition to the measured values, the spirometry is also displayed graphically. The most common representation is the flow-volume curve. The flow of the respiratory flow (y-axis) is not plotted against time, but against the exhaled volume (x-axis). With this representation, pathological changes can be seen particularly easily. The graph is also essential in order to evaluate the participation of the test person in the measurement.
Here is also the main disadvantage of spirometry. The measurement is strongly dependent on the optimal cooperation. If people do not want to work (retirement applications) or are able to (small children), spirometry cannot be performed. However, it can usually be seen from the graph whether the measured values are only bad due to a lack of cooperation.
Whole body plethysmography / body plethysmography
Another method of lung function measurement is body plethysmography with the measurement of airway resistance. The problem with measuring the resistance of the entire airways is to determine the air pressure in the alveoli that triggers the measured air flow through the bronchi. The higher this pressure built up in the alveoli has to be in order to generate a certain flow, the more you have to exert yourself to breathe and the higher the airway resistance.
The body plethysmograph is designed as a cabin with a (largely) closed air volume, it looks like a small telephone booth. The measurement effort is therefore significantly higher. With this closed volume of air, one can determine an expansion or compression of the chest. The pressure sensor determines the change in air pressure in the cabin, which is inversely proportional to the change in air pressure in the chest and thus in the alveoli. The proportionality factor depends on the lung volume.
The determination of the specific resistance is less work-dependent than spirometry, since the test person only has to breathe calmly into the mouthpiece.
To determine the lung volume, breathing is interrupted at the mouth with a closure. The subject breathes in against the closure and mouth pressure and thoracic movement are registered. The current lung volume is determined from the ratio of the thoracic displacement volume and the mouth / lung pressure multiplied by the ambient pressure using Boyle-Mariott 's law. Thus the determination of further measured variables is possible, for example, the maximum volume of air in the lungs (Total Lung Capacity TLC, total lung capacity ) and the non ausatembare residual volume of the lungs ( residual volume RV). For these values it is necessary to carry out a spirometry during the measurement. This is usually done as well.
Other methods
There are two other ways to determine the airway resistance, the oscillometry (now implemented as pulse oscillometry ) and the shutter method. Pulse oscillometry can determine resistance with puffs of air into the lungs. The shutter method relies on the fact that if the airways are briefly closed, the pressure from the alveoli to the oral cavity is equalized, which, however, works increasingly poorly with pathologically altered airways.
Neither of these alternative methods can determine the lung volume and hence the TLC and RV.
Bronchospasmolysis test
Bronchospasmolysis tests the reversibility of the bronchial obstruction. To this end, it is investigated whether a reduction in the airway resistance (Rtot) can be achieved in the patient by using respiratory sprays. This goes hand in hand with an increase in FEV1. Typically, the obstruction in bronchial asthma is reversible, while the obstruction in chronic obstructive bronchitis is never completely reversible.
In the case of a reversible obstruction, the bronchospasmolysis test also reduces the residual volume, which is primarily measurable by body plethysmography ; the difference is called the volume pulmonum auctum .
Blood gas analysis
Readings
Vital capacity
Unit: liter (l). The maximum volume that can be exhaled after maximum inspiration (maximum volume that can be ventilated at will) tidal volume (AZV) + inspiratory reserve volume (IRV) + expiratory reserve volume (ERV).
The vital capacity (VC) thus represents a measure of the expansion capacity of the lungs and thorax. It is by no means a "vital" variable, as one might infer from the name, because even with extreme demands on breathing, the possible depth of breath is increased never fully exploited. It is hardly possible to state a “normal value” for vital capacity, as this depends on various parameters such as age, gender, body size, body position and level of training. The vital capacity for a younger, 180 cm tall man is about 5 liters and decreases with age.
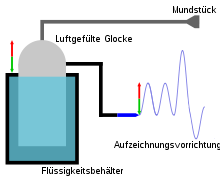
The measurement is usually carried out with a spirometer , a device that can record various volumes of gas at constant pressure. A cylindrical bell is immersed in a water container, which seals the interior of the spirometer airtight from the exterior. A large-lumen hose connects the test subject's mouthpiece with the spirometer. The change in volume during maximum exhalation after previous maximum inhalation, which leads to a corresponding bell movement, can be read on a calibrated scale. Today a spirometer is usually equipped with a flow sensor and the derived volumes are determined electronically.
One second capacity
The one-second capacity (SK) is the volume that can be exhaled forcibly within one second from the maximum inspiratory position. Measuring SK is a simple method of detecting obstructive pulmonary dysfunction.
A distinction is made between the absolute and the relative SK. The absolute SK (Forced Expiratory Volume in 1 Second: FEV 1 ) is given in volume units. The individual measured values are related to target value standard tables of the European Coal and Steel Community , depending on age, gender, height and weight .
The relative SK (FEV 1 % VC), also known as the Tiffeneau index, is given as a percentage of the vital capacity measured during inspiration (FEV 1 % IVC) or, in Germany, mostly as a percentage of the vital capacity measured during forced expiration (FEV 1 % FVC). The relative SK may only be used to describe an obstruction as long as the VC is within the normal range. If the VC is also limited in severe obstruction due to the increased work of breathing, the relative SK is calculated incorrectly normal. In such cases, the absolute SK must be used for assessment.
The disadvantage of the SK measurement is the dependence on patient cooperation.
The recording of the current strength or the respiratory flow against the volume offers further measurement parameters, for example the peak expiratory flow or peak flow (PEF)
Maximum Expiratory Flow (MEF)
MEF25 / 50/75 (unit l / s): Expiratory flow at 25/50/75% of the forced VC: Maximum expiratory respiratory flow strength at 25/50/75% vital capacity in the thorax, i.e. That is, when 75/50/25% of the vital capacity has already been exhaled.
Airway resistance (resistance)
The resistance (raw) (unit kPa × s × l −1 , measured by a pressure difference per volume flow) is a dynamic measure of the flow resistance (consisting of the viscous deformation resistance of the lung and chest wall as well as the actual airway resistance) in the airways at a defined Breathing. Airway resistance is a sensitive parameter for central airway obstruction. A decrease in resistance in the bronchospasmolysis test indicates a reversibility of the obstruction that can be influenced by drugs.
Severity: Raw ≤ 0.35 kPas / l: none; Raw 0.36-0.60 kPas / l: light; Raw 0.61 - 0.90 kPas / l: medium weight; Raw> 0.90 kPas / l: severe obstruction
Specific airway resistance
The specific airway resistance (sRaw) is a measured variable . It is defined by creating a tangent on the recorded breathing loop. The specific airway resistance contains both resistive and volume fractions without being able to differentiate them. The volume-related resistance can only be determined by determining the ITGV (FRC pleth) and the quotient formation sRAW / ITGV + VT / 2 = RAW. The equation below is mathematically correct, but physiologically incorrect! (sR) Raw / TGV kPa × s (specific resistance)
Lung volume
A distinction is made between different lung volumes (breathing volumes):
Static tidal volumes
Static tidal volumes include (composite volumes are called capacities):
- Tidal volume (AZV), also tidal volume, describes the volume that is inhaled during normal inhalation (approx. 0.5 l)
- Inspiratory reserve volume (IRV), describes the volume that can be additionally inhaled after normal inspiration
- Expiratory reserve volume (ERV), describes the volume that can still be exhaled after normal expiration
- Residual volume (RV) describes the volume that remains in the lungs after maximum expiration (cannot be exhaled). Spirometrically not detectable.
- Inspiratory capacity (IC), made up of tidal volume and inspiratory reserve volume, describes the amount of air that can be inhaled after normal expiration.
- Inspiratory vital capacity (IVC), made up of tidal volume, inspiratory reserve volume and expiratory reserve volume, describes the maximum amount of air that can be inhaled after maximum (forced) expiration, i.e. the maximum expansion capacity of the lungs.
- Total lung capacity (TLC), describes the volume that is in the lungs after maximum inspiration. Consists of vital capacity and residual volume.
- Functional residual capacity (FRC), made up of expiratory reserve volume and residual volume, describes the amount of air that remains in the lungs after normal exhalation. The FRC is not determined using whole-body plethysmography, but rather using the "gas washout method".
- Thoracic gas volume (TGV) (Syn .: intrathoracic gas volume (ITGV)), like FRC, also describes the amount of air contained in the lungs after normal expiration, but is determined via body plethysmography and therefore also takes into account gas volumes that are not in direct contact with the tracheobronchial space standing (for example, a pneumothorax or non-ventilated sections of the lung in older patients). Therefore the TGV can deliver a greater value than the FRC; in young people with healthy lungs they are mostly identical.
Dynamic tidal volumes
The dynamic tidal volumes indicate the shift in the static tidal volumes per unit of time, including:
- Respiratory limit value, also MVV, from English: maximal voluntary ventilation: maximum achievable respiratory time volume
- FVC , and FEV 1 , of Engl .: second forced expiratory volume in 1
Disruptions
Ventilation disorders
Ventilation disorders of the lungs are either ventilation disorders or an obstruction of the gas exchange. A distinction is made between obstructive and restrictive ventilation disorders, for example those caused by obesity .
Obstructive ventilation disorder
In obstructive pulmonary dysfunction , the airway resistance is increased. This can be caused by secretions or foreign bodies in the airways - bronchi (for example in the case of chronic bronchitis), by constricting pressure from outside (for example tumor or edema), by emphysema (overinflation of the lungs) or narrowing of the bronchi, e.g. B. bronchial asthma or spastic bronchitis.
The obstructive pulmonary dysfunction is shown in the Tiffeneau test by forced expiration, whereby the forced expiratory volume per second (FEV1) is reduced, but the forced vital capacity (FVC) remains the same. An increased residual volume and a reduced vital capacity can also be diagnosed in the case of long-term obstruction.
Diseases that cause obstructive ventilation disorders are asthma , chronic bronchitis or COPD , foreign body aspiration .
Restrictive ventilation disorder
In restrictive pulmonary dysfunction , the vital capacity and the total lung capacity are reduced. This is caused by restricted compliance of the respiratory system (the ability to stretch is restricted). The occurrence of a restrictive pulmonary dysfunction can for example be due to adhesions of the pleura, pulmonary fibrosis, loss of lung tissue or thorax mobility ( e.g. scoliosis , funnel chest ).
Perfusion and diffusion disorders
Pulmonary perfusion is the blood flow to the pulmonary capillaries, adapted to the ventilation. In the zone model according to John B. West , both lung ventilation and lung perfusion increase from top (apical) to bottom (basal) in healthy people according to gravity , with the ventilation-perfusion ratio decreasing in the same direction and the optimal value (alveolar ventilation: capillary Perfusion = 0.8) is in the middle.
Diffusion is a passive transport process, particles migrate from the place of higher concentration to the place of lower concentration.
Gas exchange in the lungs: O 2 from the air in the alveoli passes through the membrane into the capillaries, CO 2 from the pulmonary capillary blood into the alveoli.
Perfusion disorders:
With vascular occlusions, perfusion is limited in relation to ventilation. There is an imbalance between blood flow and ventilation of lung sections. Examples of such disturbed regional ventilation-perfusion conditions are pulmonary embolism, pulmonary fibrosis (thickening of the alveolar membrane) and pulmonary emphysema (pulmonary overinflation). With limited or no perfusion, the dead space is increased (the space that is not involved in gas exchange).
Diffusion disorders:
Are gas exchange disorders that lead to lung dysfunction. This can be: longer path of the exchange of O 2 / CO 2 in pulmonary fibrosis due to thickening of the alveolar membrane or in pulmonary edema due to fluid retention. Loss of alveoli: The exchange area is reduced in pneumonia and pulmonary emphysema. Shortened contact time: with lung resection.
literature
- Peter Lotz: Anatomy and Physiology of the Respiratory Tract. In: J. Kilian, H. Benzer, Friedrich Wilhelm Ahnefeld (Ed.): Basic principles of ventilation. Springer, Berlin a. a. 1991, ISBN 3-540-53078-9 , 2nd, unchanged edition, ibid 1994, ISBN 3-540-57904-4 , pp. 3–45.
- Hilmar Burchardi: Etiology and pathophysiology of acute respiratory failure (ARI). In: J. Kilian, H. Benzer, FW Ahnefeld (ed.): Basic principles of ventilation. Springer, Berlin a. a. 1991, ISBN 3-540-53078-9 , 2nd, unchanged edition, ibid 1994, ISBN 3-540-57904-4 , pp. 47-91; here: pp. 53–66.
- Thomas Pasch, S. Krayer, HR Brunner: Definition and measurands of acute respiratory insufficiency: ventilation, gas exchange, breathing mechanics. In: J. Kilian, H. Benzer, FW Ahnefeld (ed.): Basic principles of ventilation. Springer, Berlin a. a. 1991, ISBN 3-540-53078-9 , 2nd, unchanged edition, ibid 1994, ISBN 3-540-57904-4 , pp. 95-108.
- Joachim Frey : Diseases of the respiratory organs. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition ibid. 1961, pp. 599-746, here: pp. 626-631 ( tests of the respiratory functions ).
Web links
Individual evidence
- ↑ O. Wolfgang: Breathing - Respiratory Aid : Breathing Physiology and Ventilation Technology. 9th, revised edition. Georg Thieme Verlag, Stuttgart 2012.