Scoliosis
| Classification according to ICD-10 | |
|---|---|
| M41 | Scoliosis
Incl.:
Excl .:
|
| M41.0 | idiopathic scoliosis in the child |
| M41.1 | Idiopathic scoliosis in adolescents
Adolescent scoliosis |
| M41.2 | Other idiopathic scoliosis |
| M41.3 | Chest-related scoliosis |
| M41.4 | Neuromyopathic Scoliosis
Scoliosis after cerebral palsy, Friedreich's ataxia, poliomyelitis and other neuromuscular diseases. |
| M41.5 | Other secondary scoliosis |
| M41.8 | Other forms of scoliosis |
| M41.9 | Scoliosis, unspecified |
| ICD-10 online (WHO version 2019) | |
A scoliosis ( ancient Greek σκολίωσις scoliosis , German , curvature ' ) is a lateral deviation of the spine from the longitudinal axis of rotation (twisting) of the vortex around the longitudinal axis, and torsion of the vertebrae - accompanied by structural deformation of the vertebral bodies. This can no longer be straightened up by using the muscles . The spine usually forms several arches running in opposite directions that compensate for each other in order to maintain body balance (S-shape). The Cobb angle (after John Robert Cobb ) is used as a measure for assessing scoliosis.
In connection with kyphosis or hyperkyphosis, one speaks of kyphoscoliosis , the strongest change in the normal shape of the chest.
Scoliosis can occur in any vertebrate animal, including fish . Scoliosis in humans was first described and treated in ancient times by the Greek doctor Hippocrates .
Classification
Scolioses are classified according to their cause and time of origin, according to the position of their curvatures and the curvature pattern, according to their extent (angles of curvature and degrees of rotation) and the orientation of the curvatures (left, right). Scolioses whose cause is unknown are called idiopathic scolioses. If the cause is clarified, it is symptomatic or secondary scoliosis.
Scoliosis is one of the growth deformities. It arises and worsens during adolescence at times of increased body growth, such as the adolescent growth spurts .
Idiopathic scoliosis
In about 90% of all cases, the cause of scoliosis is unknown. There are three types of idiopathic scoliosis based on the age at which it occurred:
- Infantile idiopathic scoliosis (IIS): Develops up to the age of 3
- Juvenile idiopathic scoliosis (JIS): Develops between the ages of 4 and 10
- Idiopathic adolescent scoliosis (AIS): Develops from the age of 11
Idiopathic scoliosis has nothing to do with so-called “infant scoliosis”, a mostly short-term posture deviation in the first year of life.
Symptomatic scoliosis (secondary scoliosis)
The remaining 10% of scolioses are spread over the following causes:
- Malformation scoliosis ( congenital scoliosis) due to congenital vertebral malformations , Klippel-Feil syndrome , spina bifida , in skeletal dysplasia with exclusive involvement of the spine ( brachyolmia ), etc.
- Neuropathic scoliosis caused by nerve and muscle diseases , such as cerebral palsy , spinal muscular atrophies or poliomyelitis
- Myopathic scoliosis due to muscular dystrophy or arthrogryposis
- Scoliosis due to systemic diseases such as neurofibromatosis , skeletal dysplasia , osteogenesis imperfecta
- Iatrogenic scoliosis , i.e. scoliosis due to medical treatment measures (e.g. radiation or after surgery due to scarring)
- Post-traumatic scoliosis after violence, amputations or tumor operations in the spine.
- Static scoliosis due to differences in leg length
Classification according to the appearance
According to Lawrence Lenke, the main curvatures (the largest curvatures with structural fixation; also called primary curvatures) are named after the height of their apex (the center of the curvature):
- High thoracic: vertex of curvature between the Th2 and Th6 vertebrae
- Thoracic :vertex ofcurvature between Th6 and the intervertebral disc Th11 / 12
- Thoracolumbar: vertex of curvature between Th12 and L1
- Lumbar : vertex of curvature between the intervertebral disc L1 / 2 and L4
According to the curvature pattern, one differentiates the following scolioses:
- C-shaped scolioses: type I and V joints
- S-shaped scolioses: Lenke type II and III
- Double S scolioses (triple scolioses): Lenke type IV and VI
Etiopathogenesis (cause)
The cause of idiopathic scoliosis is - according to the meaning of its name ( idiopathic = arising spontaneously, without a known cause) - as unexplained. A coincidence of several triggering factors seems likely (multi-causal). If the cause is known, one speaks of symptomatic or secondary scoliosis.
Idiopathic scolioses arise and intensify during adolescence in times of strong body length growth , especially during pubertal growth spurts . The faster the body grows, the faster the curvature increases. Accordingly, scolioses also count among the growth deformities .
A multitude of possible causes of idiopathic scoliosis are discussed, including hormone- related growth disorders that lead to longer body growth and a more pronounced pubertal growth spurt, which would explain why patients with scoliosis are usually slightly taller than adolescents of the same age. In a quarter of the cases, idiopathic scoliosis also occurs more frequently in blood relatives, which indicates a genetic component. It is an autosomal - dominant inheritance (the inheritance only one defective gene for a disease sufficient) with incomplete penetrance (people who have the gene will not suffer) and variable expressivity (the same abnormality appears in different ways). Biomechanical factors, such as a flattened lateral ( sagittal ) profile of the spine (flat back, hypokyphosis ) and one-sided loads, probably also play a role. The theory on which the latter is based is based on the assumption that in adolescent coliosis there is a disproportion between the faster growth rate of the ventral (ventrally) parts of the vertebral body compared to the dorsal (rear; rearward) structures of the spine. The larger space requirement of the oversized ventral vertebral bodies leads to an erection of the spine and flattening of the natural kyphosis (development of hypokyphosis / flat back), as well as to a torsion (twisting) of the vertebrae against each other, so that a flattened lateral (sagittal) spine profile, such as The rotation (twisting) of the vertebrae can also occur before the spinal column is deflected from the center and are seen as a prognostically unfavorable sign of the development of scoliosis. Once the vertebrae have left the center line, there is one-sided loading and this leads to the progression of the deformity becoming independent and leading to wedge-shaped vertebrae at the apex of the curvature.
In neuropathic and mypathic scoliosis, a permanent muscular imbalance (muscular imbalance) is usually responsible for the development of scoliosis; in congenital (congenital) or iatrogenic (caused by medical measures) scoliosis it is caused by structural damage to the vertebral bodies or soft tissue structures. In the further course of growth, these scolioses worsen further, analogous to the worsening mechanism that also occurs in idiopathic scolioses.
Prevalence (frequency)
In several studies, a worldwide prevalence (frequency in the population) of 1.1% was found for scolioses above 10 ° Cobb . Scolioses with a severity of over 20 ° Cobb occur in 0.5% of the population. With scoliotic lateral deviations between 6 ° and 9 °, girls are affected just as often as boys, while more severe idiopathic scolioses are significantly more common in women than in men. Scoliosis with a Cobb angle between 10 and 19 ° affects girls 1.4 times more often, between 20 and 29 ° 5.4 times more often and from 30 ° 7.2 times more often than boys.
Course and disease value
Scoliotic incorrect posture with a curvature of less than 10 ° Cobb angle and minor scolioses that do not require treatment are common. However, so far there is no way of predicting which of these curvatures will advance as growth.
The progression ( progression ) of the curvature is directly proportional to the growth of the spine . Correspondingly, curvatures progress rapidly during the first 5 years of life and during the adolescent growth spurts (between 11 and 15 years). On the other hand, juvenile scolioses occurring between the ages of 5 and 10 can remain stable for a long time until puberty begins.
The prognosis depends on the so-called growth reserve (the growth still to come). The sooner scoliosis occurs, the greater the likelihood that it will deteriorate as it grows. Therefore, infantile scoliosis that occurred up to the age of 4 and juvenile scoliosis (with an appearance up to the age of 10) have a significantly poorer prognosis than adolescent colioses, which only develop in the prepubertal (prepubertal) growth spurt from the age of 11 and thus have the slightest residual growth in front of them, in which they can still deteriorate.
Unexpected and rapid progression very often occurs during the pubertal growth spurt. Within a few months, scolioses often reach an extent that makes an operation necessary. At this point, many parents and therapists misjudge scolioses that occurred before puberty and have hardly worsened over a long period of time, so that these scolioses are no longer medically monitored at the onset of puberty or insufficiently treated for the expected progression are. In the course of skeletal development over time, only 5% of juvenile scolioses are not progressive. The others increase by about 1 to 5 ° Cobb per year until they reach the age of 10, and by 5 to 10 ° Cobb per year after the age of 10, during the adolescent growth spurt. However, within six months they can increase by up to 40 ° Cobb.
Even after growth has ended, more pronounced, untreated scoliosis can deteriorate further due to degradation processes in the intervertebral disc or vertebral body area as a result of curvature-related unilateral loads. In scolioses up to 30 ° Cobb, no further deterioration is to be expected until the onset of menopause. Scolioses between 30 ° and 60 ° Cobb can also remain stable, but can progress up to a maximum of 1 ° Cobb per year. In the case of scolioses with initial degrees between 60 ° and 80 ° Cobb, however, it is to be expected that these will continue to progress even after growth has ended if they are left untreated. A deterioration of between 0.5 ° Cobb and a maximum of 1 ° Cobb per year can be expected here. Scolioses from 80 ° Cobb, on the other hand, usually only worsen slightly after growth has ended, since the lack of space in the trunk that begins with this curvature counteracts further collapse of the spine. This progression limitation only applies to scoliosis in adulthood, not to scoliosis in growing age, which can develop curvatures up to strengths of 160 ° to 180 ° Cobb.
In severe scoliosis, there is a risk of considerable limitations in vital capacity and thus an overload of the cardiopulmonary circulation as well as a cor pulmonale with limitations in quality of life and life expectancy. Restrictions of this type only begin at angles of curvature greater than 80 to 90 ° Cobb.
In particular, the development of a rib hump and lumbar bulge are often a cosmetic problem. Back pain occurs mainly in patients with lumbar and thoracolumbar scolioses as well as decompensated scolioses. Patients with thoracic scolioses usually have no or only mild pain symptoms . Paralysis is not to be expected in idiopathic scolioses; these usually only occur in congenital or other secondary scolioses.
Diagnosis
early detection
Scoliotic incorrect posture with a curvature of less than 10 ° Cobb angle and minor scolioses are common, only very few need treatment. However, there is no way to predict which scolioses will progressive . Since the majority of untreated scolioses worsen, early detection and follow-ups are of paramount importance.
The onset of scoliosis is gradual and rarely causes pain, which would make those affected seek medical advice. For this reason, an annual school medical check-up at the typical age of onset of idiopathic adolescent scoliosis between 11 and 13 years for girls and 12 and 14 years for boys would be useful for scoliosis early detection. Since preventive examinations of this kind are not part of the routine in Germany, the early detection rate of scoliosis is very low in this country. The main task of the sports teachers here would be to carry out regular scoliosis screenings and to report any malformations.
Initial diagnosis

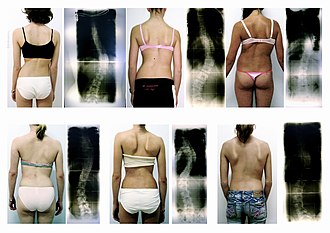
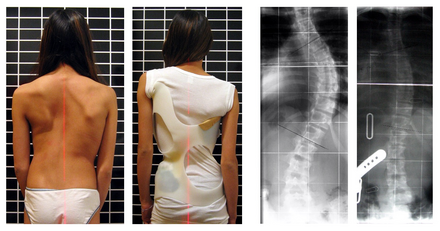
back profile standing and bent over (Adams test)
X-rays in the frontal and sagittal planes
Idiopathic scoliosis is initially just a deformity that does not cause any symptoms. Children are presented to doctors because they push the hips out to the side, because of unequal waist triangles, crooked shoulders or deviations of the upper body from the middle (vertical deviations ).
The most suitable clinical examination, which is also used in early detection of scoliosis , is the preventive test (Adams test). The patient leans forward with loosely hanging arms and straight legs (a possible leg length difference must be compensated for with a mat), a second person then looks over the back from behind and recognizes any asymmetries such as ribs and shoulder blades raised on one side (incipient rib hump ), lumbar muscles that are more pronounced on one side (the so-called lumbar bulge) and a crooked course of the spine.
Any twisting of the trunk that is noticeable through unevenness in the upper body is an indication of the onset of scoliosis and must be examined radiologically . Twists of the spine and the associated trunk sections that can be identified in this way often already correspond to a lateral curvature of up to 20 ° Cobb, for which a brace may already be indicated. A full spine view from the front ( ap; anterior-posterior ) or back ( pa: posterior-anterior ), which depicts the iliac crests in one piece and extends to the cervical spine, is also necessary to determine the likelihood of progression and to select the appropriate therapy method; also to exclude or diagnose other spinal deformities that can occur together with scoliosis (such as spondylolysis , Scheuermann's disease , congenital vertebral malformations) and to serve as a comparison image at a later point in time in order to be able to determine the extent of any progression that has taken place. Any leg length differences should be compensated for beforehand during the X-ray. Recordings lying down cannot be used.
For the initial examination, in addition to the total image of the spine in the frontal plane, an image in the sagittal (lateral) plane ( ll; latero-lateral ) should also be taken and examined. A reduced thoracic spinal column kyphosis (hypokyphosis, flat back) can then be recognized as a prognostically unfavorable sign for the further course of the scoliosis.
Using the X-ray image, the angle of the individual curvatures according to Cobb and the twisting (torsion, rotation) of the vertebrae are determined, either according to the simpler method according to Nash and Moe or the more precise method according to Raimondi. The degree of cracks is determined on the iliac crests. If other (non-idiopathic) causes of scoliosis are suspected, a magnetic resonance imaging (MRI) scan of the entire spine should be performed at an early stage .
Other important prognostic data are the age of the patient, the time of the first menstrual period in girls and the signs of maturity (development of the breasts, armpit and pubic hair).
process control
During the growing age, all scolioses should be checked by a doctor at regular intervals of 4–6 months, scoliotic malpositions up to 10 ° Cobb at least once a year. A frontal x-ray is usually sufficient for check-ups. For reasons of radiation protection, however, x-ray examinations of the spine should not take place more frequently than once a year. Since scoliosis can worsen drastically within a few months, especially during puberty , radiation-free examination methods should be used in the intervening check-ups.
These follow-up controls are usually carried out through the clinical examination and visual inspection by the doctor, or as a process documentation with photos. Bunnell's scoliometer measurement is an inexpensive measurement method that provides meaningful and numerically comparable data . Furthermore, in order to save the radiation dose, so-called “low dose” recordings can be carried out with a shortened exposure time, which are only suitable for measuring the angle of curvature.
Occasionally, computer-aided three-dimensional light-optical measurement ( video raster stereography ) of the back profile is also used, but according to an analysis by IQWiG , this is not an alternative to x-rays, as the values do not match those of x-rays well and can thus lead to incorrect treatment decisions. There is a lack of scientific evidence for their use.
In the case of severe scoliosis, the determination of body weight and vital capacity (breathing parameters) is also important. In adult patients, a significant loss of height can be an indication of progression.
Therapy of scoliosis
Depending on the severity of the scoliosis, physiotherapy (physiotherapy), corset treatment and stiffening spinal surgery are used. The various treatment methods regularly overlap. 90% of all scolioses can be treated conservatively (with physiotherapy and, if necessary, corsets) and do not require surgery.
Physiotherapy (physiotherapy)
Scoliotic malpositions up to 10 ° Cobb do not require treatment. Incipient scoliosis from 10 to 20 ° Cobb, in order further progression ( progression ) prevent, with physiotherapy treated (physiotherapy).
The objective of physiotherapeutic exercises in scoliosis treatment is the active straightening of the spine with subsequent muscular stabilization. The best known physiotherapy methods for the treatment of scoliosis in German-speaking countries are the scoliosis treatment according to Katharina Schroth and the Vojta method .
Physiotherapy according to Katharina Schroth aims at conscious posture training, which is later to be integrated more and more subconsciously into everyday life. It should lead to one-sided stressful attitudes and progression-promoting behavior to be avoided. The method must be understood and learned by the patient, which is why it is only recommended from the age of 7. It can be practiced into old age. For children between 5 and 9 years of age, a parent must be present during therapy, learn the exercises and then instruct the child in the daily exercise program at home. The scoliosis treatment according to Katharina Schroth is now also widely used in the outpatient area. The effectiveness of the method could be demonstrated by radiological follow-up controls, improvements in vital capacity (respiratory parameters) and electromyographically.
The developmental kinesiological and neurophysiological method Vojta therapy is based on reflexes (the so-called reflex locomotion), which is why no special cooperation on the part of the patient is required on the intellectual level. The method is therefore particularly suitable for infants, toddlers, mentally and learning disabled patients, as well as for patients who have problems with their body motor skills (e.g. patients with spasticity ). Because these reflexes are more pronounced in infancy and toddlerhood, the effect of the method in this age group is much greater than in later years of life. An assistant is almost always required to carry out the method.
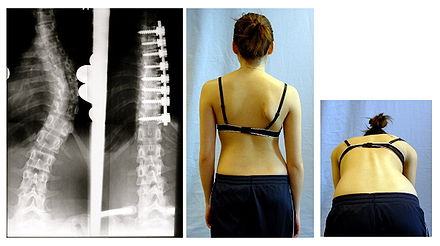
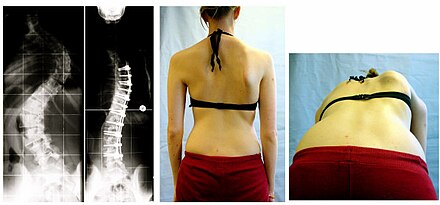
Orthosis treatment (corset therapy)
Progressive scolioses in the growing age of over 20 ° Cobb should be treated with a corset in addition to scoliosis-specific physiotherapy , which serves to guide growth. The aim of the treatment is to stop further deterioration until the end of growth, to correct existing curvatures and to maintain the corrections achieved.
In German-speaking countries, the derotation orthosis according to Chêneau ( Chêneau corset ) is most often used, which is also used today for lumbar scoliosis that used to be treated with the Boston orthosis. Only very high thoracic curvatures require the neck part of the Milwaukee corset for therapy, which is usually not necessary.
Scoliosis brace therapy must be performed by teams of physician-orthopedic technicians who have experience in scoliosis treatment. The success of the therapy depends not only on the optimal fit and adherence to the wearing times, but also on the maximum possible curvature correction. Therefore, an initial reduction in the angle of curvature in the brace (primary correction) by at least 40% should be aimed for. After two weeks of wearing, the corrective effect of the corset (the primary correction) should be checked in an initial X-ray check. In the further course of the treatment, the orthopedic technician checks every three months, which are also used to make corrections to the corset (such as reinforcing the pressure pads ). The corset should be worn more than 22 hours a day. In the case of scolioses with a corset that has a low tendency to deteriorate, shorter wearing times of at least 16 hours per day can also be considered, the advantage being seen in greater adherence to therapy , since the corset then does not have to be worn during school hours and other leisure activities. Inpatient rehabilitation measures in specialist clinics that specialize in conservative treatment of scoliosis and spinal deformities can be particularly useful for patient education, motivation and the exchange of experiences with other affected persons of the same age (all of which help improve adherence to therapy). At the end of the corset treatment (usually after growth has finished) the corset should only be worn at night for another year.
If the conditions are favorable (high-quality corsets with high primary correction and high adherence to therapy during corset wearing times), conservative therapy (i.e. corset in conjunction with physiotherapy) can almost completely straighten the spine at a young age or, if the curvature is more pronounced, prevent the threat of an operation become.
The limits of indications for corset therapy depend not only on the extent of the curvature and the age of the patient but also on the quality of the corset, in particular on the primary correction.
surgery
indication
An operation is only indicated when all conservative treatment options have been exhausted and have not produced or promise sufficient therapeutic success. In the growing age, the start of the indication for surgery depends on the deterioration tendency and the effectiveness of an alternative brace fitting and does not start below 40 ° Cobb without alternative therapy. A higher degree of disability and mortality can only be expected from a curvature of more than 80 to 90 ° Cobb. Due to these restrictions, an operative procedure is usually necessary for curvatures of this thickness even after the growth has been completed. The corrective success of surgical therapy decreases rapidly at Cobb angles above 60 ° with a simultaneous increase in surgical risk. Neuro- or myopathic scolioses are tackled surgically much earlier (from a Cobb angle of 20 °), since no conservative treatment success can be expected due to the lack of muscular stabilization options. During the growing age, surgical corrections are possible with the VEPTR procedure.
Basic principle
The basic principles of all scoliosis operations are identical: the curvature is straightened as much as possible, the rotation is eliminated, the result of the correction is held with implants and the spine is fixed in place.
techniques
There are two different approaches to operating on scoliosis: the posterior approach and the anterior approach.
Anterior derotation spondylodesis
The anterior approach surgery is performed along the ribs over the side. A rib is removed, which is later introduced into the intervertebral spaces as a separate bone material (" autologous transplant ") to bridge the gap. After opening the chest cavity and / or the abdominal cavity , the spine is exposed in such a way that the surgeon has free access to the vertebral bodies and intervertebral discs . For correction, the intervertebral discs are removed from the selected area and screws are inserted into the vertebral bodies to be corrected from the side. These screws are connected to a rod and, after correction, attached to this rod. The prepared body's own bone material takes the place of the removed intervertebral discs. Modern surgical procedures use two rods for better initial stability, if the body size allows this. This operation has the disadvantage that the abdominal or chest cavity has to be opened. In some cases, however, you cannot do without a corset treatment.
Dorsal scoliosis erection
In the posterior approach, the incision is made in the midline over the spinous processes of the spine. Various rod systems are used in this operation, which are attached to the vertebral arches with hooks and / or transpedicular screws. These bars are provided with cross connections for better stabilization. Immediately after the operation, mobility in the bridged spinal area is no longer possible. This promotes the later bony strength. The development of the "Spanstraße" is decisive for the lasting success of the operation. The necessary corticospongious crumbs are taken from the posterior iliac crests.
Ventrodorsal surgery
In severe cases, dorsal and ventral access can be used in combination (one or two stages ). This is occasionally necessary, especially in the case of special malformations or neuropathic forms of scoliosis.
Results
The cosmetic and functional result is usually better with the anterior approach. In contrast, the dorsal approach offers the advantage of safe, immediate, corset-free follow-up treatment. However, without additional correction of the back hump, the results are rather unfavorable from a cosmetic point of view.
Risks and Complications
In German-speaking countries, scoliosis operations are almost exclusively performed in specially designated scoliosis centers. Due to the high degree of specialization, the risk of complications is described as rather low and is less than 5%. Special complications of scoliosis operations are:
- Metal breaks with loss of correction
- Pseudarthroses , i.e. lack of the desired stiffening
- Infections with the need to remove the implant
- very rarely injuries to the spinal cord with partial or complete paraplegia
- renewed complaints as a result of changed spinal mobility after straightening operations, see p. Flat back deformity
- Crankshaft phenomenon ( English crankshaft , the crankshaft ' ), in which there may be the further growth below the fixed vertebral sections to a progressive postoperative deformity in all three levels - the more, the more growth potency is still present.
"Operation without stiffening"
A more recent concept is the "dynamic" scoliosis correction. This is a non-rigid surgical method. Randal Betz, who introduced the method in 2011 at the Shriners Hospital for Children in Philadelphia, USA under the name Vertebral Body Tethering , is considered to be the pioneer of this technique . The basic idea of this surgical technique is a growth control with the help of a rod-rope construct, which, however, unlike stiffening operations, allows the spine to grow further in length. In June 2017, the technique was carried out for the first time in Germany under the heading of "dynamic scoliosis correction". Since only a few operations have been performed and this has only been the case for a few years, information on complications and, above all, long-term results are still pending, so this procedure has not yet been established.
Also “dynamic” are older methods that are used particularly in childhood and neuromuscular scoliosis, such as the Luque method, first described in 1975 , in which two long L-shaped rods are attached sublaminarly to the vertebral arches with wires and the wires with the further growth can slide along the bars and thus also allow controlled growth.
Pregnancy and scoliosis
As a rule, pregnancy will not affect the curvature of the scoliosis.
A Swedish study, however, shows that patients with multiple pregnancies before the age of 23 are more likely to experience an increase in curvature. However, more recent and controlled research from Sweden suggests that a woman should not make scoliosis the basis of her life planning.
With a pregnancy from the third decade of life, there are practically no symptoms or increased curvature to fear that go beyond the normal range. Curvatures below 30 ° after growth has ended (double-arched even up to 40 °) can generally be regarded as stable even without treatment after growth has ended. From an obstetrical point of view, no lasting effects of scoliosis on pregnancy or the labor process are known. However, this does not always apply to operated patients. Due to the considerable stiffening of the spine up to the sacrum , the responsiveness of the pelvic ring can possibly be impaired.
See also
literature
- H.-P. Sharp: orthopedics and trauma surgery . Ed .: A. Rüter. Urban & Fischer in Elsevier, Munich / Jena 2009, ISBN 978-3-437-24400-1 , p. 599-605 .
- F. Niethard, UG Stauffer: Pediatrics and Adolescent Medicine . Ed .: B. Koletzko. 13th edition. Springer, Berlin 2007, ISBN 978-3-540-48632-9 , Chapter 16.3.3 Scoliosis.
- H.-P. Bischof, J. Heisel, H. Locher (Ed.): Practice of conservative orthopedics . 1st edition. Georg Thieme, Stuttgart 2007, ISBN 978-3-13-142461-7 .
- Per Trobisch, et al .: Idiopathic Scoliosis . In: Dtsch Arztebl Int . tape 107 , no. 49 , 2010, p. 875-884 ( aerzteblatt.de ).
Web links
- EuroSpine - Idiopathic Scoliosis
- Guideline: Idiopathic Scoliosis in Growing Age , as of October 1, 2009 (currently being revised)
Individual evidence
- ^ Klaus Holldack, Klaus Gahl: Auscultation and percussion. Inspection and palpation. Thieme, Stuttgart 1955; 10th, revised edition, ibid 1986, ISBN 3-13-352410-0 , p. 56.
- ^ J. Harms: Classifications (King, Lenke). Archived from the original on February 25, 2008 ; Retrieved March 20, 2010 .
- ↑ Lawrence G. Lenke, Randal R. Betz, Jürgen Harms, Keith H. Bridwell, David H. Clements, Thomas G. Lowe, Kathy Blanke: Adolescent Idiopathic Scoliosis. A New Classification to Determine Extent of Spinal Arthrodesis . In: The Journal of Bone and Joint Surgery . tape 83 , no. 8 , August 2001, ISSN 0021-9355 , p. 1169-1181 (English, lww.com ).
- ↑ a b C. J. Wirth, L. Zichner, J. Krämer: Orthopädie und Orthopädische Chirurgie. Spine and thorax . 1st edition. Thieme, Stuttgart 2004, ISBN 978-3-13-126191-5 , p. 166 ff .
- ^ P. Edelmann: Differential Diagnosis Pediatrics . Ed .: D. Michalk, E. Schönau, I. Fritz. 2nd Edition. Urban & Fischer in Elsevier, Munich 2004, ISBN 978-3-437-22530-7 , pp. 602-606 .
- ↑ a b H.-P. Bischof, J. Heisel, H. Locher (Ed.): Practice of conservative orthopedics . 1st edition. Georg Thieme, Stuttgart 2007, ISBN 978-3-13-142461-7 , pp. 425 .
- ↑ J. Specht, M. Schmitt, J. Pfeil: Technical Orthopedics . Orthotics and shoe adjustments. 1st edition. Springer, Berlin 2007, ISBN 978-3-540-29892-2 , Chapter 1.4.11 "Introduction to scoliosis orthoses", p. 52 ( limited preview in Google Book search).
- ↑ SL Weinstein, IV Ponseti: Curve progression in idiopathic scoliosis. In: J Bone Joint Surg Am . Vol. 65, No. 4, Apr 1983, pp. 447-455.
- ↑ a b S. L. Weinstein, LA Dolan, KF Spratt, KK Peterson, Spoonamore MJ, Ponseti IV. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study . JAMA 2003; 289-5: 559-567.
- ^ F. Niethard, UG Stauffer: Pediatrics and Adolescent Medicine . Ed .: B. Koletzko. 13th edition. Springer, Berlin 2007, ISBN 978-3-540-48632-9 , Chapter 16.3.3 Scoliosis.
- ^ A b Klaus Buckup : Pediatric Orthopedics . 2nd Edition. Georg Thieme, Stuttgart 2001, ISBN 978-3-13-697602-9 , p. 62-69 .
- ^ P. Edelmann: Differential Diagnosis Pediatrics . Ed .: D. Michalk, E. Schönau, I. Fritz. 2nd Edition. Urban & Fischer in Elsevier, Munich 2004, ISBN 978-3-437-22530-7 , pp. 606 .
- ↑ Scoliosimetry - degrees according to COBB, rotation according to RAIMONDI. Skoliose-Info-Forum.de, archived from the original on April 18, 2008 ; Retrieved March 21, 2010 .
- ↑ Arne Hillienhof: Video raster stereography: No alternative to x-rays in scoliosis Deutsches Ärzteblatt 2019, Volume 116, Issue 49 of December 6, 2019, page A2278, link accessed on December 15, 2019 at 8:38 p.m. CEST
- ↑ M. Fleischhauer: Guide to Physiotherapy in Orthopedics and Traumatology . 2nd Edition. Urban & Fischer in Elsevier, 2006, ISBN 3-437-45211-8 , pp. 694 .
- ↑ P. Matzen (Ed.): Pediatric orthopedics . Urban & Fischer in Elsevier, Munich 2007, ISBN 978-3-437-24020-1 , Chapter 3.6.2 - Scoliosis, p. 43 .
- ^ C. Lehnert-Schroth: Three-dimensional scoliosis treatment - Respiratory-Orthopedic System Schroth . 7th edition. Urban & Fischer in Elsevier, Munich 2007, ISBN 978-3-437-44025-0 ( limited preview in Google book search).
- ↑ H.-P. Bischof, J. Heisel, H. Locher (Ed.): Practice of conservative orthopedics . 1st edition. Georg Thieme, Stuttgart 2007, ISBN 978-3-13-142461-7 , pp. 429 .
- ^ CJ Wirth, L. Zichner, J. Krämer: Orthopedics and Orthopedic Surgery. Spine and thorax . 1st edition. Thieme, Stuttgart 2004, ISBN 978-3-13-126191-5 , p. 175 .
- ↑ a b c Guideline Idiopathic Scoliosis in Growing Age ( PDF ( Memento of the original of March 21, 2016 in the Internet Archive ) Info: The archive link has been inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this note. ), As of October 1, 2009 (currently being revised)
- ↑ J. Specht, M. Schmitt, J. Pfeil: Technical Orthopedics. Orthotics and shoe adjustments . 1st edition. Springer, Berlin 2007, ISBN 978-3-540-29892-2 , Chapter 1.4.11 "Introduction to scoliosis orthoses", p. 53–55 ( limited preview in Google Book search).
- ↑ H.-P. Bischof, J. Heisel, H. Locher (Ed.): Practice of conservative orthopedics . 1st edition. Georg Thieme, Stuttgart 2007, ISBN 978-3-13-142461-7 , pp. 430-431 .
- ^ CJ Wirth, L. Zichner, J. Krämer: Orthopedics and Orthopedic Surgery. Spine and thorax . 1st edition. Thieme, Stuttgart 2004, ISBN 978-3-13-126191-5 , p. 177 .
- ^ C. Lehnert-Schroth: Three-dimensional scoliosis treatment . 7th edition. Urban & Fischer in Elsevier, Munich 2007, ISBN 978-3-437-44025-0 , p. 309 .
- ↑ F. Landauer, H. Behensky: Correction Mechanism of Scoliosis in Corset Therapy . Orthopedic technology, 6/2002.
- ↑ Home - Pediatric Spine Foundation. Retrieved November 30, 2018 (American English).
- ↑ Per Trobisch: The dynamic scoliosis correction (DSK) - a movement-preserving surgical technique for the treatment of severe scoliosis . In: Back time - the scoliosis magazine . No. 1 , 2018.
- ↑ Danielsson AJ, Nachemson AL: Childbearing, curve progression, and sexual function in women 22 years after treatment for adolescent idiopathic scoliosis: a case-control study . In: Spine . tape 26 , no. 13 , July 2001, p. 1449-56 , PMID 11458150 ( lww.com ).