Meniere's disease
| Classification according to ICD-10 | |
|---|---|
| H81.0 | Meniere's disease |
| ICD-10 online (WHO version 2019) | |
The Meniere's disease ( Meniere's disease ) is a disorder of the inner ear , characterized by attacks of vertigo ( Vertigo ), hearing loss and phantom noise ( tinnitus , "ringing in the ears"). If these three symptoms occur together, one speaks of the Menière triad . The causes of Meniere's disease are unknown. There are some treatment methods that can have a beneficial effect on the course of the disease, but some of them are controversial.
The disease usually occurs between the ages of 40 and 60 and affects women somewhat more often than men.
The name goes back to the French ear doctor Prosper Menière ( Paris , 1799–1862), who first described the symptoms in 1861 and assigned them to the inner ear (with hearing and balance organ ).
Symptoms
Occur
Menière's seizures occur in bursts and usually repeat themselves at different intervals. Several years may pass between attacks without symptoms. Few seizures have even been seen in a patient's life. Often the disease does not begin as a complete Menière triad, i. That is, either only hearing loss together with tinnitus or only dizziness are found. Only when a Menière attack occurs with the three symptoms can the diagnosis be considered certain. In addition to hearing loss (deafness), there may be a feeling of pressure and fullness in the ear ( hydrops cochleae ).
dizziness
Dizziness, sometimes with nausea or even vomiting, is typical of a Menière attack. The dizziness lasts for minutes to hours and can be so severe that the patient can no longer stand. It gets worse with movement, but is also present at rest. Patients therefore try to keep their heads completely still or to sleep for a long time immediately after an attack.
At best, slight uncertainties in balance are felt between the attacks. Very short or very long periods of dizziness speak for diseases other than Menière's disease (such as a stroke or positional dizziness ). If there is persistent dizziness between seizures with no other characteristics of Meniere's seizures, the "additional dizziness" may be psychogenic dizziness and may cause dizziness . a. can be explained by principles of classical and operant conditioning as well as stimulus generalization .
A Tumarkin otolith crisis or vestibular drop attack is a sudden fall without loss of consciousness in patients with Meniere's disease. About 5 percent of people with Meniere's disease suffer from it. The disease was first described in 1936 by Alexis Tumarkin (1900–1990).
Hearing loss and tinnitus
In the event of an attack, the hearing ability of the affected ear worsens, associated with a ringing sound (tinnitus) and sometimes a feeling of pressure or fullness in the ear. Hearing impairment and tinnitus can go away after the first attacks, with more frequent attacks the hearing loss and usually the tinnitus persist. A hearing loss may precede the frame of Meniere's disease years. Hearing loss in Menière's disease mostly affects the low frequency range. Distorted hearing ( diplakusis ) is also remarkably often complained of. The extent of the hearing impairment is not related to the severity and frequency of the seizures.
If an already existing hearing loss improves during a Menière attack, it is referred to as the (rare) Lermoyez syndrome . It has long been unclear whether this is a special form of Menière's disease or an independent disease.
At the same time as the hearing deterioration, tinnitus occurs or worsens. In Menière's disease, tinnitus is often low-frequency. The impairment caused by tinnitus in Menière's disease is often only moderately or slightly pronounced.
It is not uncommon for a feeling of pressure or fullness in the ear and an intensification of the tinnitus to occur shortly before the attack, which can herald the attack for the patient.
causes
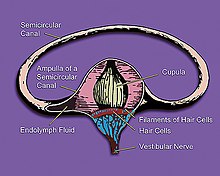
The direct cause of the disease is an endolymphatic hydrops (hydrops cochleae), in which the chambers and channels in the inner ear filled with endolymph are temporarily under increased pressure due to an increase in volume and are stretched. Since the chambers and channels of the equilibrium organ and cochlea form a connected system, the disorder affects both organs, but often to different degrees. The causes of the endolymph congestion are not clear. Some studies suggest that endolymphatic congestion can have multiple causes. Thus, not every hydrops cochleae automatically leads to Menière's disease, which develops from the first signs of dizziness and hearing impairment to full training in an average of one year. Conversely, however, every Menière's disease is associated with an endolymphatic disorder.
The mechanisms by which hydrops lead to the symptoms of Meniere's disease are not yet fully understood. A common theory is that too much pressure on the Reissner membrane leads to temporary ruptures in the membrane or increased permeability of the endolymphatic tube. This allows the potassium-rich endolymph to mix with the sodium-rich perilymph . However, the separation of the ions is important for the electrical processes at the cell / nerve level in the inner ear, as it maintains an electrical potential difference. Mixing the two fluids results in incorrect signal transmission to the brain. This is perceived by the patient as dizziness or hearing impairment. The Reissner membrane is closed again through physiological processes and the potential difference is restored. Progressive damage to the sensory cells during these seizures can cause the affected person's hearing ability to deteriorate and, in extreme cases, lead to complete deafness . More recent research results (2009) suggest that multifactorial mechanisms are possible, e.g. B. pressure-sensitive ion channels of vestibular hair cells can cause a significant change in the transmission of stimuli.
diagnosis
Patient reports, examination options
Typically, patients report a sudden onset of dizziness (sometimes associated with nausea), ringing in the ears, and hearing loss, which can recur at irregular intervals. An important part of the diagnosis is therefore questioning the patient ( anamnesis ). The "Menière triad" is not always completely present. Especially at the beginning, the condition may only show one or two symptoms, making it difficult to assess.
For further confirmation of the diagnosis ( differential diagnoses ), examinations of the middle ear ( otitis media ), the inner ear ( sudden hearing loss , semicircular canal dehiscence ), the auditory and equilibrium nerves ( acoustic neuroma , vestibular neuritis ) and the brain (stroke, multiple sclerosis , basiliar migraine ) are carried out as well as a Balance check performed to identify conditions with similar symptoms. Other diagnostic methods include performing a SISI test , computed tomography of the temporal bone and neurological examinations.
Listening tests
- Hearing threshold audiogram : This tests the hearing ability of the ears via air and bone conduction . The bone conduction test reveals a possible disorder in the middle ear. Inner ear hearing loss for the low frequencies is often found in Menière patients.
- Discomfort threshold audiogram : This is used tocheckfor hypersensitivity ( intolerance ) to loud sounds ( hyperacusis ), which is widespread in Menière patients and usually even precedes hearing loss.
- Otoacoustic emissions : These are sound signals that the ear sends out as actively produced "echoes" after certain acoustic stimuli. They are the by-product of the active cellular sound amplification that takes place in the inner ear. By measuring it, the functionality of the outer hair cells (amplifier cells in the inner ear) can be checked.
- BERA : With BERA (Brainstem Evoked Response Audiometry) the ear is stimulated with sound impulses. Electrodes on the head measure the currents generated by the brain stem. The examination allows conclusions to be drawn as to whether the sound is transmitted via the auditory nerve without problems. If the measurement results are clear, an acoustic neuroma can be largely excluded.
- Glycerol exposure test / glycerol test (Klockhoff test): With the glycerol exposure test, an endolymphatic process in the inner ear and thus Menière's disease can be detected. In addition, the sober test person drinks a glass with the extremely sweet drink. If the substance has entered the blood via the gastric mucosa, there is a concentration gradient between blood and endolymph. In order to compensate for the concentration gradient, fluid from the endolymph diffuses into the blood. This reduces the overpressure in the inner ear. If an improvement of 10–15 dB is subsequently detectable in at least three adjacent frequencies in the tone threshold audiogram, an endolymphatic event is considered to be proven.
- Air conduction-induced (AC, air conducted) cervical and ocular vestibular evoked myogenic potentials (AC cVEMP, AC oVEMP) : With the help of the cVEMP (sacculus function test) and oVEMP (analysis of the predominant part of the utricle), statements can be made about the function of the otolith organs. Above all, the function of the sacculus is often impaired at an early stage due to its central position in the organ of equilibrium.
Imaging procedures
A magnetic resonance examination (with administration of contrast medium and T2 weighting) can be carried out to rule out an acoustic neuroma . Since 2007 in Japan for the first time the endolymphatic hydrops itself could be visualized by means of contrast-enhanced magnetic resonance imaging , this method has also been used increasingly in Europe. The first study centers in Germany are the LMU Munich Clinic and the Münster University Clinic .
treatment
Limited options
Since the causes of endolymphatic hydrops and thus Menière's disease are largely unknown, specific causal treatments are not possible. However, the effects of the disease can be partially compensated for or influenced favorably. Above all, it is possible, through an adapted lifestyle, to reduce the likelihood of seizures, sometimes to the point of completely avoiding them.
Treatment of acute cases
In acute cases, the dizziness and vomiting with z. B. Thiethylperazine or Dimenhydrinat (Vomex) treated with medication and prescribed bed rest.
The immediate cause of Meniere's disease, i.e. endolymphatic hydrops, is often treated with betahistine . However, as early as 2001 a systematic review (meta study) by the Cochrane Collaboration showed that there was insufficient data to be able to assess whether betahistine has any effect on Menière's disease at all.
The skepticism against the use of betahistine has increased further after the expansion of the endolymph-filled vessels in the inner ear in humans has been quantitatively measurable in recent years using magnetic resonance imaging (MRI). In a corresponding study of six patients, betahistine did not have any effect on any of them, and a case study of one patient over two years showed an end to the dizziness, but a deterioration in hydrops and hearing in both ears. An extensive placebo-controlled longitudinal study from 2016 confirmed the ineffectiveness of betahistine.
For severe and frequent attacks (more than two every three months), doctors sometimes recommend attempting therapy with a low-dose loop diuretic (e.g. furosemide ). Here, too, the unproven effect should be emphasized.
Circulation-promoting measures in the form of medication or with the help of the compressed air chamber are often prescribed for inner ear complaints such as sudden hearing loss or tinnitus, but they do not make any sense in a confirmed diagnosis of Menière's disease. Other highly advertised procedures such as low-level laser therapy, in which the outer ear is irradiated with a red light laser, are more than questionable, as the laser light - which is said to have a positive effect on the sensory cells in the inner ear - does not physically get there .
Operative interventions
A historical overview from 2005 of the therapy methods for Menière's disease can be found in Leif Erik Walther. Here, among other things, reference is made to the step-up therapy for Menière's disease. With very frequent dizziness an intervention on the endolymphatic sac (can endolymphatic sac ) are made. During this operation, the skull bone around the endolymphatic sac is drilled away with the aim of decompression (pressure relief). The aim of the procedure is to improve the expansion of the endolymphatic sac and thus the endolymph to be better absorbed. In addition, the endolymphatic sac can be opened to allow the endolymph to drain (e.g. via a silicone splint). A neo-saccus often forms afterwards. Although this operation can reduce the number of attacks of vertigo, the procedure is not always successful or the success is rarely permanent (around 50–60 percent of patients reported an improvement in their vertigo attacks). It has not yet been proven that these numbers are more than a placebo effect .
Another way of eliminating dizziness is to partially or completely shut down the organ of equilibrium with gentamicin . This treatment, which is evidence-based, is intended to prevent the patient from dizzying attacks that last for years. The effect of gentamicin in the inner ear has not yet been fully understood. The function of all five subsystems of the organ of equilibrium need not be impaired in every case. Failures in the organ of equilibrium and a partial loss of hearing during this treatment are accepted as they are typical of Menière's disease anyway. A one-sided loss of equilibrium can usually be compensated. This remedy is a last resort and may only be used in the case of very severe impairments and only if it is certain that the balance organ is responsible for the dizziness (and not disturbances in the brain). According to a study, intratympanic gentamicin therapy is superior to saccotomy in some respects. With the help of the cervical and ocular vestibular evoked myogenic potentials and the video head impulse test, monitoring of the receptor function is possible today as part of intratympanic gentamicin therapy, but it is also necessary.
A final treatment option is the surgical severing of the equilibrium nerve ( vestibular nerve ). Certain movements have to be relearned afterwards.
In all surgical (saccotomy, transection of the vestibular nerve) and non-surgical (gentamicin administration) interventions on the inner ear, it must be taken into account that the further course of the disease can affect both organs of balance and both organs of hearing. A hasty deactivation of one side can lead in the long term to a complete loss of the sense of balance or a severe reduction in hearing.
Seizure prevention (prophylaxis)
Ventilation of the middle ear
The systems of pressure equalization in the inner ear are coupled in a highly complex way to the ongoing fluctuations in the static pressure in the middle ear and are stimulated by them. The details of the mechanisms have recently been largely clarified physiologically and anatomically .
The pressure regulation of the middle ear has a slow main component (gas exchange with middle ear tissue) and a fast secondary component (brief opening of the ear trumpet, the Eustachian tube ). The latter usually happens automatically as needed, for example when chewing or yawning, but can also be done arbitrarily, e.g. B. when flying or diving can be brought about.
In Menière patients, the pressure regulation of the middle ear is significantly worse than normal and there has been evidence since 1988 that additional ventilation of the middle ear can prevent attacks. In 1997 there was experimental evidence that additional ventilation of the middle ear actually counteracts the development of hydrops.
The method of choice for voluntary ventilation of the middle ear is the Valsalva method . It can be carried out almost anywhere spontaneously and without aids and is best combined with subsequent pressure equalization by yawning or chewing (slight cracking per ear). The Valsalva maneuver, which should always be carried out carefully and with feeling, causes a brief increase in middle ear pressure, which then disappears again due to the pressure equalization. This achieves an optimal effect on the aforementioned pressure regulation in the inner ear.
way of life
There are several methods available for treating between attacks. These are more aimed at strengthening the person as a whole (relaxation techniques, psychotherapy, balance exercises). Any kind of sporting activity is recommended, as this can regain confidence in one's own equilibrium system after a dizzy attack and, above all, the neuronal processing of the equilibrium-related signals can reorganize itself more quickly after any permanent damage caused by seizures.
A diet rich in potassium and low in salt is recommended. The WHO generally recommends a daily intake of 3.5 grams of potassium for adults . Noise, alcohol, nicotine and stress should also be avoided.
Frequent "personality image" of the Menière patient
Since the micro-metabolism in the inner ear is highly complex and under the influence of the vegetative nervous system , stress and psychological stress are repeatedly mentioned as possible contributing or triggering factors. This coincides with the frequently observed personality image of the Menière patient, which is often characterized by a tendency towards ambition and perfectionism, i.e. the risk of putting oneself under excessive pressure. From 1527 the reformer Martin Luther showed clear symptoms of Menière's disease , as a study by the Münster doctor Harald Feldmann shows.
Spelling of the name
Prosper Menière wrote himself only with a grave accent on the second "e", as evidenced by several handwritten letters with his signature. In the literature there are often other spellings (Ménière, Menier), some of which stem from the irritating lettering on the grave chapel of the Menière family in the Montparnasse cemetery in Paris.
literature
- Olaf Michel: Menière's disease and related balance disorders . Georg-Thieme-Verlag, Stuttgart 1998, ISBN 3-13-104091-2 .
- Helmut Schaaf: Menière's disease: vertigo - hearing loss - tinnitus - a psychosomatically oriented presentation. 7th edition. Springer, Berlin 2012, ISBN 978-3-642-28215-7 .
- Ralf Bröer: Meniere's disease. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. de Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 969 f.
Web links
- Meniere's disease. In: Orphanet (Rare Disease Database).
- Menière's page of the Tinnitus League
- KIMM e. V. - Contacts and information on Menière's disease
Individual evidence
- ^ JP Harris, TH Alexander: Current-day prevalence of Ménière's syndrome. In: Audiol Neurootol. 15 (5), 2010, pp. 318-322. PMID 20173319
- ↑ Meniere (1861) Sur une forme de surdité grave dépendant d'une lésion de l'oreille internal. (On a form of severe deafness dependent on a lesion of the inner ear). In: Bulletin de l'Académie impériale de médecine. 26, p. 241.
- ↑ H. Schaaf, H. Holtmann, G. Hesse, U. Kolbe, D. Brehmer: The (reactive) psychogenic vertigo. An important component in repeated M. Menière attacks. In: ENT. 47, 1999, pp. 924-932. ( drhschaaf.de ; PDF; 295 kB).
- ↑ E. Kenala et al: Short lasting drop attack in Meniere's disease. In: OtolaryngolHead Neck Surg. 124, 2001, pp. 526-530.
- ↑ T. Mom, Y. Pavier, F. Giraudet, L. Gilain, P. Avan: Measurement of endolymphatic pressure. In: European annals of otorhinolaryngology, head and neck diseases. Volume 132, number 2, April 2015, pp. 81-84, doi: 10.1016 / j.anorl.2014.05.004 . PMID 25467202 (free full text) (review).
- ↑ R. Gürkov, I. Pyykö, J. Zou, E. Kentala: What is Meniere's disease? A contemporary re-evaluation of endolymphatic hydrops. In: Journal of neurology. Volume 263, Suppl 1, April 2016, pp. 71-81, doi: 10.1007 / s00415-015-7930-1 . PMID 27083887 , PMC 4833790 (free full text) (review).
- ^ Helmut Schaaf: Menière's disease. Springer, Heidelberg 2007, ISBN 978-3-540-36960-8 , p. 58 ff.
- ↑ T. Haasler, G. Homann, TA Duong Dinh, E. Jüngling, M. Westhofen, A. Lückhoff: Pharmacological modulation of transmitter release by inhibition of pressure-dependent potassium currents in vestibular hair cells. In: Naunyn-Schmiedeberg's archives of pharmacology. Volume 380, Number 6, December 2009, pp. 531-538, doi: 10.1007 / s00210-009-0463-3 . PMID 19830405 .
- ^ Pschyrembel: Clinical Dictionary. 257th edition. Publisher Walter de Gruyter, 1994.
- ↑ J. Sheldrake, PU Diehl, R. Schaette: Audiometric characteristics of hyperacusis patients. In: Frontiers in neurology. Volume 6, 2015, p. 105, doi: 10.3389 / fneur.2015.00105 . PMID 26029161 , PMC 4432660 (free full text).
- ^ CS Hallpike, JD Hood: Observations upon the neurological mechanism of the loudness recruitment phenomenon. In: Acta oto-laryngologica. Volume 50, Nov-Dec 1959, ISSN 0001-6489 , pp. 472-486. PMID 14399131 .
- ↑ H. Levo, E. Kentala, J. Rasku, I. Pyykkö: Aural fullness in Menière's disease. In: Audiology & neuro-otology. Volume 19, number 6, 2014, ISSN 1421-9700 , pp. 395-399, doi: 10.1159 / 000363211 . PMID 25500936 .
- ↑ Leif Erik Walther and others: Morbus Menière? How to secure the diagnosis. In: MMW update. Med. No. 5, 2011, p. 153.
- ↑ Shinji Naganawa et al: Visualization of Endolymphatic Hydrops in Patients with Menière's Disease. In: Laryngoscope. No. 117, 2007, pp. 415-420.
- ↑ Gerhard Grevers, Heinrich Iro, Rudolf Probst (ed.): Ear, Nose and Throat Medicine. 3. Edition. Georg Thieme Verlag, Stuttgart 2008, ISBN 978-3-13-152123-1 , p. 259.
- ↑ AL James, MJ Burton: Betahistine for Menière's disease or syndrome. In: The Cochrane database of systematic reviews. Number 1, 2001, ISSN 1469-493X , S. CD001873, doi: 10.1002 / 14651858.CD001873 . PMID 11279734 (Review).
- ↑ R. Gürkov, W. Flatz, D. Keeser, M. Strupp, B. Ertl-Wagner, E. Krause: Effect of standard-dose Betahistine on endolymphatic hydrops: an MRI study pilot. In: European archives of oto-rhino-laryngology: official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS): affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. Volume 270, Number 4, March 2013, ISSN 1434-4726 , pp. 1231-1235, doi: 10.1007 / s00405-012-2087-3 . PMID 22760844 .
- ↑ C. Jerin, E. Krause, B. Ertl-Wagner, R. Gürkov: Longitudinal assessment of endolymphatic hydrops with contrast-enhanced magnetic resonance imaging of the labyrinth. In: Otology & neurotology: official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. Volume 35, Number 5, June 2014, ISSN 1537-4505 , pp. 880-883, doi: 10.1097 / MAO.0000000000000393 . PMID 24770407 .
- ↑ C. Adrion, CS Fischer, J. Wagner, R. Gürkov, U. Mansmann, M. Strupp: Efficacy and safety of betahistine treatment in patients with Meniere's disease: primary results of a long term, multicentre, double blind, randomized, placebo controlled, dose defining trial (BEMED trial). In: BMJ (Clinical research ed.). Volume 352, 2016, p. H6816. PMID 26797774 , PMC 4721211 (free full text).
- ↑ M. Strupp, T. Brandt: Pharmacological advances in the treatment of neuro-otological and eye movement disorders. In: Current Opinion in Neurology 19 (1), February 2006, pp. 33-40. PMID 16415675 .
- ^ AS Thirlwall, S. Kundu: Diuretics for Meniere's disease or syndrome. In: Cochrane Database Syst Rev. 3, Jul 19, 2006, p. CD003599. PMID 16856015 .
- ↑ Leif Erik Walther: Restoring procedures for a disturbed balance. In: Laryngo-Rhino-Otology. 84, Suppl 1, 2005, pp. 70-98. doi: 10.1055 / s-2005-861144 (free full text).
- ↑ P. Bretlau, J. Thomsen, M. Tos, NJ Johnsen: Placebo effect in surgery for Meniere's disease: nine-year follow-up. In: Am J Otol. 10 (4), Jul 1989, pp. 259-261. PMID 2679115 .
- ↑ J. Paradis, A. Hu, LS Parnes: Endolymphatic sac surgery versus intratympanic gentamicin for the treatment of intractable Ménière's disease: a retrospective review with survey. In: Otology & neurotology: official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. Volume 34, Number 8, October 2013, ISSN 1537-4505 , pp. 1434-1437, doi: 10.1097 / MAO.0b013e3182908b28 . PMID 23846192 .
- ↑ Leif Erik Walther u. a .: Dynamic change of VOR and otolith Function in intratympanic gentamicin treatment for Ménière's disease: Case report and review of the literature . In: Case Rep Otolaryngol. 2013, p. 168391, doi: 10.1155 / 2013/168391 , Epub 2013 Feb 26.
- ^ HP Wit, RA Feijen, FW Albers: Cochlear aqueduct flow resistance is not constant during evoked inner ear pressure change in the guinea pig. In: Hearing research. Volume 175, Number 1-2, January 2003, ISSN 0378-5955 , pp. 190-199. PMID 12527138 .
- ↑ R. Hofman, JM Segenhout, FW Albers, HP Wit: The relationship of the round window membrane to the cochlear aqueduct shown in three-dimensional imaging. In: Hearing research. Volume 209, number 1-2, November 2005, ISSN 0378-5955 , pp. 19-23, doi: 10.1016 / j.heares.2005.06.004 . PMID 16039079 .
- ↑ M. Brattmo, B. Tideholm, B. Carlborg: Inadequate opening capacity of the eustachian tube in Meniere's disease. In: Acta oto-laryngologica. Volume 132, number 3, March 2012, ISSN 1651-2251 , pp. 255-260, doi: 10.3109 / 00016489.2011.637175 . PMID 22201512 .
- ^ P. Montandon, P. Guillemin, R. Häusler: Prevention of vertigo in Ménière's syndrome by means of transtympanic ventilation tubes. In: ORL, journal for oto-rhino-laryngology and its related specialties. Volume 50, Number 6, 1988, ISSN 0301-1569 , pp. 377-381. PMID 3231460 .
- ↑ RS Kimura, J. Hutta: Inhibition of experimentally induced endolymphatic hydrops by middle ear ventilation. In: European archives of oto-rhino-laryngology: official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS): affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. Volume 254, Number 5, 1997, ISSN 0937-4477 , pp. 213-218. PMID 9195144 .
- ↑ WJ ten Cate, LM Curtis, KE Rarey: Effects of low-sodium, high-potassium dietary intake on cochlear lateral wall Na +, K (+) - ATPase. In: European archives of oto-rhino-laryngology: official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS): affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. Volume 251, Number 1, 1994, pp. 6-11. PMID 8179870 .
- ^ Potassium Intake for Adults and Children . Recommendations WHO Guideline, 2012.
- ↑ Olaf Michel: Menière's disease and related balance disorders . Georg Thieme Verlag, Stuttgart 1998, ISBN 3-13-104091-2 , p. 139.
- ↑ Olaf Michel: Menière's disease and related balance disorders . Georg Thieme Verlag, Stuttgart 1998, ISBN 3-13-104091-2 , p. 133 f.
- ↑ Harald Feldmann: Martin Luther's seizure disorders. In: Sudhoff's archive. Volume 73, 1989, pp. 26-44.
- ↑ From the French-language Wikipedia: il n'y a pas de “é” à Menière, du moins pour Prosper, l'état civil a rajouté le “é” sur l'extrait de naissance du fils de Prosper (there is no “é "With Menière, at least with Prosper, the registry office has added the" é "to the birth certificate of Prosper's son).
- ↑ A. Rauchfuss: On the correct spelling of Prosper Menière's name and some comments on his life and work. In: Laryngol Rhinol Otol (Stuttgart). 63 (8), Aug 1984, pp. 381-385.
- ↑ Olaf Michel: Menière's disease and related balance disorders. Thieme, 1998, ISBN 3-13-104091-2 , p. 8.



