Salter osteotomy
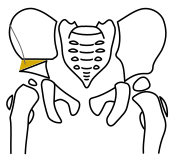
The Salter osteotomy (Innominate Osteotomy) is an orthopedic surgical technique for the mechanical improvement of the roofing of the femoral head. As a simple ( two-dimensional ) pelvic osteotomy, it belongs to the category of acetabuloplasty and is therefore one of the standard procedures in hip dysplasia therapy .
It is named after Robert Bruce Salter (1924-2010), a specialist in pediatric orthopedics in Toronto, who developed it since 1960 and used it for the first time in 1961. At that time the osteotomy was still used exclusively in connection with an open ( operative ) reduction of the femoral head. Today this is rather the rarest case.
Basics and anatomy
The hip bone is made up of three bones, the iliac bone , the pubic bone and the ischium . During growth, the growth plates between the three bones remain open. They are only connective tissue , but are later flexibly connected to one another by cartilage tissue and only ossify at the end of the bony growth. The three growth plates meet in the later center of the acetabulum and form the Y-joint there .
In hip dysplasia, the joint socket lacks the lateral (lateral) and front (ventral) roofing (also known as the socket cavity ). The head of the femur is therefore incorrect covered and threatening depending on the severity of dysplasia after slipping up and dislocate (dislocate).
The biomechanical effects of hip dysplasia affect the acetabulum, femoral head and femoral neck. The pressure from the head on the socket during exercise has sufficient transfer surface in a healthy socket, the so-called stress zone. It is precisely this area that is reduced in hip dysplasia. This leads to an increase in the loading pressure. The result of this pressure increase is hip arthrosis in untreated dysplasia . The inadequate centering of the head also leads to a steep position of the femoral neck and thus to a coxa valga , which can further promote the development of osteoarthritis.
Indications
This surgery was designed and is still used to treat childhood hip dysplasia . Today hip are sonography in screening U3 standard, and most hip dysplasia can thus be detected early. Depending on the severity of the dysplasia, conservative, i.e. non-operative, measures such as splints or plaster of paris are sufficient. Severe dysplasias with irreversible dislocation of the joint must definitely be treated surgically. Despite all the early examinations, not all dysplasias can be detected, and the later hip dysplasia is diagnosed, the sooner it must be tackled surgically.
Further indications are Perthes disease and secondary dysplastic cup changes, for example in the context of neurological diseases such as infantile cerebral palsy . The Salter technique has proven itself in Perthes disease, especially in connection with intertrochanteric osteotomy . The enlarged femoral head leads to relative dysplasia because it can no longer be grasped by the natural socket. By swiveling the pan over, the head can be rimmed and, if the therapy is applied early, it can even be shaped.
The Salter osteotomy can be performed from around 18 months of age. In any case, the duration of the conservative measures that are regularly used beforehand only very rarely allow the operation to be carried out earlier. The strength of the bone increases sharply in the course of the first year of life, which is advantageous for performing the osteotomy, so you should wait until this point. The Salter method can be used as long as the Y-joint is open and the socket fragment can therefore be pivoted. As with all cup-improving interventions in childhood, the upper limit is around 14 years.
Aim of the Salter osteotomy
The aim of the Salter osteotomy, as with other acetabuloplasties , is to improve the roofing of the femoral head. The Salter technique tries to adjust the acetabulum so that the socket, femoral head and femoral neck can grow as anatomically as possible. In Perthes disease , the objective is so-called "containment". The femoral head should be gripped, recentered and - through the growth stimulation - also shaped.
The technology
Under X-ray control, the iliac bone is divided horizontally on one side above the acetabulum, i.e. above the acetabulum. The lower fragment that has become free is now pivoted downwards and forwards, the pivot point being roughly in the area of the symphysis . The surgeon measures how far it is pivoted both in a preoperative planning and on the intraoperative x-ray. According to the resulting osteotomy gap, a bone wedge is sawn to size, which is then driven into the gap. If there is sufficient tension, the bone wedge will hold in its position by itself; if this is not the case, it can be fixed with a thin wire (so-called Kirschner wire).
After the operation, while still under anesthesia, a pelvic leg cast is put on, which is left in place for about 6 weeks.
The bone wedge
In children it is difficult to use their own bone in the sense of autologous (bone) transplantation . In the case of simultaneous intertrochanteric (between the protruding bones on the thigh bone), an attempt can be made to use the sloping correction wedge. In most cases, however, it is too small.
Today donor bones from in-house bone banks or from various manufacturers are mainly used. These are mostly femoral heads that are removed during endoprosthesis operations and donated to otherwise healthy patients who have given their consent. The donor bone are in certified thermal disinfection equipment disinfected and deproteinized. They are then in sterile containers at least minus 20 ° C cryopreserved . Alternatively, it is possible to sterilize donor bones in an autoclave under the influence of pressurized steam . Other sterilization methods , for example gamma-ray sterilization, are also used in industrial bone preparation.
All processing and disinfection / sterilization processes as well as the storage of the donor bones (deep freezing) are complex and are subject to strict requirements of the German Medical Association , the Medical Devices Act (MPG) and the Robert Koch Institute .
Complications
General complications
As with any surgery, vascular and nerve injuries can occur. However, the easy and safe access and the short duration of the operation keep blood loss to a minimum. During bone surgery there is always a risk of unexpected fractures. These must be treated directly intraoperatively.
Postoperative complications such as wound healing disorders , arthritis of the hip joint and wound infections can occur. In the worst case, the latter can lead to sepsis .
Specific complications
Intraoperative injuries to organs or larger blood vessels are not described in the literature. Injuries or irritations of the lateral femoral cutaneous nerve (sensitive inguinal-femoral nerve ) can occur, but are usually not permanent (reversible).
A postoperative failure or collapse ( sintering ) of the bone wedge can make a new operation necessary. It can also happen that the bone wedge has not been anchored firmly enough and it loosens postoperatively from the osteotomy gap, which usually leads to the dissolution ( lysis ) of the wedge. The pelvic leg plaster can cause pressure damage or nerve irritation.
Alternatives
Overall, the Salter osteotomy is a simple technique with few complications. Nevertheless, techniques that start closer to the joint and enable the reconstruction to be more precise and anatomical are on the advance. The Acetabuloplastik to Pemberton or Dega, as well as other modifications which provide good opportunities for early treatment of gelenkdeformierenden diseases of the hip in children.
history
The history of surgical therapy for cup misalignments begins at the end of the 19th century. In 1891, King King tried for the first time in Berlin to fold down a periosteal bone scale in the lateral acetabular cavity . Albee (1915) and Jones (1920) used this concept and developed from it the basic form of today's acetabuloplasty. They deposited bone chips from the shin into the osteotomy gap. In 1924, Spitzy tried a method that was unsustainable. He fixed bone chips (also from the shin) to the dysplastic edge of the socket. They should form a new pan bay as they grow.
Salter developed his surgical technique between 1958 and 1961 as a modification of the already existing techniques of simple pelvic osteotomy. He called the technique "Innominate Osteotomy" (unnamed bone cutting). The technique was revolutionary, as all other procedures up to now had osteotomized near the joint. Above all, Salter wanted to establish a procedure that was simple and as safe as possible.
The Salter technique has been used worldwide and very often with great success. Nowadays the Salter technique is being replaced more and more by newer modifications of acetabuloplasty. The basic principle, however, always remains the same.
See also
Literature and Sources
literature
- AB Imhoff, R. Baumgartner: Checklist Orthopedics . Thieme, 2006, ISBN 3-13-142281-5 .
- SJ Breusch, H. Mau, D. Sabo: Clinical Guide Orthopedics . Elsevier, 2006, ISBN 3-437-22471-9 .
- Klaus Buckup , LC Linke, W. Cordier: Pediatric Orthopedics . Thieme, 2001, ISBN 3-13-697602-9 .
- J. Duparc: Surgical Techniques in Orthopedics and Traumatology . Bd. Pelvic ring and hip. Elsevier, 2005, ISBN 3-437-22556-1 .
- F. Hefti, R. Brunner: Pediatric orthopedics in practice . Springer, 2006, ISBN 3-540-61480-X .
- R.-P. Meyer, A. Gächter: Hip surgery in practice . Springer, 2005, ISBN 3-540-22718-0 .
- Results of acetabuloplasty using the modified Dortmund technique (dissertation by Robert Bonmann 2003) (PDF file; 1.38 MB)
- CJ Wirth: Orthopedics and orthopedic surgery . Bd. Pelvis / hip. Thieme 2004, ISBN 3-13-126221-4 .
Individual evidence
- ^ RB Salter: Role of innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip in the older child. In: J Bone Joint Surg Am . 48 (7), 1966 Oct, pp. 1413-1439. PMID 5921797 .
- ^ Huang SC, Wang JH. A comparative study of nonoperative versus operative treatment of developmental dysplasia of the hip in patients of walking age. In: J Pediatr Orthop. 17 (2), 1997 Mar-Apr, pp. 181-188. PMID 9075093
- ^ SR Thomas, JH Wedge, RB Salter: Outcome at forty-five years after open reduction and innominate osteotomy for late-presenting developmental dislocation of the hip. In: J Bone Joint Surg Am. 89 (11), 2007 Nov, pp. 2341-2350. PMID 17974875
- ^ A b c d e F. Hefti, R. Brunner: Children's orthopedics in practice . Chapter Hip Dysplasia. Springer 2006.
- ^ RP Meyer, A. Gächter, U. Kappeler: Hip surgery in practice . Springer, 2005, ISBN 3-540-22718-0 .
- ↑ a b K. Buckup, LC Linke, W. Cordier: Kinderorthopädie . Thieme, 2001, ISBN 3-13-697602-9 .
- ↑ R. Suda, G. Petje: osteonecrotic diseases in pediatrics. In: Journal for Mineral Metabolism. 14 (1), 2007, pp. 27-31.
- ↑ a b Katja Linnemann: Radiological results and clinical long-term observations of Salter and Pemberton operations in patients with infantile cerebral palsy . Dissertation. Clinic and Polyclinic for Orthopedics of the Westfälische Wilhelms-Universität Münster, 2005. Online version ( Memento from March 14, 2007 in the Internet Archive ) (PDF; 831 kB)
- ↑ RB Salter: The scientific basis for innominate osteotomy in the treatment of Legg-Perthes disease. In: J. Bone Joint Surg. 55B (1973), pp. 216-221.
- ^ Robert B. Salter: Innominate osteotomy in the management of residual congenital subluxation of the hip in young adults. In: Clin Orthop Relat Res. Edition Jan-Feb (182), 1984, pp. 53-68. PMID 6692628 .
- ^ Roland Bonmann: Results of acetabuloplasty in the modified Dortmund technique . Inaugural dissertation . Justus Liebig University, Giessen 2003. Online version
- ^ Lars Niclauß: Long-term analysis of Salter's pelvic osteotomy in congenital hip dysplasia . Inaugural dissertation, Ruhr University Bochum 2002. Online version
- ↑ A. Ishida, SS Kuwajima, J. Laredo Filho, C. Milani: Salter Innominate Osteotomy in the Treatment of Severe Legg-Calve-Perthes Disease: Clinical and Radiographic Results in 32 Patients (37 Hips) at Skeletal Maturity. In: Journal of Pediatric Orthopedics. 24 (3), May 2004, pp. 257-264. PMID 15105719
- ↑ Telos Guidelines for Maintaining a Bone Bank . Online version ( Memento of the original dated December 16, 2015 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. (PDF; 101 kB)
- ↑ Steffen Schröter: Biomechanical properties of human cancellous bone after gamma sterilization versus heat disinfection with the Lobator . Dissertation . Medical Faculty of the Eberhard Karls University of Tübingen, 2005. Online version
- ^ FH Albee: The bone graft wedge. In: NY Med. 52, pp. 433-441 (In: Am J Med Sci. 149, pp. 313-325).
- ^ E. Jones: The operative treatment of irreducible paralytic dislocation of the hip. In: Amer J Orthop Surg. 18 (1920).
- ^ H. Spitzy: Artificial pan roof formation. In: Z Ortop. 43, 1924, pp. 284-294.
- ^ Robert B. Salter, JP Dubos: The first fifteen years personal experience with innominate osteotomy in the treatment of congenital disloction and subluxation of the hip. In: Clin Orthop. 98, 1974, pp. 72-103. PMID 4817246