Sporotrichosis
| Classification according to ICD-10 | |
|---|---|
| B42.9 | Sporotrichosis |
| ICD-10 online (WHO version 2019) | |
The sporotrichosis or Sporothrix mycosis (also Schenk's disease or Crohn's Schenk or Rose gardener's disease ) is a fungal disease , which the deep skin layers, the lymphatic system can be attacked or the whole body. It occurs in humans, but also in dogs, cats, horses, cattle, chimpanzees and rats and is classified as a zoonosis as a disease that can be transmitted from humans to animals and vice versa . The causative agent of the infectious disease is Sporothrixschenckii. Sporotrichosis occurs mainly in tropical and subtropical areas, more common in North America, Africa and Japan, while it is very rare in Central Europe. The disease manifests itself primarily in the formation of lumps in the subcutaneous tissue , which can break open and then secrete a greasy exudate . Iodine compounds or antimycotics are used for treatment .
Cause, spread and development of the disease
The infection occurs through direct contact with the pathogen, especially through skin wounds. Sporothrixschenckii is a ubiquitous fungus that occurs everywhere and is particularly abundant in soils with decomposing organic material ( humus , compost ) as a rot germ ( saprophyte ). Sporothrixschenckii is a dimopher fungus: At temperatures below 30 ° C it grows in mycelium form, at body temperature in yeast form.
Puncture injuries caused by contaminated splinters, by putting soil or parts of plants in wounds, and scratches and bite wounds caused by cats are more common triggers of sporotrichosis. The pathogen can also be found in the oral cavity of healthy cats. In the case of humans, employees in tree nurseries, gardeners and farmers are particularly at risk.
Direct introduction into wounds does not seem to be absolutely necessary in every case. Human contact with cat exudate may be sufficient to cause infection. In addition, infected cats also excrete large amounts of the pathogen with their faeces.
Sporotrichosis is primarily a single disease. In 1988, 84 cases of sporotrichosis occurred in the USA, which could be traced back to peat waste packaging from tree seedlings. Between 1998 and 2004 there was a strong accumulation of the disease in Rio de Janeiro , with 1503 cats, 759 people and 64 dogs being affected. In the majority of cases in humans and dogs, direct contact with cats was demonstrated.
Clinical manifestations
The shape of the skin manifests itself in skin changes, which are mostly located near skin injuries and are not painful. They are not sensitive to antibacterial treatment. This form occurs less often in humans, in such cases as "ulcerative-verrucous" lesions of the skin. In dogs, numerous nodules (occur granulomas ) in the subcutaneous tissue, the ulcerated disintegrate and a red-brownish exudate can secrete. Cats more often show boils ( abscesses ) or non-demarcated pus foci ( phlegmon ), which also disintegrate into ulcers and show no tendency to heal. Due to the strong need to clean the cat, the pathogens can be distributed further over the body and also settle beyond the original focus.
The skin-lymph form (lymphohocutaneous form) arises from the spread of the pathogen from the skin wounds via the lymph vessels and is thus a complication of the skin form. This manifestation is typical of human sporotrichosis. At the point of entry, boil- like nodules develop that can melt down, as well as "satellite lesions" that are located like chains along the draining lymphatic vessels. Lymph node swelling in the affected region is typical .
The generalized form occurs seldom and mostly only in immunocompetent patients, in humans especially patients with AIDS or after organ transplants , in cats, animals with leukemia or immunodeficiency syndrome . It is characterized by general and unspecific symptoms such as weakness and fever . The pathogen is then transferred to other organs and tissues . It is mostly spread from the affected lymph nodes.
Primary lung involvement ( lung shape ) by inhaling the conidia is possible. The prognosis in such cases is poor.
Investigation methods
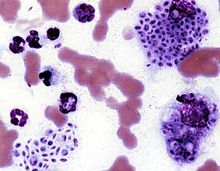
During the examination, it should be ensured that the disease is contagious, even if the granulomas have not yet opened. The diagnosis is made by microscopic examination of the exudate from the nodules. The pathogens appear as cigar-shaped or round structures about 2–10 µm in size, which can occur both within cells and freely in the exudate fluid. Secondary bacterial infections are common. Special staining methods such as PAS staining make diagnosis easier. A negative detection in a sample does not rule out the disease, especially in dogs there are usually only a few fungi in the skin nodules.
The pathogen can usually only be cultivated from samples that are surgically obtained from the depths of the nodules.
The most reliable evidence is an immunofluorescence test , which shows the possible presence of the pathogen even with a negative fungal culture.
Bacterial and other fungal diseases of the skin ( botryomycosis , nocardiosis , actinomycosis , leprosy and other mycobacteriosis ), smallpox diseases such as catpox , tumors and parasites ( demodicosis ) must be excluded from the differential diagnosis .
treatment
Treatment of man
According to the latest guidelines, the treatment of the lymphocutaneous and cutaneous forms of humans is initially recommended to be administered itraconazole daily for up to 2-4 weeks after the lesions have healed, with a treatment duration of 3-6 months being expected. If there is no response, the dose should be administered twice. Alternatively, terbinafine or saturated potassium iodide solution can be used. Fluconazole should only be used if these drugs are poorly tolerated . Local hyperthermia can be recommended for pregnant and breastfeeding women .
The treatment of sporotrichosis with bone and joint involvement takes place with itraconazole for at least 12 months. After two weeks of treatment, the serum level of the drug should be determined to ensure a sufficient serum concentration. Immediate treatment with amphotericin B , which is not tolerated by all patients, and a later switch to itraconazole are less reliable .
In the case of severe and life-threatening lung involvement , therapy is also carried out with an initial dose of amphotericin B and later switching to itraconazole, whereby the total duration of therapy should also be at least 12 months. If the lung involvement is less pronounced, itraconazole can also be administered for at least 12 months. Surgical removal of the lesion in connection with amphtericin B is recommended in localized lung involvement.
Similar guidelines apply to the generalized form . Lifelong therapy may be necessary in AIDS patients.
Treatment of animals
In animals, oral administration of saturated potassium iodide solution is also the method of choice for reasons of cost. Oral administration of antimycotics such as ketoconazole or itraconazole is also possible. Treatment with potassium iodide should be continued for 30 days after the granulomas have disappeared. However, iodine is toxic in higher doses (→ iodine intolerance ). If symptoms of poisoning occur (discharge from the nose and eyes, severe dandruff formation in the dog; vomiting, unwillingness to eat, disturbed general condition or even cardiovascular failure in the cat), the treatment must be discontinued or at least interrupted.
Literature and Sources
- Chiara Noli, Fabia Scarampella: Sporotrichosis. In: Practical Dermatology in Dogs and Cats. 2nd Edition. Schlütersche Verlagsanstalt, 2005, ISBN 3-87706-713-1 , pp. 216-217.
- DW Scott et al .: Small animal dermatology. 5th edition. WB Saunders, Philadelphia 1995, pp. 364-368.
- P. Fritsch: Dermatology and Venereology . 2., revised. Edition. Springer-Verlag, 2004, ISBN 3-540-00332-0 .
- Individual evidence
- ^ A b c Christiane Weingart et al.: Sporothrix schenkii infection in a cat. In: Small Animal Practice. 56 (2011), pp. 263-267.
- ^ FB Coles et al.: A multistate outbreak of sporotrichosis associated with sphagnum moss. In: Am. J. Epidemiol. 136: 475-487 (1992). PMID 1415167
- ↑ A. Schubach et al.: Epidemic sporotrichosis. In: Curr Opin Infect Dis . 2008, pp. 129-133. PMID 18317034
- ^ CA Kauffman et al .: Infectious Diseases Society of America. Clinical practice guidelines for the management of sporotrichosis: 2007 update by the Infectious Diseases Society of America. ( Memento of September 17, 2008 in the Internet Archive ) In: Clin Infect Dis . 45 (2007), pp. 1255-1265.
