Talimogen laherparepvec
| Overview | |
|---|---|
| Non-proprietary name | Talimogen laherparepvec |
| other names | T-Vec, T-VEC, OncoVEX GM-CSF |
| CAS number | 1187560-31-1 |
| ATC code | L01 xx51 |
| Drug class | Antineoplastic and immunomodulating agents |
| Source material |
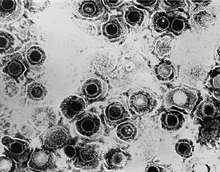
HSV-1 , strain JS1 ( Herpesviridae ) |
| characterization | JS1 / ICP34.5- / ICP47- / hGM-CSF |
| Route of administration | Intralesional |
| Trade name | Imlygic ( Amgen ) |
Talimogen laherparepvec (also: T-Vec ) is an oncolytic virus that destroys cancer cells . It is used for the gene therapy treatment of black skin cancer ( melanoma ), which has already formed daughter tumors ( metastases ).
description
Talimogen laherparepvec is a weakened herpes simplex virus type 1 (HSV-1, "cold sore virus"), the genetic material of which has been modified biotechnologically so that it can infect melanoma cells and multiply in them. The agent is injected directly into the skin lesions and leads to the destruction of the infected melanoma cells. This releases substances that are supposed to activate the immune system to fight cancer cells throughout the body.
Talimogen laherparepvec is the first authorized representative in the western world from the group of genetically engineered oncolytic viruses. It was approved as Imlygic in the USA in October 2015 and EU-wide in December 2015, and was launched in Germany in June 2016.
Talimogen laherparepvec is produced in monkey kidney cells ( Vero cells ) using recombinant DNA technology .
pharmacology
Mechanism of action
The following two mechanisms are assumed for the effect of Talimogen laherparepvec:
- Local lysis of the melanoma cells
- Systemic tumor-specific immune response .
The combination of the two active principles is known as oncolytic immunotherapy. The exact mechanism of action is unknown.
A virus strain from clinical isolation (JS1) was used as the starting material for the genetic modifications instead of a laboratory strain. Through the functional deletion of the two genes for ICP 34.5 and ICP47, the herpes simplex virus type 1 (HSV-1) was modified in such a way that it selectively infects tumor cells and multiplies in them. Unlike normal cells, tumor cells are susceptible to damage and cell death by herpes simplex virus type 1, which lack the ICP34.5 gene.
The second gene, ICP47, codes for a defense strategy in the HSV-1 wild type with which it tries to evade the host's immune defense by downregulating the formation of the antigen-presenting MHC class I protein complex on the surface of cells. The antigen presentation to cytotoxic T cells attracts killer cells , which the virus-infected cells normally eliminate. By removing the ICP47 gene, this downregulation is switched off. Furthermore, the lack of ICP47 causes an increased expression of the HSV US11 gene , which increases viral replication in tumor cells. The tumor cells are “flooded” with Talimogen laherparepvec and lyse (“burst”), releasing not only the newly formed viruses, which can attack other melanoma cells, but also tumor antigens .
The insertion of a sequence coding for human granulocyte macrophage colony stimulating factor (GM-CSF) into the HSV-1 genome causes the infected melanoma cells to produce GM-CSF. This is also released during the lysis of the melanoma cells. It is assumed that tumor antigens and GM-CSF trigger a systemic anti-tumor immune response and effector T-cell response, whereby tumor cells are recognized and destroyed in other places in the body.
Biodistribution and excretion
Talimogen laherparepvec is eliminated by the body's own general host defense mechanisms ( autophagocytosis , immune response ). Virus components are broken down by the endogenous catabolic metabolic pathways typical for proteins and DNA .
Of 30 patients examined, transient low concentrations of viral DNA (Talimogen-laherparepvec-DNA) were measured in 90% in the blood and in 20% in the urine. Virus DNA was detected in tissue samples from treated melanoma cells in 90% of the patients. The presence of viral DNA does not necessarily correlate with the risk of viral infection.
As with wild-type HSV-1 infections, talimogen laherparepvec can also have a latent accumulation of viral DNA in neurons that innervate the infected sites.
Clinical information
field of use
Imlygic is approved in the EU for the treatment of adult patients with melanoma that can not be removed surgically and already in other body areas scattered have (stage IIIB, IIIC and IVM1a), but not in bones, lungs, brain or other internal organs. Approval in the US is not limited to specific stages of melanoma.
Restrictions on use and precautions
Patients who are severely immunocompromised should not be treated with Talimogen laherparepvec. Women who could become pregnant and are to be treated with Talimogen laherparepvec should use contraceptive measures to avoid pregnancy. It is known from the HSV-1 wild type that the virus can cross the placental barrier or be transmitted to the child at birth. Wild-type HSV-1 infections have been associated with serious adverse effects if the unborn or newborn became ill with the infection. It cannot be ruled out that the infection with the modified virus has a similar effect, even if there are no clinical data on it so far. No effects on embryo-fetal development were observed in animal studies.
Accidental exposure to Talimogen laherparepvec can lead to infection with the modified herpes viruses. Contact persons of the patient such as healthcare professionals, household members, caregivers and sexual partners should avoid direct contact with treated skin areas and body fluids of the patient during the treatment period and for up to 30 days afterwards. Pregnant women, newborns and immunocompromised people must not be exposed to contaminated objects. It is not known whether Talimogen laherparepvec is excreted in breast milk.
Talimogen laherparepvec is sensitive to acyclovir . Treatment with this or other antiviral agents may make Talimogen laherparepvec less effective.
unwanted effects
The most common side effects, seen in more than a quarter of Imlygic- treated patients, were fatigue , chills, fever (pyrexia), nausea, flu-like illness and injection site pain. The vast majority of side effects were mild or moderately severe. The most common serious adverse effect ( Grade 3 or higher) was inflammation of the subcutaneous tissue ( cellulitis ), which occurred in 2.1% of the treated.
Cold sores or other herpes diseases (e.g. herpetic corneal inflammation ) may occur during treatment with Talimogen laherparepvec . Even after the end of treatment, there is a risk of symptomatic herpes infections due to reactivation of Talimogen laherparepvec or HSV-1 wild type.
Studies
The approval of Imlygic is based on data from the Phase III OPTiM study . In this open, randomized study in 436 patients, the effectiveness of Talimogen laherparepvec with advanced inoperable melanoma was compared to treatment with subcutaneous administration of GM-CSF. To enable delayed, immune-mediated anti-tumor effects, patients were treated for at least six months or until no injectable melanomas were present. The primary endpoint was sustained response rate; H. the proportion of patients with a complete or partial response that persisted for at least six months. Secondary endpoints were overall survival , overall response rate, time to response, duration of response, and time to treatment failure. The sustained response rate was 16.3% with Talimogen laherparepvec treatment compared to 2.1% with GM-CSF. The overall response rate was 26.4% versus 5.7% in the GM-CSF group. With regard to overall survival (23.3 versus 18.9 months), the difference was not statistically relevant.
Subgroup analyzes showed that patients without involvement of the lungs or other internal organs benefited more from Imlygic therapy than those with more advanced disease.
According to an analysis to assess the systemic effects of Talimogen laherparepvec, skin lesions that had not been injected with the active substance decreased in 34.2% of the patients and in 11.3% also metastases inside the body were reduced by more than half.
Another phase III study is investigating the concomitant treatment of locally advanced squamous cell carcinomas of the head and neck with talimogen laherparepvec. The study is still ongoing.
Further information
The existing two-word generic name Ta lim o gen la herparepvec based on the set by the WHO root words for gene therapy drugs: the first word encoded with the final syllable -gen gene therapy use, -lim- represents immunomodulator ; the second word with the end of the word -repvec describes the vector principle (ie replicating viral vector ) and with -herpa- the virus family from which the active ingredient is derived.
In Germany, the Federal Joint Committee (G-BA) in the early benefit assessment according to Section 35a SGB V ( AMNOG ) of Talimogen laherparepvec in September 2016 did not determine any additional benefit compared to the existing standard therapies, since the authorization holder did not submit any correspondingly valid data on appropriate comparative therapies.
swell
Web links
- Imlygic on the website of the European Medicines Agency, there in particular: Assessment report Imlygic, Committee for Medicinal Products for Human Use (CHMP), 22 October 2015.
Individual evidence
- ^ Pharmaceutical newspaper online, news: T-Vec: Oncolytic immunotherapy on the market , July 1, 2016.
- ↑ What Is IMLYGIC? Description of the mechanism of action on the Amgen website, 2017
- ↑ For the stages of malignant melanoma see: Malignant Melanoma Staging - TNM Classification for Malignant Melanoma , W. Tan Winston on Medscape, as of October 1, 2015.
- ↑ Amgen Clinical Trials - Clinical Study Report (CSR) Synopses , accessed April 21, 2017.
- ↑ WHO: The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances, 2011 , Annex 4, p. 181.
- ↑ IQWiG reports - No. 431: Talimogen laherparepvec (melanoma) - Benefit assessment according to Section 35a SGB V , Joint Federal Committee (G-BA), as of September 9, 2016.