Lyell syndrome
| Classification according to ICD-10 | |
|---|---|
| L51.2 | Toxic Epidermal Necrolysis (Lyell's Syndrome) |
| L00 | Staphylococcal scalded skin syndrome (SSS syndrome) Dermatitis exfoliativa neonatorum (Ritter (-von-Rittershain)) Pemphigus acutus neonatorum |
| ICD-10 online (WHO version 2019) | |
The Lyell syndrome , also known as Epidermolysis necrolysis or scalded skin syndrome referred to is a rare, after the Scottish dermatologist Alan Lyell named acute skin change caused by bubble detachment of the epidermis of the skin ( "scalded skin syndrome") is characterized.
The death rate is between 25 and 70% depending on the extent of the damage.
There are two forms of Lyell syndrome. The drug-induced Lyell syndrome ( toxic epidermal necrolysis , TEN) and the staphylogenic Lyell syndrome ( staphylococcal scalded skin syndrome , SSSS).
Epidemiology
In Germany, the incidence of drug-induced Lyell's syndrome is 0.93 per 1,000,000 people per year and for staphylogenic Lyell's syndrome between 0.09 and 0.13 per 1,000,000 people per year. In France, the incidence for drug-induced Lyell's syndrome is 1.2 per 1,000,000 population per year and for staphylogenic Lyell's syndrome is 0.56 per 1,000,000 population per year.
The drug-induced Lyell syndrome (TEN)
The drug-induced Lyell syndrome occurs as a cytotoxic allergic reaction to drugs, especially in adults, less often in children. Due to the very similar clinic and histopathology, TEN can be viewed as the maximum form of Stevens-Johnson syndrome .
According to the drug commission of the German medical profession, the following drugs are considered possible triggers:
- antibacterial sulfonamides , for example cotrimoxazole (mixture of sulfamethoxazole and trimethoprim )
- Anticonvulsants, for example phenytoin , carbamazepine , lamotrigine
- Analgesics and nonsteroidal anti-inflammatory drugs, especially pyrazolones such as metamizole
- Allopurinol .
More recent study data suggest that the association between TEN and sulfonamides is rather weak and, in the case of cotrimoxazole, appears to be based on its component trimethoprim. Several cases have been described in which treatment with fluoroquinolone antibiotics has resulted in fatal courses of TEN. These also affected patients without predisposing risk factors. Interactions between fluoroquinolones and T cells are assumed to be the cause. However, it should be noted that severe skin reactions can generally also occur when taking many other drugs. In the case of drugs that are to be taken long-term, the risk is usually highest in the first two months.
Lyell's Staphylogenic Syndrome (SSSS)
The staphylogenic Lyell syndrome (staphylococcal scalded skin syndrome) is caused by the exotoxin exfoliatin of the bacterium Staphylococcus aureus of phage group II. It mainly affects infants in the first three months of life. Often it is preceded by a purulent infection of the skin, conjunctiva , purulent otitis or pharyngitis . In adults there is immunity through neutralizing antibodies against the exfoliate . However, immunocompromised adults can also become ill.
Clinical appearance and course
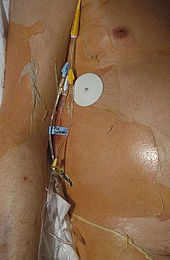
The drug-induced Lyell syndrome
There is initially a prodromal phase with malaise, loss of appetite, rhinitis and fever. This can last between 2 and 21 days. Following this, the disease goes into an acute phase. If the fever persists, extensive erythema occurs . There is extensive necrosis-related detachment of the epidermis. The Nikolsky sign is positive. The necrosis can also affect the mucous membranes, especially the oral mucosa. The acute phase is followed by a one to two week re-epithelialization phase.
Possible complications are infections with sepsis , leukopenia up to agranulocytosis or scarring in the healing phase.
Lyell's staphylogenic syndrome
Initially, there is fever and generalized erythema. Bubbles with sterile contents form within 24 hours. The Nikolsky sign is positive. Lyell's staphylogenic syndrome can be localized or generalized anywhere on the body. The lesions usually heal without scarring within 14 days.
Diagnosis
An immediate skin biopsy and swabs help to differentiate the drug form from the infectious form. In the differential diagnosis, large-bladder impetigo contagiosa , Stevens-Johnson syndrome and scarlet fever rash must be considered.
histology


Histologically, drug-induced Lyell's syndrome shows a gap and detachment of the entire epidermis , while staphylogenic Lyell's syndrome detaches the stratum corneum from the stratum granulosum .
The drug-induced form shows histologically a subepidermal blister with a superficial infiltrate of lymphocytes and occasionally granulocytes . The entire epidermis is detached and necrotic with a normal wicker-like stratum corneum. The papillae of the dermis are intact. There are isolated extravasations of erythrocytes .
The staphylogenic form shows histologically a bladder cover consisting only of the stratum corneum of the skin; cells from the stratum granulosum can occasionally be found here. There are scant inflammatory infiltrates and the contents of the bladder are sterile.
Differential diagnosis
A distinction must be made between epidermolytic ichthyosis and DRESS syndrome (Drug Rash with Eosinophilia and Systemic Symptoms).
therapy
Immediate intensive care monitoring and therapy is required. In addition to constant room temperature and humidity, patients need reverse isolation to avoid secondary infections . Symptomatic therapy is analogous to large-scale burns . In drug-induced Lyell's syndrome, all drugs must be discontinued immediately. The only exceptions are medicines that are absolutely essential for life. Systemic administration of corticosteroids as well as fluid and electrolyte administration to compensate for the losses are required. The staphylogenic Lyell syndrome is treated with β-lactamase-stable antibiotics . Corticoids are contraindicated here. Local therapy of the lesions is carried out with local antiseptic measures and surgical repair of necroses and infections.
Individual evidence
- ↑ a b c d e f Sterry et al: Dermatology Checklist 2010 Georg Thieme Verlag ISBN 978-3-13-697006-5
- ↑ a b c d Reinhold et al: Emergencies in Dermatology and Allergology 2012 Georg Thieme Verlag KG ISBN 978-3-13-116932-7
- ^ E. Schöpf, A. Stühmer, B. Rzany, N. Victor, R. Zentgraf, JF Kapp: Toxic epidermal necrolysis and Stevens-Johnson syndrome. An epidemiologic study from West Germany. In: Archives of Dermatology . Volume 127, Number 6, June 1991, pp. 839-842, ISSN 0003-987X . PMID 2036029 .
- ↑ M. Mockenhaupt, M. Idzko, M. Grosber, E. Schöpf, J. Norgauer: Epidemiology of staphylococcal scalded skin syndrome in Germany. In: Journal of Investigative Dermatology . Volume 124, Number 4, April 2005, pp. 700-703, ISSN 0022-202X . doi: 10.1111 / j.0022-202X.2005.23642.x . PMID 15816826 .
- ↑ JC Roujeau, JC Guillaume, JP Fabre, D. Penso, ML Fléchet, JP Girre: Toxic epidermal necrolysis (Lyell syndrome). Incidence and drug etiology in France, 1981-1985. In: Archives of dermatology. Volume 126, Number 1, January 1990, pp. 37-42, ISSN 0003-987X . PMID 2134982 .
- ↑ V. Lamand, O. Dauwalder, A. Tristan, JS Casalegno, H. Meugnier, M. Bes, O. Dumitrescu, M. Croze, F. Vandenesch, J. Etienne, G. Lina: Epidemiological data of staphylococcal scalded skin syndrome in France from 1997 to 2007 and microbiological characteristics of Staphylococcus aureus associated strains. In: Clinical Microbiology and Infection . Volume 18, Number 12, December 2012, pp. E514-E521, ISSN 1469-0691 . doi: 10.1111 / 1469-0691.12053 . PMID 23078129 .
- ^ A. Meves: Dermatology intensive course. 1st edition, Urban & Fischer, Munich 2006, ISBN 978-3-437-41162-5
- ↑ Drugs Commission of the German Medical Association. Drug-induced severe skin reactions. Deutsches Ärzteblatt 95, Issue 49, December 4, 1998 (accessed November 28, 2012)
- ↑ Antibiotic Drug Use and the Risk of Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: A Population-Based Case-Control Study . In: Journal of Investigative Dermatology . December 19, 2017, ISSN 0022-202X , doi : 10.1016 / j.jid.2017.12.015 ( sciencedirect.com [accessed April 6, 2018]).
- ↑ TonyC.K. Tham, Grace Allen, Dorothy Hayes, Brendan Mcgrady, JamesG. Riddell: Possible association between toxic epidermal necrolysis and ciprofloxacin . In: The Lancet . tape 338 , no. 8765 , August 24, 1991, ISSN 0140-6736 , doi : 10.1016 / 0140-6736 (91) 90602-L ( thelancet.com [accessed April 6, 2018]).
- ↑ AB Yerasi, MD Oertel: Ciprofloxacin-induced toxic epidermal necrolysis . In: The Annals of Pharmacotherapy . tape 30 , no. 3 , March 1996, ISSN 1060-0280 , p. 297 , doi : 10.1177 / 106002809603000317 , PMID 8833569 .
- Jump up ↑ Marc R. Matthews, Daniel M. Caruso, Bradley J. Phillips, Laura G. Csontos: Fulminant Toxic Epidermal Necrolysis Induced by Trovafloxacin . In: Archives of Internal Medicine . tape 159 , no. 18 , October 11, 1999, ISSN 0003-9926 ( jamanetwork.com [accessed April 6, 2018]).
- ↑ SL Report: Ofloxacin: a probable cause of toxic epidermal necrolysis . In: The Annals of Pharmacotherapy . tape 35 , no. November 11 , 2001, ISSN 1060-0280 , p. 1388-1390 , doi : 10.1345 / aph.1Z433 , PMID 11724089 .
- ↑ C Açikel, E Ülkür, B Çeliköz: Fatal ciprofloxacin-induced toxic epidermal necrolysis (Lyell syndrome): A case report and review of the literature . In: Marmara Medical Journal . tape 15 , July 1, 2002, p. 189–193 ( researchgate.net [accessed April 6, 2018]).
- ↑ Bhaskar Mandal, Michael Steward, Sudhir Singh, Hywel Jones: Ciprofloxacin-induced toxic epidermal necrolysis (TEN) in a nonagerian: a case report . In: Age and Aging . tape 33 , no. 4 , July 2004, ISSN 0002-0729 , p. 405-406 , doi : 10.1093 / aging / afh088 , PMID 15115708 .
- ↑ Galicia Davila, Javier Ruiz-Hornillos, Patricia Rojas, Francisco De Castro, Jose M. Zubeldia: TOXIC EPIDERMAL NECROLYSIS INDUCED BY LEVOFLOXACIN . In: Annals of Allergy, Asthma & Immunology . tape 102 , no. 5 , May 1, 2009, ISSN 1081-1206 , doi : 10.1016 / S1081-1206 (10) 60521-2 ( annallergy.org [accessed April 6, 2018]).
- ↑ Bhandarkar Anoosha, Kop Priyadarshini, Pai Varadraj, Navin Patil: A REPORT OF FIVE CASES OF FLUOROQUINOLONE-INDUCED EPIDERMAL NECROLYSIS AT A TERTIARY CARE TEACHING HOSPITAL IN NORTHERN KARNATAKA . tape 3 , July 22, 2014 ( researchgate.net [accessed April 6, 2018]).
- ↑ Jhanvi J. Vaghela, Vivek N. Nimbark, Bhavesh C. Chavda, Hita H. Mehta, Bhargav M. Purohit: A Rare Case Report of Toxic Epidermal Necrolysis due to Ofloxacin . In: Current Drug Safety . March 2, 2018, ISSN 2212-3911 , doi : 10.2174 / 1574886313666180302124012 , PMID 29506464 .
- ↑ CA Livasy, AM Kaplan: Ciprofloxacin-induced toxic epidermal necrolysis: a case report . In: Dermatology (Basel, Switzerland) . tape 195 , no. 2 , 1997, ISSN 1018-8665 , p. 173-175 , doi : 10.1159 / 000245726 , PMID 9310730 .
- ↑ Sarita Nori, Chris Nebesio, Ryan Brashear, Jeffrey B. Travers: Moxifloxacin-Associated Drug Hypersensitivity Syndrome With Toxic Epidermal Necrolysis and Fulminant Hepatic Failure . In: Archives of Dermatology . tape 140 , no. December 12 , 2004, ISSN 0003-987X , doi : 10.1001 / archderm.140.12.1537 ( jamanetwork.com [accessed April 6, 2018]).
- ↑ AFM Saiful Islam, Md Sayedur Rahman: Levofloxacin-Induced Fatal Toxic Epidermal Necrolysis . In: The Annals of pharmacotherapy . tape 39 , July 1, 2005, p. 1136–7 , doi : 10.1345 / aph.1E613 ( researchgate.net [accessed April 6, 2018]).
- ↑ Niti Mittal, Adesh Mishra, Prashant Urade, MC Gupta: Fatal case of ciprofloxacin induced Toxic epidermal necrolysis . In: International Journal of Basic & Clinical Pharmacology . January 1, 2014, p. 1 , doi : 10.5455 / 2319-2003.ijbcp20141208 ( researchgate.net [accessed April 6, 2018]).
- ↑ Maria Gloria Aversano, Jan Schroeder, Antonella Citterio, Joseph Scibilia, Chiara Gamba: Levofloxacin induced Stevens-Johnson syndrome / toxic epidermal necrolysis overlap syndrome: case reports . In: Clinical and Translational Allergy . tape 4 , no. 3 , July 18, 2014, ISSN 2045-7022 , p. P91 , doi : 10.1186 / 2045-7022-4-S3-P91 .
- ↑ a b c d Constantin E. Orfanos, Claus Garbe: Therapy of Skin Diseases 2002, Springer Verlag
- ↑ a b c Andreas Plettenberg, Helmut Schöfer, Wilhelm Meigel: Infectious diseases of the skin: Fundamentals, diagnostics and therapeutic concepts for dermatologists, internists and pediatricians 2010, Georg Thieme Verlag
- ↑ Antonio Cardesa, Thomas Mentzel, Pierre Rudolph, Pieter J. Slootweg: Pathology: head and neck region, soft tissue tumors, skin 2008 Springer Verlag
- ↑ a b Helmut Kerl, Claus Garbe, Lorenzo Cerroni, Helmut Wolff Histopathologie der Haut 2003, Springer Verlag