Non-opioid analgesic
A non-opioid analgesic (synonym non-opioid analgesic ) is a pain reliever drug ( analgesic ) that does not develop its effect by binding to opioid receptors and is therefore not an opioid . Many non-opioid analgesics have an analgesic , antipyretic and anti- inflammatory effect by inhibiting the enzyme cyclooxygenase (COX) and thus inhibiting prostaglandin synthesis . Substances that act as lipoxygenase inhibitors have recently been developed . Many non-opioid analgesics are available in pharmacies in Germany without a prescription . Typical representatives of the non-opioid analgesics are NSAIDs , COX-2 inhibitors , paracetamol and metamizole .
Mechanism of action
The mechanism of action of non-opioid analgesics is not uniform. By blocking the cyclooxygenases COX-1 and COX-2, most of them inhibit the synthesis of prostaglandins , which are formed as inflammation-promoting substances when tissue is damaged. These include not only the prostaglandins and their derived prostacyclins and thromboxanes and leukotrienes . The non-opioid analgesics that inhibit cyclooxygenases are known as prostaglandin synthesis inhibitors .
These substances affect elementary body functions to varying degrees. They influence the kidney blood flow, sodium excretion, platelet aggregation and bronchial, intestinal and uterine tone .
In connection with the development and maintenance of pain, influences on vascular tone , chemotaxis and vascular permeability play a role. These processes are crucial for inflammatory processes.
The prostaglandins are of particular interest in connection with the non-opioid analgesics. In addition to inflammatory processes, they also influence other physiological functions. They play a protective role for the gastric mucosa (acid protection) and kidney function (sodium and water excretion). There are two aspects to consider:
- There are several prostaglandins that have different effects at different sites of action.
- There are at least two types of cyclooxygenase that represent different synthetic pathways for prostaglandins. Cyclooxygenase-2 (COX-2) plays a role in the synthesis of inflammation mediators , while COX-1 is crucial for the synthesis of prostaglandins, which are responsible for mucosal protection, blood clotting (platelet aggregation) and the regulation of the electrolyte and water balance .
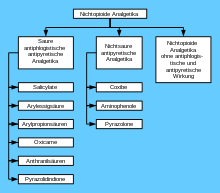
classification
The non-opioid analgesics are chemically heterogeneous substances. The acidic anti-inflammatory anti- pyretic analgesics are also referred to in human medicine as non-steroidal anti-inflammatory drugs (NSAP) or acid anti-inflammatory drugs . In veterinary medicine, on the other hand, NSAP or NSAID ( English non-steroidal anti-inflammatory drug ) refers to all non-opioid analgesics, including non-acidic ones.
Acid anti-inflammatory antipyretic analgesics
Acid anti-inflammatory antipyretic analgesics are acids. Because of this and because of their high protein binding, they accumulate particularly in tissues with a low pH value (in non-dissociated form). For this reason, they can be detected in particularly high concentrations in inflamed tissue, where they counteract the inflammation.
High concentrations are also found in the gastric mucosa and kidneys. Significant side effects result from this fact. When local prostaglandin synthesis is eliminated, its gastric mucosal protective effect (reduced mucus production and reduced blood flow to the gastric wall) is lost, which can lead to gastric ulcerations (gastric ulcer, ulcus ventriculi ) and subsequent gastric bleeding.
Salicylates
The salicylates group of substances includes:
- Acetylsalicylic acid (ASA), the most important representative
- 5-aminosalicylic acid (mesalazine), colon anti-inflammatory drug
- Diflunisal (trade name Fluniget ), not available in Germany
- Ethenzamide ( 2-ethoxybenzamide ), only as a combination partner in an influenza drug
- Salicylamide , not available in Germany
- Salacetamide , not available in Germany
Acetylsalicylic acid (ASA) - introduced as a drug since 1899 - is available for oral and intravenous administration. In addition to the use in inflammation-related pain, the platelet aggregation-inhibiting effect can also be used to prevent microembolisms in connection with myocardial infarction and cerebral ischemic stroke ( stroke ).
Anthranilic acid derivatives
Anthranilic acid derivatives are structurally closely related to the salicylic acid derivatives. These include:
Arylacetic acid derivatives
The arylacetic acid derivatives include:
- Diclofenac
- Indomethacin
- Aceclofenac is said to have a cartilage-building effect
- Acemetacin (trade name Rantudil ),
- Lonazolac
- Tolmetin , not available in Germany
- Ketorolac , used only in eye drops
- Lumiracoxib , strong COX-2-inhibiting effect (→ coxibs )
- Bufexamac
- Felbinac
Diclofenac can lead to liver and kidney damage and typically to gastric mucosa damage (reduced protective effect of the prostaglandins there).
Arylpropionic acid derivatives
The arylpropionic acid derivatives include:
Dexketoprofen and dexibuprofen are the optically right-handed enantiomers of the racemates ketoprofen and ibuprofen, respectively.
Ibuprofen is often given to treat chronic joint pain (e.g. back pain). Although attention is drawn to the general risk of acute kidney failure from all NSAIDs, the agent can be used well in postoperative pain therapy. Its rapid onset of action, which begins about 15 minutes after oral administration, is beneficial (for comparison: oral paracetamol after 2 hours). An injection solution is now also available for intravenous or intramuscular administration in the case of moderate to severe pain.
Oxicame
Oxicams are enolic acids. They include:
- Piroxicam
- Tenoxicam
- Lornoxicam , the first oxicam with a short plasma half-life.
- Meloxicam shows a preference for inhibiting COX-2.
Oxicams have a high to absolute bioavailability. Piroxicam, tenoxicam and meloxicam only have to be taken once a day due to their long plasma half-lives . Isoxicam was withdrawn from the market in 1985 and approval for Droxicam was suspended in 1994.
Pyrazolidinediones
Pyrazolidinediones are similar to the pyrazolones in terms of their basic structure , but acidic and therefore belong to the NSAIDs. Representatives are:
- Phenylbutazone
- Oxyphenbutazone , not available in Germany
- Kebuzon , not available in Germany
- Sulfinpyrazon , not available in Germany
- Mofebutazone
- Azapropazon , not available in Germany
Because of their severe side effects ( agranulocytosis ), these drugs are only used to a very limited extent.
Non-acidic antipyretic or anti-inflammatory antipyretic analgesics
In contrast to the acidic analgesics, the non-acidic antipyretic analgesics are largely evenly distributed in the organism. They are therefore well suited for the therapy of inflammation-independent pain (e.g. postoperative conditions); a well-known example is paracetamol .
The side effects on the kidneys ( acute and chronic kidney failure ) feared with acidic analgesics are not to be expected with non- acidic analgesics .
Coxibs
Coxibs are COX-2 inhibitors . They include:
- Rofecoxib , withdrawn from the market because of cardiovascular damage.
- Celecoxib ,
- Parecoxib , withdrawn from the market in Switzerland due to cardiovascular damage.
- Valdecoxib , withdrawn from the market due to cardiovascular damage and severe skin reactions.
- Etoricoxib ,
- Lumiracoxib
Coxibs selectively inhibit cyclooxygenase 2, which is why they are also called COX-2 blockers. With the inhibition of COX-2, the synthesis of prostaglandins, which function in the sense of the inflammatory response, is prevented. The prostaglandins, which are responsible for gastric protection and platelet aggregation, are less affected. This would prevent the biggest problem with long-term use of NSAIDs, the development of gastritis and gastric bleeding.
The hopes for the greatest freedom from side effects of the coxibs have not been fulfilled. The recording of adverse drug effects results in an accumulation of hypertension and myocardial infarction for the coxib with long-term use. Whether these side effects are a group effect of only the coxibs or a side effect of all NSAIDs is currently the subject of further research. The Drugs Commission of the German Medical Association (AkdÄ) has since derived the following recommendations:
- Coxibs are contraindicated in patients with pre-existing cardiovascular disease,
- A relative contraindication exists in patients over 65 years of age,
- The application is to be limited to a maximum of six months,
- The relative contraindication is perioperative therapy,
- In patients with cardiovascular and gastrointestinal risks, NSAIDs with gastric protection or similar should be avoided until the knowledge has been concretized.
Aminophenols
Paracetamol belongs to this group . In its intravenous form, it is particularly suitable for postoperative pain therapy. It has become firmly established in paediatrics, but mostly due to the lack of alternatives. If the maximum daily dose is exceeded, liver cell necrosis, hepatic coma and death can occur. If the liver is damaged, these effects are more likely to occur, which is why this is a contraindication for the use of paracetamol.
Pyrazolones
The pyrazolones include:
- Phenazone ,
- Propyphenazone ,
- Metamizole ,
- Aminophenazon , no longer on the market in Germany
Phenazone, synthesized by Ludwig Knorr in 1883, is one of the first synthetic drugs. Aminophenazone as a further development of phenazone has been replaced by propyphenazone in combination preparations since 1977 due to the carcinogenic metabolite dimethylnitrosamine . Ramifenazone (4-isopropylaminoantipyrine) has a similar structure. As a hydrochloride, it is water-soluble and therefore allows parenteral administration. A similar preparation is piperylon.
Another pyrazolone derivative that is present as a water-soluble salt and can accordingly be administered parenterally is metamizole. Metamizole also has spasmolytic activity on the smooth muscles. Agranulocytoses have been observed after administration of metamizole . The substance is not or no longer approved in the USA, England and other countries.
In some countries, such as B. in Germany in August 1982 by the Federal Health Office , the approval of 80 pyrazolone-containing combination products was revoked after they were suspected of causing damage to the blood count and shock states in rare cases.
Non-opioid analgesics without anti-inflammatory and anti-pyretic properties
Flupirtine belongs to this group . In addition to a moderate to strong analgesic effect - comparable to tramadol - flupirtine has a central muscle-relaxing effect on the skeletal muscles. It is used for acute and chronic pain, e.g. B .:
- painful muscle tension in the holding and movement muscles
- Tension headache
- Tumor pain
- Dysmenorrhea
- Pain after traumatological / orthopedic operations and injuries.
The side effects are fatigue (10–25%) and dizziness (5%). In addition, the urine may turn green (without clinical consequences). Due to the occurrence of liver damage, its use was restricted in 2013 and withdrawal from the market was recommended in 2018.
Combination preparations
In many drugs, various non-opioid analgesics are combined with one another and / or additionally with caffeine . The combination of acetylsalicylic acid, paracetamol and caffeine is the most widespread and contained in Boxonal N , Neuralgin , Ratiopyrin , Thomapyrin , Titralgan or Tsitramon P, for example . These combinations are controversial in the professional world.
Several studies (e.g. Diener et al., 2005) and at least one meta-study confirm a superadditive enhancement of the effect. The undesirable drug effects should also be less severe, since the individual substances are dosed lower than in mono preparations . Several specialist societies for headaches and migraines then included the ASA-paracetamol-caffeine combination as the first choice in their guidelines. Although the recommendations z. For example, the German Migraine and Headache Society claims to be strictly evidence-based , but independence is repeatedly questioned.
On the other hand, there is a wide range of opposition. On the one hand, there is the argument that combination products should be rejected in principle because any complications that may arise are more difficult to treat. It has also been proven that these combination preparations are misused more often, ie taken too long and too often, than the corresponding monopreparations. Whether the abuse is caused by the combination itself (for example by the slightly stimulating effect of the caffeine) or by the superior effectiveness and better tolerability compared to the monopreparations has not yet been finally clarified.
Historical names
The non-opioid analgesics were also referred to as peripheral analgesics; this in contrast to the opioids, which act in the central nervous system . As central mechanisms of action have now been proven for some non-opioid analgesics, this designation has been abandoned.
For historical reasons, acidic antipyretic analgesics are also called non-steroidal anti-inflammatory drugs (NSAIDs) in human medicine . Originally, steroids were used to treat the chronic inflammation associated with rheumatism. With the discovery of the anti-inflammatory property of non-opioid analgesics, the latter substances were initially used in rheumatism treatment. It was only later that they became popular medicines for pain and fever.
Individual evidence
- ↑ Heinz Lüllmann, Klaus Mohr, Martin Wehling, Lutz Hein (eds.): Pharmacology and Toxicology . 18th edition. Georg Thieme Verlag, Stuttgart 2016, ISBN 978-3-13-368518-4 , p. 350 .
- ↑ Wolfgang Löscher, Fritz Rupert Ungemach, Reinhard Kroker: Pharmacotherapy for domestic and farm animals , Georg Thieme, Stuttgart 2006, ISBN 9783830441601 , pp. 103-108 and 364-380.
- ↑ Consolidated List of products whose consumption and / or sale have been banned, withdrawn, severely restricted or not approved by Governments , United Nations, 2003, pp. 116 + 123 (Edition 2005) (English) , accessed on February 16, 2016.
- ↑ Drugs Commission of the German Medical Association: Cardiovascular side effects are a class effect of all coxibs: consequences for their future prescription . Deutsches Ärzteblatt, 49/2004, p. A3365
- ↑ Entry on ramifenazone. In: Römpp Online . Georg Thieme Verlag, accessed on March 30, 2016.
- ↑ Rote-Hand-Brief on Flupirtin, July 15, 2013
- ↑ Klaus Aktories et al .: General and Special Pharmacology and Toxicology . Elsevier, Urban & FischerVerlag, 10th edition 2009, ISBN 9783437425226 , p. 178.
- ↑ Roland Braun: Manual der Schmerztherapie , Georg Thieme, Stuttgart 2002, ISBN 9783131135636 , preview Google Books , pp. 11-13.