Vaginal cancer
| Classification according to ICD-10 | |
|---|---|
| C52 | Vaginal cancer |
| ICD-10 online (WHO version 2019) | |
A vaginal carcinoma , also called vaginal cancer , vaginal cancer , vaginal cancer , vaginal cancer or vaginal referred to is a relatively rare malignant tumor disease of the vagina .
Depending on the type of cell that has deteriorated, a distinction can be made between different types of cancer in vaginal cancer. Over 90% of all vaginal cancers originate from changes in the top layer of the mucous membrane . These are so-called squamous cell carcinomas (English: squamous cell carcinoma, abbreviated: SCC). The remaining 10% are adenocarcinomas (cancer of the glandular tissue) and melanomas (black skin cancer). About half of the carcinomas are located in the upper third of the vagina and on the back wall of the vagina.
Depending on the stage and degree of spread of the tumor, therapy is usually performed surgically or by radiation . If the diagnosis and subsequent therapy are made early, the prognosis for vaginal cancer is good and a complete cure is possible.
etiology

As with many other cancers, the causes of vaginal cancer are still largely unexplained and of a diverse nature. However, various risk factors are now known:
- Infections with the human papillomavirus (HPV) type 16 and 18. These viruses are the most common known causative agents of sexually transmitted diseases. They lead to wart-like changes in the vagina.
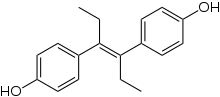
- Diethylstilbestrol (DES) is an artificial estrogen that was withdrawn from the market as a drug in 1971. It was given to pregnant women to prevent abortion . Due to the long latency period , carcinomas only occur at an advanced age or in girls whose mothers were treated with DES during pregnancy. DES-related carcinomas are adenocarcinomas .
- Also pessaries are suspected in certain circumstances to develop a Vaginalkarzinomes to be involved.
Epidemiology
Vaginal cancers are relatively rare cancers. From a statistical point of view, vaginal carcinomas are approximately 1 to 2% of all malignant tumors of the female genital organs . Worldwide, an average of around 0.4 in 100,000 women develop vaginal cancer every year. Usually women over 60 are affected by a new disease.
Symptoms
The symptoms of vaginal cancer appear at an advanced stage. Vaginal bleeding, which usually occurs after sexual contact , is usually the first abnormality. Increased, sometimes bloody, discharge is another common symptom. If the tumor has spread to surrounding tissue or other organs, abdominal pain or functional organ disorders, such as the urinary bladder or the intestine , may occur.
diagnosis
The diagnosis of vaginal cancer is usually made by chance during a gynecological check -up. If abnormalities are found in the routine cell smears (see Pap test ), this is usually followed by a colposcopy (magnifying glass examination of the inside of the vagina). In addition, a biopsy (the removal of a small tissue sample) is then usually performed.
Various imaging methods are used to assess the tumor stage, i.e. essentially the spread of the tumor :
- Sonography (ultrasound) of the vagina, usually with a vaginal probe
- Urethrocystoscopy (mirroring the urinary tract)
- Rectoscopy (reflection of the rectum)
In exceptional cases, computed tomography (CT) and magnetic resonance imaging (MRI) of the entire abdominal cavity are also performed.
Staging according to FIGO
The staging (Engl. Staging ) describes how far a malignant tumor has progressed. Therapy is usually based on this. The FIGO (International Association for Gynecology and Obstetrics) has defined the following stages for vaginal cancer :
- Stage 0: carcinoma in situ
- Stage I: The expansion is limited to the vaginal wall.
- Stage II: extension to the subvaginal tissue, but the pelvic wall is not affected.
- Stage III: the carcinoma reaches the pelvic wall.
- Stage IV A: The carcinoma has affected the mucous membrane of the bladder or rectum (rectum) or has crossed the pelvis .
- Stage IV B: spread to distant organs ( distant metastases )
therapy
For the treatment of vaginal cancer, surgery and radiation therapy (“steel and beam”) are used. The application of the respective procedure is, however, highly dependent on the stage and the spread of the disease.
surgery
Small vaginal carcinomas diagnosed at an early stage can be removed by surgery to preserve the organs. Extensive carcinoma often requires that the vagina be completely removed. Often parts of the bladder and intestine also have to be removed.
radiotherapy
There are basically two ways of irradiation:
- The brachytherapy , in which a small radiation source is applied in the immediate vicinity of the tumor.
- The teletherapy , that is irradiated with a radiation source from the outside.
With brachytherapy, irradiation can either be from the inside ( afterloading technique ) or from the outside through the skin ( percutaneous ).
chemotherapy
In most cases, chemotherapeutic treatment is only used if metastases , i.e. secondary tumors, have developed in other organs.
Course of disease
If the disease is not treated, there is always the risk that the tumors will grow (infiltrate) into the surrounding tissue and neighboring organs. Thereof mainly affects the cervix ( cervical ), the external genitalia ( vulva ), the bladder and the rectum ( rectal ). Vaginal cancer can spread throughout the body through the lymphatic system and then form lymph node metastases in the pelvic area. Metastasis to the liver , lungs and bones is less common . Large tumors in the pelvic area can obstruct the flow of urine, as the ureter can be blocked by the space required by the tumor. In the case of kidney congestion , life-threatening kidney damage is possible.
Individual evidence
- ↑ GL Pride et al .: Primary invasive squamous carcinoma of the vagina. In: Obstet Gynecol 53, 1979, pp. 218-225. PMID 2520784
- ↑ SC Rubin et al .: Squamous carcinoma of the vagina: treatment, complications, and long-term follow-up. In: Gynecol Oncol 20, 1985, pp. 346-353. PMID 3972294
- ↑ GL Eddy et al .: Primary invasive vaginal carcinoma. In: Am J Obstet Gynecol 165, 1991, pp. 292-296. PMID 1872329
- ↑ a b c d e f g h i j krebsgesellschaft.de: Vaginal cancer, vaginal cancer, vaginal cancer, vaginal cancer. Retrieved on December 18, 2007 ( Memento of the original from April 14, 2013 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice.
- ↑ a b c krebsgesellschaft.de: vaginal carcinoma ( Memento of the original October 20, 2013 Internet Archive ) Info: The archive link is automatically inserted and not yet tested. Please check the original and archive link according to the instructions and then remove this notice. (PDF; 184 kB)
- ↑ JR Daling: Risk of anogenital cancer in women with CIN. In Lancet Oncology 8, 2007, pp. 281-282. PMID 17395100
- ^ DM Parkin and F. Bray: Chapter 2: The burden of HPV-related cancers. In: Vaccine , 24, 2006, pp. 11-25. PMID 16949997 (Review)
- ↑ JR Daling et al.: A population-based study of squamous cell vaginal cancer: HPV and cofactors. In: Gynecologic oncology 84, 2002, pp. 263-270. PMID 11812085
- ^ E. Müller-Holzner: Gynäkopathologie. 3rd edition 1996, Studia Innsbruck
- ↑ A. Jain et al .: How innocent is the vaginal pessary? Two cases of vaginal cancer associated with pessary use. In: J Obstet Gynaecol 26, 2006, pp. 829-830. PMID 17130056
- ↑ G. Lamotte: Primary adenocarcinoma of the vagina due to the use of a pessary. In: Bull Soc R Belge Gynecol Obstet 39, 1969, pp. 287-294. (in French)
- ↑ PT Tran et al .: Prognostic factors for outcomes and complications for primary squamous cell carcinoma of the vagina treated with radiation. In: Gynecologic Oncology 105, 2007, pp. 641-649. PMID 17363046
- ↑ WT Creasman include: The national cancer data base report on cancer of the vagina. In: Cancer 83, 1998, pp. 1033-1040. PMID 9731908
- ↑ http://www.figo.org - Staging Classifications and Clinical Practice Guidelines for Gynaecological Cancers ( Memento of December 3, 2008 in the Internet Archive ) (PDF document)
- ↑ B. Sushil et al .: High-dose-rate brachytherapy (HDRB) for primary or recurrent vaginal cancer. In: Brachytherapy 6, 2007, p. 115.
- ^ L. Hughes-Davies et al .: Parametrial interstetial brachytherapy for advanced or recurrent pelvic malignancy: the Harvard / Stanford experience. In: Gynecol Oncol 58, 1995, pp. 24-27. PMID 7789885
literature
- FIGO: Annual Report on the Results of Treatment in Gynecological Cancer. In: J Epidem Biostat 6, 2001, pp. 141–152.
- D. Fournier et al .: Preneoplasias or neoplasms of the vagina. In: Clinic of Gynecology and Obstetrics,: H. Schmidt-Matthiesen (editor), Volume 11, 3rd edition. Urban & Schwarzenberg, Munich, 1991, pp. 105–127.
- YS Fu and JW Reagan: Epithelial neoplasms of the vagina. In: Pathology of the uterine cervix, vagina and vulva. Saunders, Philadelphia, 1989, pp. 193-224.
- D. Henson and R. Tarone: An epidemiologic study of cancer of the cervix, vagina and vulva based on the Third National Cancer Survey in the United States. In: Am J Obstet Gynecol 129, 1977, pp. 525-532. PMID 199064
- P. Kirkbride et al.: Carcinoma of the vagina - experience at the Princess Margret Hospital (1974-1989). In: Gynecol Oncol 56, 1995, pp. 435-443. PMID 7705681 (Review)
- CA Perez et al: vagina. In: Principles and practice of gynecologic oncology. Lippincott Philadelphia, 1992, pp. 567-590.
- K. Urbanski et al .: Primary invasive vaginal carcinoma treated with radiotherapy: analysis of prognostic factors. In: Gynecol Oncol 60, 1996, pp. 16-21. PMID 8557220
- R. Samant et al .: Primary vaginal cancer treated with concurrent chemoradiation using Cis-platinum. In: Int J Radiat Oncol Biol Phys 69, 2007, pp. 746-750. PMID 17512130
- TB Daniels et al: Radiation for Vaginal Cancer: The Mayo Clinic Experience In: International Journal of Radiation Oncology - Biology - Physics 69, 2007, p. 403.
- H. Malmström et al .: Primary invasive squamous cell carcinoma of the vagina. In: Acta Obstet Gynecol Scand 68, 1989, pp. 411-415. PMID 2520784
- JL Benedet et al .: Primary invasive carcinoma of the vagina. In: Obstet Gynecol 62, 1983, pp. 715-719. PMID 6633996
- R. Samant: Radiotherapy for the treatment of primary vaginal cancer. In: Radiotherapy and Oncology 77, 2005, pp. 133-136. PMID 16260055
- A. Viswanathan et al: The impact of brachytherapy dose in vaginal cancer. , International Journal of Radiation Oncology * Biology * Physics 57, 2003, p. 343.
- PW Grigsby: Vaginal Cancer. In: Curr Treat Options Oncol 3, 2002, pp. 125-130. PMID 12057075