Achalasia
| Classification according to ICD-10 | |
|---|---|
| K22.0 | Achalasia |
| ICD-10 online (WHO version 2019) | |
As achalasia a disease is referred to, in which the lower esophageal sphincter (entrance to the stomach, the lower esophageal sphincter ) does not open properly and the motility (mobility) of the muscles of the esophagus is disturbed. The term achalasia comes from the Greek ( achalasis = lack of relaxation) and was coined by Sir Arthur Hurst in 1927. Insufficient relaxation of the lower throat cord is known as cricopharyngeal achalasia .
Stages
Achalasia is divided into three stages.
- Stage I - hypermotile form
- Stage II - hypomotile form
- Stage III - amotile form
The disease progresses from the first to the last stage. In stage I the esophagus is still functional and tries to “pump” against the excessive pressure in the lower sphincter muscle (stomach entrance) (hypermotile = overmovable in the sense of overactive). In the second stage, the esophageal muscles become sluggish as the esophagus gradually expands (dilates). In the final stage of the disease (stage III), the esophagus finally “hangs” as a slack, functionless muscle tube in the mediastinum (middle space of the chest). The esophagus is defective and completely amotile (immobile).
New classification of achalasia based on the HRM
A new classification of achalasia is being established in clinical practice based on high-resolution manometry (HRM). A distinction is made between three different forms of contractility (mobility through contractions) in the tubular esophagus (tubular esophagus). In classic achalasia (type I), the esophagus shows few contractions. In type II achalasia, pressure builds up in the esophagus between the upper and lower sphincter muscles. In type III achalasia (spasmodic form) there are also spastic contractions, especially in the lower esophagus.
frequency
Achalasia is a rare disease with an incidence of about 1: 100,000 people per year and a prevalence (predominance) of about 10: 100,000 people. The gender ratio is balanced (men and women equally often). The typical age of onset is between 20 and 40 years. However, there is a second frequency peak in older people. Less than 5% of patients are children.
Causes and Disease Development
Primary achalasia
The cause of the disease is unknown. Scientific studies have shown an association of primary achalasia with the HLA antigen HLA-DQw1 and an increased number of antibodies directed against the autonomic nervous system in some patients . Based on these results, it can be assumed that achalasia is an autoimmune disease . In addition, pathogen-related causes were also considered. In particular, a possible involvement of varicella zoster viruses , measles viruses and human papillomaviruses were published. However, these assumptions could not be confirmed in more recent studies. In addition to immunological and pathogen-related causes, psychological and hereditary factors are also discussed.
More is known about the mechanisms of pathogenesis and pathophysiology than about the actual cause of the disease. Normally the act of swallowing triggers a peristaltic wave in the esophagus that transports the ingested food towards the stomach and leads to a reflex relaxation of the lower esophageal sphincter. The latter keeps the opening from the esophagus to the stomach closed with the exception of the act of swallowing, thus preventing gastric acid from flowing back.
In achalasia, the (propulsive) peristalsis in the lower esophagus is disturbed and the reflex relaxation of the lower esophageal sphincter during the act of swallowing is absent. This leads to a lack of emptying of the esophagus contents into the stomach and thus to a build-up of food components. This causes the swallowing difficulties typical of achalasia. Only when the hydrostatic pressure built up by the accumulating food exceeds the pressure of the esophageal sphincter caused by the contraction does the food components empty into the stomach.
The cause of the functional deficit of the esophagus is a degeneration of the nerve cells of the Auerbach myenteric plexus . The degeneration is triggered by an inflammatory reaction and mainly affects the nerve cells that inhibit the smooth muscles and thus lead to a lack of relaxation of the lower esophageal sphincter. The lack of inhibitory innervation not only leads to a lack of relaxation, but also to an increase in the basal sphincter pressure.
Secondary achalasia
Secondary achalasias can be caused by carcinomas, especially oesophageal and gastric carcinomas , or v. a. caused by Chagas disease in the tropics . These forms are also known as pseudoachalasia.
Further diseases that in rare cases can cause achalasia of the esophagus are amyloidosis , sarcoidosis , neurofibromatosis , eosinophilic esophagitis, multiple endocrine neoplasia type 2B , chronic idiopathic intestinal pseudo-obstruction and Fabry's disease .
Symptoms
The main symptom of the disease is swallowing disorders . Usually the symptoms increase steadily as the disease progresses. In summary, the following symptoms occur in achalasia:
- Difficulty swallowing ( dysphagia )
- Regurgitation
- Retrosternal pain , often related to the heart
- Aspirations , d. H. Passage of chyme into the windpipe
- Weight loss , rarely malnutrition, v. a. with children
Complications
The nocturnal regurgitations can lead to the development of aspiration pneumonia when food particles get into the airways. The prolonged stay of food components in the esophagus can cause secondary inflammation and thus what is known as retention esophagitis. On the one hand, this can lead to a shortening of the esophagus ( endobrachyesophagus ) and, on the other hand, is considered a precursor to esophageal carcinoma .
diagnosis
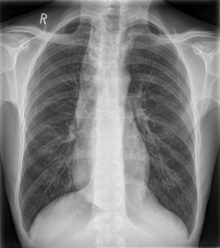
In the early stages, manometry ( pressure measurement ) is the method of choice in different sections of the esophagus (norm: 18–24 mmHg). Within the scope of this manometry one can determine the insufficient relaxation (opening) of the lower esophageal sphincter in combination with a pump dysfunction of the esophagus above the sphincter; in the late stage, the X-ray examination with contrast swallowing porridge ( barium porridge) shows characteristic findings. However, one cannot rely on these examinations alone if one also wants to exclude other causes of swallowing disorders (e.g. carcinomas, scar strictures, neurological disorders, rarely dysphagia lusoria , scleroderma , megaesophagus in Chagas disease ). Thus, an endoscopy of the upper digestive tract or a gastroscopy (gastroscopy) is required in routine diagnostics.
therapy
The cause of the achalasia is still not curable, but there are good treatment options for those affected to enable normal food intake and a symptom-free life again. The decision for one of the forms of therapy depends on the different requirements of the individual patient such as age, secondary diseases or the condition of the esophagus.
Pharmacological therapy
Drug therapy is only indicated for milder forms of achalasia. Nitrates and calcium channel blockers (e.g. nifedipine), which reduce the muscle tone of the esophageal sphincter and thus enable better passage of food, are suitable for therapy . Both substance groups have a short half-life , so that they are usually taken about 10 to 30 minutes before ingestion. Isosorbide dinitrate from the group of nitrates, for which the best effect in the treatment of achalasia has been proven, has proven itself . The pharmacological therapy of achalasia is considered less effective compared to the invasive therapy options. It is therefore mainly used in patients who refuse invasive therapy or are in a poor general condition, so that an invasive form of therapy is associated with greater risk of complications.
Balloon dilatation
The physical expansion ( balloon dilatation ) of the lower esophageal sphincter by balloon catheters, also known as pneumatic dilatation , tears the cardiac muscle and the passage becomes possible again.The treatment is usually not painful, as it is carried out as part of a gastroscopy with the help of a sedating drug . Balloon dilation carries a risk of esophageal perforation (2% of treatments); this often requires immediate emergency surgery. However, a large number of patients can remain permanently symptom-free with one or more endoscopic dilation.
Operative therapy
As a surgical therapy option, the laparoscopic myotomy according to Heller is used more and more frequently, which can usually achieve permanent freedom from symptoms in the hands of an experienced surgeon.
The results of the myotomy are excellent at first, but over the course of 10 to 15 years, achalasia will recur in up to 10% of sufferers. Often the esophagus is already greatly dilated, aperistaltic and tortuous. In this situation, sometimes even the esophagus had to be removed, an operation that is risky even in experienced hands. The method of transgastric esophagofundostomy developed by an Austrian team of doctors in 2007 is much gentler .
Peroral Endoscopic Myotomy (POEM)
Peroral endoscopic myotomy (POEM) is used as a new procedure, which enables myotomy in a purely endoscopic way, without cutting the abdomen. With the flexible endoscope (gastroscope) an incision is first made on the esophageal mucosa. Then a tunnel is formed under the mucous membrane and the mucous membrane is lifted off. This tunnel continues from the esophagus to the stomach. In the next step, the diseased muscles at the transition between the esophagus and stomach (cardia) are cut (myotomy). Finally, the mucosal entrance is closed again with endoscopically placed clips. The procedure is performed under general anesthesia.
The pioneer of the method is Professor Haruhiro Inoue from Showa University in Japan, who was the first to publish the application of this method in 17 achalasia patients in 2010 with very good treatment results. In the western world, POEM was first used at the University Medical Center Hamburg-Eppendorf (UKE) in 2010 and the first results were published. In addition, further follow-up studies from specialized endoscopy centers around the world confirmed these results. The patient's safety of the procedure and the short-term results are very good (very good relief of swallowing difficulties, little reflux, very good treatment of chest pain). In the medium term (at least 2 years) the treatment results remain stable at almost 80%. Long-term results are still pending. Prospective studies are currently ongoing to compare POEM with the previous standard procedures, laparoscopic Heller myotomy and pneumatic dilation (balloon expansion), in order to determine the value of the new treatment for achalasia.
Botulinum toxin injection
Endoscopic injection of botulinum toxin into the esophageal sphincter partially paralyzes the muscle so that the opening to the stomach is widened, making it easier for the pulp to pass through again. In various studies, the effect of a single treatment lasts on average for about six months and must therefore be repeated regularly.
Esophagectomy
Surgical removal of the esophagus ( esophagectomy ) is rarely required in achalasia. Even with advanced achalasia, myotomy can usually still help (e.g. Sweet et al., 2008). In the final stages of the disease, a myotomy is no longer effective. The only therapy that can be used here is esophagectomy. For the reconstruction, a section of the large intestine is usually inserted as an "interposal".
psychotherapy
Gerhard Klumbies reported in 1988 about treatments on 31 achalasia patients: “If we take stock of our observations [...], the psychotherapeutic treatment [...] has impressively proven itself [...]. Our psychotherapy usually consisted of hypnosis treatment, an introduction to autogenic training and psychagogical guidance. "
history
In 1672 Sir Thomas Willis successfully treated a patient with dysphagia and widening of the esophagus by dilating the esophagus with a whale bone. In 1881 Johann von Mikulicz described this disease as a consequence of cardiaspasm and was the first to point out the component of the functional disorder. In 1929, Hurt and Rake recognized the problem as a failure of the lower esophageal sphincter to open. They also introduced the term "achalasia" into medicine. In the early 1990s , the treatment of achalasia was revolutionized with the development of endoscopy and minimally invasive surgery .
See also
- Triple-A syndrome , a very rare hereditary disease with a. Achalasia.
literature
- Manuel Döhla: About the character of epithelial inflammation in achalasia . Medical dissertation. Erlangen 2018, DNB 1173170618 .
- Martin Allgower, J. Rüdiger Siewert (editors: R. Bumm and RB Brauer): Surgery. 8th, completely revised edition. Springer, Berlin a. a. 2006, ISBN 3-540-30450-9 .
- HJ Stein, H. Feussner, BHA von Rahden and others: Benign diseases of the esophagus and cardia - Chap. 24.7.1 Achalasia. In: JR Siewert, M. Rothmund, V. Schumpelick (ed.): Practice of visceral surgery: Gastroenterological surgery. , 3rd, newly edited and extended Edition. Springer, Berlin / Heidelberg a. a. 2011, ISBN 978-3-642-14222-2 .
- H. Rütze, H. Schulz: A life with achalasia. Achalasia Self-Help e. V., Münster 2008; 4th edition, by H. Rütze, I. Gockel and P. Schweikert-Wehner. Selbsthilfe Selbstverlag, Mechernich, 2018, ISBN 978-3-00-044249-0 .
- F. Farrokhi, MF Vaezi: Idiopathic (primary) achalasia. In: Orphanet J Rare Dis. 2, Sep 26, 2007, p. 38. PMID 17894899 , PMC 2040141 (free full text)
- I. Gockel, M, Müller, J. Schumacher: Achalasia - a disease of unknown cause that is often diagnosed too late. In: Deutsches Ärzteblatt . Int. 109 (12), 2012, pp. 209-214. doi: 10.3238 / arztebl.2012.0209
- JF Mayberry: Epidemiology and demographics of achalasia. In: Gastrointest Endosc Clin N Am. 11, 2001, pp. 235-248.
- MP Sweet, I. Nipomnick, WJ Gasper, K. Bagatelos, JW Ostroff, PM Fisichella, LW Way, MG Patti: The outcome of laparoscopic Heller myotomy for achalasia is not influenced by the degree of esophageal dilatation. In: Journal of Gastrointestinal Surgery . 12 (1), 2008, pp. 159-165. PMID 17710504 .
- AF Hurst: The treatment of achalasia of the cardia: so-called 'cardiospasm.' In: Lancet. i, 1927, p. 618.
- E. Heller: Extramucous cardioplasty in chronic cardiospasm with dilation of the esophagus . In: Mitt Grengeb Med Chir. 2, 1913, pp. 141-149.
- BHA von Rahden, J. Filser, S. Reimer, CT Germer: Peroral endoscopic myotomy (POEM) for the therapy of achalasia: own initial experiences and literature review. In: surgeon. 85 (5), 2014, pp. 420-432. doi: 10.1007 / s00104-013-2639-0
- BHA von Rahden, J. Filser, F. Seyfried, S. Veldhoen, S. Reimer, CT Germer: Diagnostics and therapy of achalasia / [Diagnostics and therapy of achalasia]. In: surgeon. 85 (12), Dec 2014, pp. 1055-1063. doi: 10.1007 / s00104-014-2803-1 .
- D. von Renteln, M. Schoenberg, Y. Werner, O. Mann, T. Rösch: Achalasia. In: DMW - German Medical Weekly. 138, 2013, p. 1240, doi: 10.1055 / s-0033-1343194 .
- Daniel Von Renteln, Karl – Hermann Fuchs a. a .: Peroral Endoscopic Myotomy for the Treatment of Achalasia: An International Prospective Multicenter Study. In: Gastroenterology. 145, 2013, p. 309, doi: 10.1053 / j.gastro.2013.04.057 .
- AJ Bredenoord, T. Rösch, P. Fockens: Peroral endoscopic myotomy for achalasia. In: Neurogastroenterology & Motility. 26, 2014, p. 3, doi: 10.1111 / nmo.12257 .
- YB Werner, T. Rösch: Endoscopic Myotomy. In: The gastroenterologist. 12, 2017, p. 223, doi: 10.1007 / s11377-017-0166-0 .
- Yuki B. Werner, Thomas Rösch: POEM and Submucosal Tunneling. In: Current Treatment Options in Gastroenterology. 14, 2016, p. 163, doi: 10.1007 / s11938-016-0086-y .
Web links
- Achalasia Consortium Germany's largest (genetic) research group on achalasia
- Information page about the POEM method for achalasia therapy Showa University in Yokohama, Japan
- achalasie.info - current information on the diagnosis and therapy of achalasia for patients and doctors
- speiseroehrenzentrum.de - specialized center for benign and malignant diseases of the esophagus at the UKE Hamburg with information, specialist center for achalasia with a research focus on POEM
- Achalasia self-help - exchange for achalasia sufferers
References and comments
- ↑ a b New classification of achalasia based on the HRM. In: JE Pandolfino et al: Gastroenterology. 2008.
- ^ RK Wong et al.: Significant DQw1 association in achalasia. In: Dig Dis Sci. 34 (3), Mar 1989, pp. 349-352. PMID 2920639
- ^ GN Verne et al: Anti-myenteric neuronal antibodies in patients with achalasia. A prospective study. In: Dig Dis Sci. 42 (2), Feb 1997, pp. 307-313. PMID 9052511 .
- ↑ a b c S. J. Spechler et al: Pathophysiology and etiology of achalasia. In: UpToDate. August 2007.
- ↑ CS Robertson, BA Martin, M. Atkinson: Varicella-zoster virus DNA in the oesophageal myenteric plexus in achalasia. In: Good. 34 (3), Mar 1993, pp. 299-302. PMID 8386130
- ↑ H. Niwamoto et al .: Are human herpes viruses or measles virus associated with esophageal achalasia? In: Dig Dis Sci. 40 (4), Apr 1995, pp. 859-864. PMID 7720482
- ↑ S. Birgisson et al .: Achalasia is not associated with measles or known herpes and human papilloma viruses. In: Dig Dis Sci. 42 (2), Feb 1997, pp. 300-306. PMID 9052510 .
- ↑ D. Henne-Bruns, B. Kremer, M. Dürig: Duale series surgery. 3. Edition. Thieme, 2008, ISBN 978-3-13-125293-7 .
- ↑ caused, triggered
- ↑ Innervation: equipment (of a body part) with nerves; Conducting stimuli via the nerves to an organ, nerve supply to an organ or area of the body
- ↑ TJ Vogl, W. Reith, EJ Rummeny (ed.): Diagnostic and interventional radiology. Springer-Verlag, Berlin 2010, ISBN 978-3-540-87667-0 .
- ^ I. Gockel, VF Eckardt, T. Schmitt, T. Junginger: Pseudoachalasia: a case series and analysis of the literature. In: Scandinavian journal of gastroenterology. Volume 40, Number 4, April 2005, ISSN 0036-5521 , pp. 378-385. PMID 16028431 . (Review).
- ↑ a b c M. Classen, V. Diehl, K. Kochsiek et al. (Ed.): Internal medicine. 5th edition. Urban & Fischer-Verlag, Munich 2006, ISBN 3-437-44405-0 , p. 1117 ff.
- ↑ a b S. J. Spechler et al.: Overview of the treatment of achalasia. In: UpToDate. February 2008.
- ↑ TSE - transgastric stapled esophagofundostomy. Re-myotomy, TSE (cardiaplasty) and merendino surgery in the picture and comparison
- ↑ H. Inoue et al: Endoscopy . 2010.
- ↑ D. von Renteln, H. Inoue, H. Minami, YB Werner et al .: Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. In: Am J Gastroenterol. 107, 2012, pp. 411-417. Epub 2011 Nov 8.
- ↑ YB Werner, D. von Renteln, T. Noder et al .: Early adverse events of per-oral endoscopic myotomy. In: Gastrointest Endosc. 85, Apr 2017, pp. 708-718. Epub 2016 Sep 5.
- ^ YB Werner, G. Costamagna, LL Swanstöm et al .: Clinical response to peroral endoscopic myotomy in patients with idiopathic achalasia at a minimum follow-up of 2 years. In: Good. 65, 2016, pp. 899-906. Epub 2015 Apr 30.
- ^ Gerhard Klumbies: Psychotherapy in internal and general medicine. 5th revised edition. S. Hirzel, Leipzig a. a. 1988, ISBN 3-7401-0117-2 , DNB 881500100 , pp. 370-385.
- ^ JR Siewert, F. Harder, M. Rothmund: Practice of visceral surgery - gastroenterological surgery. 1st edition. Springer Verlag, 2002, ISBN 3-540-65950-1 , p. 293 ff.