Skin flora
All microorganisms , such as bacteria and fungi , are summarized as skin flora , which as commensals or mutuals form a natural component of the surface of healthy skin and which densely colonize it. The skin flora is part of the microbiome and contributes significantly to protecting the skin and the entire organism from pathogens .
The term skin flora comes from a time when bacteria and fungi were still regarded as plants and consequently as part of flora . Today the term skin microbiome is more appropriate (see microbiome ).
As long as the skin is intact as the border organ to the outside world and can thus fulfill its barrier function, these microorganisms do not disturb, do not make you sick and are useful for several reasons. So the commensals compete e.g. B. with foreign microorganisms around their "territory" : Before the foreign microorganism can settle on the skin, the resident placeholder must first have been displaced. Only pathogens that prevail against the local flora can multiply. In addition, the resident microorganisms of the skin flora produce metabolic products that have a beneficial effect on the functions of the skin.
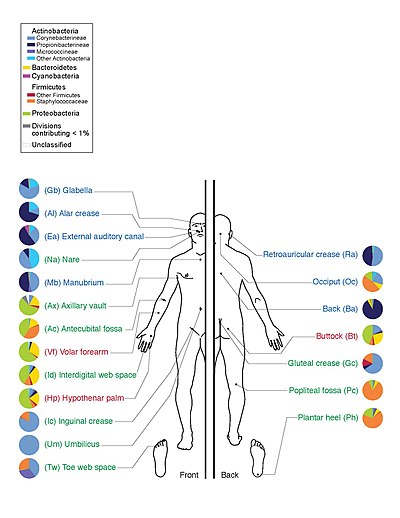
The individual skin regions have a very different composition of microorganisms. The hair follicles house the majority of the microorganisms, which u. a. is crucial for the development of skin diseases such as acne or folliculitis .
Components of the skin flora
Depending on the skin region, age, gender, genetic predisposition and environmental conditions, both the spectrum of germs and the number of microorganisms in the skin flora can be very different. A study by New York University, for example, which examined the microbes on the forearms of six people, found a total of 182 different types of bacteria from eight strains , although only four types were detectable on all six people. The ratio of anaerobic to aerobic species is comparatively balanced at 10: 1. The germ densities are, depending on the region, between 10 2 and 10 6 per cm². Approximate germ counts of different skin regions (germ count per cm²): fingertips 20 - 100, back 3 × 10 2 , feet 10 2 - 10 3 , forearm 10 2 - 5 × 10 3 , hand 10 3 , forehead 2 × 10 5 , scalp 10 6 , Armpit 2 × 10 6 . A total of around 10 10 bacteria live on our skin surface.
It is divided into resident and transient skin flora.
Resident flora
The resident flora or local flora is part of the physiological nature of the skin. The associated microorganisms are located in the stratum corneum of the horny layer and the ducts of sebum glands or hair follicles. As placeholders, they make the settlement of non-resident germs more difficult and in this way ensure so-called colonization resistance . Through their metabolic products , they maintain normal skin functions and also inhibit the growth of non-resident germs. However, if resident microorganisms get inside the body - e.g. For example, if the skin is not intact or as a result of invasive procedures - they can also cause infections.
Staphylococci ( S. epidermidis, S. saprophyticus, S. hominis, S. xylosus, S. warneri, S. haemolyticus, S. saccharolyticus, S. conii, S. auricularis ) preferentially colonize moist skin regions with poor sebum, such as intertriginous areas, hands and feet.
Corynebacteria ( C. minutissimum, C. jeikeium, C. xerosis, C. pseudotuberculosis, C. goutcheri, C. pseudodiphteriticum, C. bovis ) break down the fats formed by the sebum glands of the skin into fatty acids that are essential for the acidic environment on the skin are jointly responsible and thus again lead to an inhibition of germ growth.
Brevibacterium and Dermabacter cause, among other things, individual body odor.
Micrococci ( M. luteus , M. flavus ) are particularly detectable in children.
Other bacteria are non- pathogenic mycobacteria , Sarcinia spp. , Propionibacteria ( P. acnes, P. granulosum, P. avidum ), enterococci and acinetobacteria .
While the skin of the feet has a diverse fungal flora, all other areas of the skin are mainly inhabited by species of the genus Malassezia . If the sebum glands of a person produce too much sebum or if these sebum glands are blocked by sebum, the normally harmless yeast Pitysporum ovale is allowed to grow more rapidly , which leads to seborrheic dermatitis with itching and flaking. Dandruff can now be brought under control with suitable shampoos.
Colonization of the hair follicles
Here there are particularly high numbers of bacteria, predominantly lipophilic species. 20% of the entire skin flora is located in deep sections of the hair follicles. Staphylococci and Malassezia, including aerobic corynebacteria, and anaerobic, lipophilic bacteria (propionibacterium) below, settle near the surface. These microorganisms can not be eliminated even by disinfecting the skin ; they form the reservoir from which the skin flora is formed again within 24 to 72 hours after disinfection.
Hair follicle mite
Hair follicle mites like Demodex folliculorum live in the hair follicles of the skin. Hair follicle mites are passed on from person to person, mostly from mother to child, and colonize everyone, but also dogs and cats. The tiny mites eat fat, bacteria, but also cream residues and make-up. After two weeks of life on the skin, they return to their place of birth, the hair follicle, where they mate and lay eggs. The new mites migrate back to the surface of the skin with the growing hair. Their existence helps maintain balance on the skin. While they can cause mange in animals with compromised immune systems, negative effects are not known in humans and its partner Demodex folliculorum .
Transient colonization
The transient skin flora consists of microorganisms that temporarily colonize certain skin regions. This may also include pathogens that cause disease. You can come from the environment or from your own body - e.g. B. nasal secretions, intestinal bacteria - originate.
Staphylococcus aureus , E. coli , Klebsiella , Pseudomonas and Enterobacteriaceaen are more common on moist and warm skin regions (intertriginous areas). Further microorganisms of the transient germ colonization are aerobic gram-positive spore formers.
Hygienic hand disinfection can reduce the transient skin flora of the hands to such an extent that the spread or transmission of pathogens is largely prevented.
Influencing factors
Moisture, pH value and oxygen supply are very different depending on the skin area, and accordingly the distribution of the bacteria in the skin flora is not even.
Horny layer
Apart from those microorganisms that have specialized in the breakdown of keratin ( dermatophytes , trichophytes ), the range of nutrients on the skin surface is limited and therefore by no means ideal for all bacteria. The constant growth of the epidermis also prevents invasion , because the most densely populated cell layers ( stratum disjunctum of the stratum corneum ) are continuously shed.
Skin surface pH
It has long been known that the surface of the skin reacts acidic (Heuss 1882), later it was also referred to as the “ protective acid mantle of the skin” (Schade / Marchionini 1928). Numerous studies have been carried out on the skin surface pH value and for a long time the much-cited pH range of 5.4-5.9 was considered to be the normal value on the "forearm of a white, male, adult individual" (Braun-Falco / Korting 1986) . Two current studies have shown that the physiological pH value is just below 5 (Lambers et al. 2006; Segger et al. 2007). In addition, the pH is influenced by numerous factors, such as: B. Age, gender, skin area, cosmetics, etc.
The importance of the slightly acidic pH value has also been examined in numerous studies and it has been shown that it inhibits the growth of some pathogenic microorganisms (e.g. Propionibacterium acnes ), but the microorganisms of the normal flora (e.g. Staphylococcus epidermidis ) grow very well at a pH around 5. The “protective acid mantle” stabilizes the growth of non-pathogenic bacteria and inhibits that of pathogenic bacteria (Pillsbury / Rebell 1952; Korting et al. 1987, 1990 and 1992; Kurabayashi et al. 2002; Lambers et al. 2006).
In addition, many pH-dependent enzymes, which are involved in the development and regeneration of the epidermal permeability barrier (skin barrier), work very well due to the pH value of the skin surface . The slightly acidic skin pH value is therefore of decisive importance for the overall homeostasis of the skin.
dryness
Despite the sweat glands and transdermal fluid secretion (perspiratio insensibilis), the epidermis offers a very dry environment, which is a poor breeding ground. This corresponds to the significantly higher bacterial density in moist skin areas (intertrigines) such as armpits, spaces between fingers and toes, groin and anal folds.
Lipids, fatty acids
Free fatty acids , some of which are only formed through bacterial metabolism (lipophilic microorganisms, see below), have a bactericidal effect on many types of bacteria . A change in these milieu conditions also results in shifts in the germ density of the individual species and species. For example, the proportion of lipophilic species in the condition of the Seborrhoeae increases and the general germ count increases with increased perspiration (moisturizing otherwise dry skin).
Skin regions with special environmental properties
Seborrheic zones
Skin regions rich in sebum are particularly densely populated with lipophilic microorganisms, including: Corynebacteria , Propionibacteria and Malassezia furfur . The lipolytic metabolism of propionibacteria (including lecithinases) leads to the formation of free fatty acids, which in turn influence the rest of the colonization of the skin. In addition to these lipophilic microorganisms (predominantly propionibacteria), there are also plenty of coagulase-negative staphylococci and non-pathogenic mycobacteria . The seborrheic zones include: forehead, nasolabial fold , nose, neck, and shoulders.
Moist areas of the skin
Increased humidity leads to an increase in the germ density. In the intertriginous areas (spaces between fingers and toes, groin, armpit, anal folds), the germ counts are significantly larger than z. B. on the rather dry lower legs. The armpits are populated very differently, either coagulase-negative staphylococci predominate alongside a few corynebacteria or vice versa. Peptostreptococci settle in the sweat gland ducts , which often become the cause of sweat gland abscesses .
Between the toes: Pigment- forming Bacteroides species ( B. melaninogenicus , B. asaccharolyticus ) and Clostridium perfringens are regularly detectable. Intertriginous areas are relatively often colonized with (yeast) fungi.
Dry areas of the skin
For example the flexor side of the forearms: Overall low germ count. Coagulase-negative staphylococci predominate (10 2 - 10 3 CFU / cm²). Only a few corynebacteria and propionibacteria.
Determination of the number of germs on the skin (detergent washing method)
An area of skin of a defined size is covered with a certain volume of detergent solution. The microorganisms on the surface of the skin are dissolved by vigorous rubbing in the detergent and grown after being diluted.
swell
- Jörg Blech: Life on people . Rowohlt, Reinbek 2000; Revised new edition ibid. 2010, ISBN 978-3-499-62494-0
- Peter Brooke: Small monsters, The secret world of tiny living beings , Gondrom-Verlag, 1999, p. 32/33
Web links
Individual evidence
- ↑ Robert L. Dorit: Body Microbes - Before We Conquer Each Other To Death . In: Spectrum of Science. September 2008, pp. 62-66
- ^ A. Kramer, D. Gröschel, P. Heeg, V. Hingst, Hans Lippert , M. Rotter, W. Weuffen (eds.): Clinical antiseptics. Springer Verlag, Berlin 1993, p. 107; ISBN 978-3-642-77716-5 .
- ^ Christian Jassoy, Andreas Schwarzkopf: Hygiene, Infectology, Microbiology. 3rd edition, Georg Thieme Verlag, Stuttgart 2018, p. 40; ISBN 978-3-13-241368-9 .
- ↑ Keisha Findley, Julia Oh and a .: Topographic diversity of fungal and bacterial communities in human skin. In: Nature. 2013, S., doi : 10.1038 / nature12171 .
- ^ Christian Jassoy, Andreas Schwarzkopf: Hygiene, Infectology, Microbiology. 3rd edition, Georg Thieme Verlag, Stuttgart 2018, p. 195; ISBN 978-3-13-241368-9 .
- ↑ Axel Kramer: Hand hygiene - patient and staff protection. Review article, GMS Krankenhaushyg Interdiszip 2006; 1 (1): Doc14; accessed on December 20, 2019