Trigeminal neuralgia
| Classification according to ICD-10 | |
|---|---|
| G50.0 | Trigeminal neuralgia |
| IHS / ICHD-II code | 13.1 |
| ICD-10 online (WHO version 2019) | |
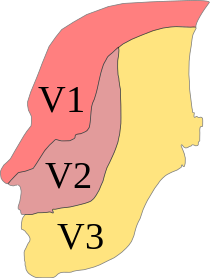
The trigeminal neuralgia (also tic douloureux , French tic , [nervous] twitching ' douloureux , painful') is a form of facial pain (facial neuralgia, facial neuralgia). It is an extremely painful irritation of the fifth cranial nerve , the trigeminal nerve , which consists of three nerve branches that supply the forehead area, the upper jaw and the lower jaw. The designation as tic douloureux indicates the reflex twitching of the facial muscles that occasionally accompanies the pain. This is to be distinguished from atypical facial pain and other facial pain.
to form
A distinction is a classic or idiopathic from a symptomatic trigeminal neuralgia: When idiopathic trigeminal neuralgia that the atypical facial pain triggers the cause is largely unknown in the symptomatic trigeminal neuralgia , however, a cause can be found. However, an anatomical correlate is often found in idiopathic trigeminal neuralgia - there is close contact between a vascular branch and a branch of the trigeminal nerve, so that this circumstance can be assumed to be the cause. For example, symptomatic trigeminal neuralgia can result from an inflammatory process, e.g. B. in multiple sclerosis ( MS ), or a brain tumor . This distinction is clinically relevant because the therapeutic approach is based on it, among other things.
Epidemiology
Idiopathic trigeminal neuralgia
First occurrence after the age of 40. The incidence for women is 5.9 per 100,000 people per year, and for men 3.9 per 100,000 people per year. The second ( maxillary nerve ) and third trigeminal nerve ( mandibular nerve ) are most frequently affected alone (18% and 15%) or combined (approx. 40%). Trigeminal neuralgia on both sides is rare at around 3%.
Symptomatic trigeminal neuralgia
First occurrence before the age of 40. The first branch of the trigeminal nerve ( ophthalmic nerve ) and bilateral nerve pain are much more common .
Symptoms
Characteristic is the spontaneous or triggered, lightning-like shooting pain in the area of one or more trigeminal branches (usually the second and third branch, rarely the first branch). The pain usually lasts for a few seconds, rarely up to two minutes. The pain attack can also be followed by vegetative symptoms in the supply area of the corresponding trigeminal branch, such as reddening or secretion of the lacrimal and / or salivary glands or the nose . These symptoms can, especially after a long and pronounced attack, speak against the presence of idiopathic trigeminal neuralgia in the differential diagnosis. The attacks occur several times a day for weeks, sometimes 3 to 4 times per minute, and for months; At the beginning, pain-free intervals lasting weeks to months are also possible.
The following can act as triggers: chewing, speaking, swallowing, brushing teeth, touching the face, cold drafts, movements of the facial muscles .
In idiopathic trigeminal neuralgia, there is no pain between the individual pain attacks, whereas in symptomatic trigeminal neuralgia, abnormal sensations or a dull feeling of pain can persist between the attacks. Symptomatic trigeminal neuralgia is more likely to involve the first branch of the trigeminal nerve and occur on both sides. These patients often have a sensory disorder in the supply area of the affected trigeminal branch.
Patients who have been troubled for years often develop avoidance behavior and, for example, no longer go outside (if cold air acts as a trigger), no longer wash or shave in the affected area of the face if even a slight touch acts as a trigger. Trigeminal neuralgia is often accompanied by a depressive mood . The suicide rate is significantly increased in those affected.
Strength of pain
The pain that occurs in trigeminal neuralgia, along with cluster headache, is one of the strongest pains imaginable for humans. They are often given the highest grade on a pain scale from 0 to 10.
Pathogenesis
In over 70% of patients, pathological vascular-nerve contact can be detected intraoperatively. In most cases, this is the contact between the superior cerebellar artery and the root of the trigeminal nerve in the area of the brain stem . The rhythmic expansion of the vessel results in a localized demyelination of the nerve. This does not mean that all persons with pathological vascular-nerve contact must have a vascular-related pain syndrome. In addition to this theory, there is the hypothesis of a functional disorder in the core area of the trigeminal nerve and the hypothesis of a disorder in the pain-processing system.
In symptomatic trigeminal neuralgia, for example, masses and demyelination processes in the context of multiple sclerosis lead to the typical pain.
Differential diagnoses
- atypical facial pain
- Odontogenic infection
- Glossopharyngeal neuralgia
- all forms of headache (especially trigeminal autonomic headache disorders )
- Craniomandibular Dysfunction
- Paratrigeminal Syndrome
- Trigeminal neuropathy (typical: permanent pain + sensory disturbances, no trigger effect, often after facial injuries)
therapy
There are conservative and operative therapy options. First, a conservative, i.e. drug-based therapy attempt will always be made, as all surgical interventions have (sometimes serious) side effects - not to mention the operability of the patient.
In the past, surgical measures were still frequently performed in the area of the facial skull because the pain was misinterpreted. It should therefore be noted at this point that removing teeth or rinsing the maxillary sinuses did not show any therapeutic success. Nevertheless, pathological changes in the tooth, mouth and jaw area must first be excluded or treated - also to rule out other causes. The effectiveness of psychotherapeutic methods could also not be proven.
Conservative therapy
- First choice drug: carbamazepine / oxcarbazepine
- Agent of choice for acute therapy: phenytoin (sodium channel blocker)
- In addition, there are a number of other drugs that have been proven in studies or empirically, such as baclofen as an additional therapy, lamotrigine , pregabalin and gabapentin . Levetiracetam may also have a therapeutic effect.
- Misoprostol is effective for treating trigeminal neuralgia in multiple sclerosis.
- Opiates are insufficiently effective and have not been investigated in long-term studies, which is why the 2001 expert group does not recommend their use.
Operative therapy
Various therapy options are also available here:
Procedure without opening the skull in / on the Gasseri ganglion
The damage to the ganglion gasseri caused by heat (temperature-controlled coagulation) by chemical substances (glycerol rhizolysis) and by mechanical pressure (balloon compression) is summarized here. All procedures are very effective with an early success rate of more than 90%. After ten years, the significant pain relief or freedom from pain is still 70 to 80%. As a side effect, sensory disturbances (possibly also painful) occur in the supply area of the trigeminal nerve and, in rare cases, meningitis (1 to 5%, depending on the therapy method).
Procedure for relieving the trigeminal nerve in the cerebellopontine angle
- See also: microvascular decompression
In the Jannetta operation, either a muscle cushion or foreign material is inserted between the trigeminal nerve and the compressing vessel. The early success rate of 98 percent proves the effectiveness (freedom from pain or significant pain relief). After 20 years, this success rate is still over 67 percent. In 11 percent of the cases, the operation had to be re-operated within six years, whereby the success rate after these re-operations was significantly lower than after the first operation (after five years only 51 percent). As a side effect, in 3 to 30 percent of cases there are sensory disturbances (mostly in the form of a decrease in feeling) in the trigeminal region and in up to 5 percent of cases there is deafness in the ear on the same side .
Radiotherapy treatment procedures
- See also: gamma knife , linear accelerator
The early success rate is around 86 percent, but drops to around 75 percent after just under three years. It is a relatively new therapy option, so long-term results have to be awaited.
literature
- H. Iro, F. Waldfahrer: Disturbed Trigeminal Sensitivity. In: Laryngo-Rhino-Otology. Stuttgart 84.2005, 179-193. ISSN 0935-8943 , doi: 10.1055 / s-2005-861141 .
Web links
- Guideline trigeminal neuralgia of the German Society for Neurology . In: AWMF online (as of 2012)
- Deutsches Ärzteblatt; Therapy options for trigeminal neuralgia - focus on surgical procedures (PDF)
Individual evidence
- ↑ K. Poeck, W. Hacke: Neurology . Springer-Verlag 2006, 12th edition. ISBN 3-540-29997-1
- ↑ S. Love, T. Gradidge, HB Coakham: Trigeminal neuralgia due to multiple sclerosis: ultra structural findings in trigeminal rhizotomy specimens. In: Neuropathology and applied neurobiology. Volume 27, Number 3, June 2001, pp. 238-244, ISSN 0305-1846 . PMID 11489143 .
- ↑ S. Katusic, CM Beard et al. a .: Incidence and clinical features of trigeminal neuralgia, Rochester, Minnesota, 1945-1984. In: Annals of neurology. Volume 27, Number 1, January 1990, pp. 89-95, ISSN 0364-5134 . doi: 10.1002 / ana.410270114 . PMID 2301931 .
- ^ A. Delitala, A. Brunori, F. Chiappetta: Microsurgical posterior fossa exploration for trigeminal neuralgia: a study on 48 cases. In: Minimally invasive neurosurgery: MIN. Volume 44, Number 3, September 2001, pp. 152-156, ISSN 0946-7211 . doi: 10.1055 / s-2001-18124 . PMID 11696884 .
- ^ G. Zorman, CB Wilson: Outcome following microsurgical vascular decompression or partial sensory rhizotomy in 125 cases of trigeminal neuralgia. In: Neurology. Volume 34, Number 10, October 1984, pp. 1362-1365, ISSN 0028-3878 . PMID 6541308 .
- ↑ S. Love, HB Coakham: Trigeminal neuralgia: pathology and pathogenesis. In: Brain: a journal of neurology. Volume 124, Pt 12 December 2001, pp. 2347-2360, ISSN 0006-8950 . PMID 11701590 . (Review).
- ↑ Guideline trigeminal neuralgia of the German Society for Neurology . In: AWMF online (as of 2012)
- ^ WH Sweet: Specific neural stimulation for inhibition of pain. In: Proceedings of the Australian Association of Neurologists. Volume 5, Number 3, 1968, pp. 459-461, ISSN 0084-7224 . PMID 4179480 .
- ↑ S. Håkanson: Trigeminal neuralgia Treated by the injection of glycerol into the trigeminal cistern. In: Neurosurgery. Volume 9, Number 6, December 1981, pp. 638-646, ISSN 0148-396X . PMID 7322329 .
- ^ S. Mullan, T. Lichtor: Percutaneous microcompression of the trigeminal ganglion for trigeminal neuralgia. In: Journal of neurosurgery. Volume 59, Number 6, December 1983, pp. 1007-1012, ISSN 0022-3085 . doi: 10.3171 / jns.1983.59.6.1007 . PMID 6631493 .
- ↑ HD Jho, LD Lunsford: Percutaneous retrogasserian glycerol rhizotomy. Current technique and results. In: Neurosurgery clinics of North America. Volume 8, Number 1, January 1997, pp. 63-74, ISSN 1042-3680 . PMID 9018706 .
- ^ DJ Skirving, NG Dan: A 20-year review of percutaneous balloon compression of the trigeminal ganglion. In: Journal of neurosurgery. Volume 94, Number 6, June 2001, pp. 913-917, ISSN 0022-3085 . doi: 10.3171 / jns.2001.94.6.0913 . PMID 11409519 .
- ^ D. Kondziolka: Gamma knife thalamotomy for disabling tremor. In: Archives of neurology. Volume 59, Number 10, October 2002, p. 1660; author reply 1662-1660; author reply 1664, ISSN 0003-9942 . PMID 12374506 .

