Defibrillation
The defibrillation ( lat. De , ab ', off' and English. Fibrillation , flicker ') is a method of treatment against the life-threatening cardiac arrhythmias ventricular fibrillation and ventricular flutter , where the normal heart activity to be restored by strong surges. The instrument used is called defibrillator or technical jargon Defi .
Indications
Defibrillation is used exclusively for resuscitation in ventricular fibrillation, ventricular flutter and pulseless ventricular tachycardia .
- Ventricular fibrillation (VF, ventricular fibrillation) means that all heart muscle cells tremble, but are incapable of coordinated action, due to a faulty generation of excitation in the heart. As a result, the heart can no longer pump, causing a circulatory arrest . The pulse can no longer be felt.
- Ventricular flutter shows the same pathological mechanism as fibrillation, but differs in the frequency of the flicker waves, whereby different values are given in the literature (from 280–350 / min).
- The ventricular tachycardia (VT) may be in a pulseless and a pulsatile be distinguished, wherein the pulseless VT represents an absolute indication for defibrillation. The pulsatile VT can be ended by means of cardioversion (a special form of defibrillation), provided that drug therapy remains ineffective. The VT shows even, rapid excitations that emanate from the ventricles and not, as usual, from the excitation center in the atrium .
In order for the heart to pump blood into the arteries, it needs to contract. In the situations described, the heart cannot or no longer fully contract due to the high frequency of excitation. As a result, the organs can no longer be supplied with blood. The arrhythmias described here are fatal if left untreated within minutes. Ventricular fibrillation is the most common fatal arrhythmia in adults. The respective diagnoses can be made with a simple 3-channel ECG . The defibrillator itself can serve as a monitor .
Causes of life-threatening cardiac arrhythmias can be, for example, a heart attack , but also electric shocks or drug and drug intoxication . If the heart shows no electrical activity at all, known as asystole or also as the zero line, or if the electrical activity does not cause any mechanical reaction of the heart (PEA - pulseless electrical activity , or EMD - electro-mechanical dissociation), defibrillation has no effect , would be time-consuming and can also damage the heart muscle tissue.
The aim in the context of cardiopulmonary resuscitation from ventricular fibrillation or pulseless ventricular tachycardia is an early defibrillation : The earlier an indexed defibrillation is done, the better the survival rate and prognosis of affected patients.
Contraindications
There are conditions under which defibrillation should not be performed.
Physiological reasons
- Existing pulse
- Hypothermic patients below 27 ° C core body temperature
- Asystole , pulseless electrical activity
- Safe death signs
Environmental reasons
- Direct skin contact between the patient and the helper
- Wet subsurface (wet bridge to the helper)
- Metallic contact between patient and helper
- Potentially explosive environment
Legal reasons
In some countries, patients can write legally binding advance directives. The purpose of these is to record in writing the will of the patient with regard to medical treatment in the event of his inability to consent. Often this also includes the will not to be resuscitated or defibrillated. However, due to time pressure, the lack of verifiability of personal details and the living will itself, these are normally not relevant in out-of- hospital emergency medicine . The situation is different for hospital patients whose identity has been clarified and whose living will is enclosed in their medical record .
Therapy principle
The activity of the heart muscle cells is controlled by electrical signals. In the case of shockable rhythm disturbances, the transmission of these stimuli is disturbed, so that disordered electrical signals are formed in the affected muscle tissue.
Ventricular fibrillation leads directly to a complete breakdown of the circulatory system, since an orderly and mechanically efficient contraction is not possible due to an electrical chaos of the heart. The only effective therapy is the delivery of an electrical current pulse, the defibrillation. It has been known for many years that this can stop ventricular fibrillation. The physiological principles according to which defibrillation works are only partially understood. Two different theories try to explain defibrillation: On the one hand, it is assumed that defibrillation of a sufficiently large amount of the myocardium - about 70% is assumed - intramyocardial 'barriers' from refractory myocardium arise. The fronts of the automatics run 'dead' on these. Another hypothesis assumes that defibrillation creates a borderline voltage gradient (around 6 V / cm). This leads to prolonged repolarization, at which the fronts of automatism break. Animal experiments suggest that the latter hypothesis is the more plausible one. An effective defibrillation of ventricular fibrillation is accordingly characterized by the fact that the shock discharge ends the circling excitation fronts and higher-level control centers of the heart rhythm resume their function. In the case of inefficient defibrillation, the shock ends ventricular fibrillation, but since automatisms continue to revolve around partially refractory myocardium, ventricular fibrillation is re-initiated.
Procedure in the context of resuscitation
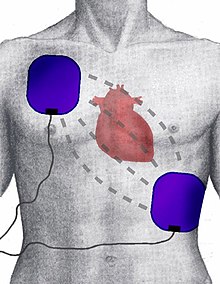
During defibrillation, the “paddles” (contacts) of the defibrillator are pressed onto the patient's chest. In order to reduce the contact resistance inside the body, they are coated beforehand with electrically conductive electrode gel. Alternatively, adhesive electrodes that can only be used once are applied to the chest, which is also the case with automated external defibrillators ( AED ). The position of the electrodes is chosen so that the current flows between them through the heart. Even with optimal positioning, only about four percent of the energy reaches the heart muscle due to the resistance of skin and tissue.
In adults, the basic resuscitation measures are carried out until the defibrillator arrives . This is followed by defibrillation with an energy of 360 joules (monophasic) and, for biphasic devices, depending on the manufacturer's specifications. Immediately thereafter, chest compressions and ventilation are continued for two minutes, after which the circulatory function and pulse are checked.
Every shock causes burn-like tissue damage. In addition, in almost all cases the likelihood of a successful resuscitation drops massively if the patient has already been defibrillated several times without success, which is also a sign of a long resuscitation period. Exceptions are hypothermic and poisoned patients.
In between defibrillation attempts, the patient is usually intubated and drugs are administered to increase heart strength .
In the event of cardiac arrest with no visible electrical activity ( asystole ), an adrenaline preparation is given; If the heart rhythm is very slow ( bradycardia ), an attempt is made to stimulate heart muscle contractions using an external pacemaker . Defibrillation is pointless in this situation.
hazards
If defibrillation is accidentally performed with a normal heart rhythm (e.g. unconsciousness from another cause), this can trigger ventricular fibrillation. Devices that are intended for operation by medical laypersons therefore independently check the patient's heart rhythm and, if necessary, prevent the delivery of a current surge.
In addition, during defibrillation it is important that the assistants are not connected to the patient in a conductive manner (e.g. by touching the patient), as otherwise they could get some of the energy.
equipment

There are both manual and semi-automatic defibrillators. These devices are mainly used in the rescue service and in hospitals . They often have additional functions such as an EKG , measuring the oxygen saturation of the blood or blood pressure .
AEDs (automated external defibrillators) are increasingly being placed in public squares and places with high traffic in order to reduce the duration of cardiac arrest in the event of ventricular fibrillation as much as possible.
Procedure
A distinction is made between monophasic and biphasic defibrillation; the monophasic was developed around 1960, the biphasic was developed by a Russian scientist around 1990 and represents the more modern method. The biphasic defibrillation uses significantly lower energies, since the impedance of the chest is determined first. If the impedance is low, Ohm's law requires a lower voltage to generate the necessary electrical power. Only in " high-resistance " patients (e.g. obese or dehydrated patients) does the voltage have to be increased in order to bring the required power (and thus the energy) to the heart muscle. Why biphasic devices work more efficiently than monophasic devices is still being investigated. It is assumed that the heart muscle can store a certain amount of electrical energy, which can then lead to refibrillation (renewed fibrillation). Due to the negative part in the biphase, this energy is "drawn off" and an orderly chamber excitation is possible again.
Monophasic excitation
With monophasic defibrillation, the electrical current between the paddles only flows in one direction, the impulse has only one phase.
Biphasic stimulation
This is different with biphasic defibrillation: Here the polarity of the current pulses is different. First of all, the defibrillator conducts a small measuring current from one electrode through the patient to the other electrode via the paddles. This first current flow is used to measure the complex resistance of the chest, its impedance . Depending on the measured impedance, the device sets the appropriate voltage for defibrillation: a low one because of the lower resistance, for example in slim people, or a higher voltage, for example in obese people. Set in this way, the actual shock takes the form of a current surge with the selected strength. The pulse is emitted in two parts, which differ in their polarity; in other words, the paddles are switched once during the pulse delivery.
Although it has been known for many years that defibrillation can stop ventricular fibrillation, the optimal amount of energy is still unclear. A study by Weaver and co-workers in 1982 showed that shocks with 175 J and 320 J are basically equally effective. However, the same study showed that the higher the shock energy, the higher the frequency of higher-grade AV blocks. The algorithms commonly used for monophasic defibrillation thus reflect a compromise that has not yet been verified. Ultimately, it must be stated that the optimal energy for a monophasic shock to terminate ventricular fibrillation is not known.
Data comparing monophasic and biphasic shocks are sparse. The largest group was examined in the ORCA study. There it was shown that a biphasic 150 J shock could end with 96% ventricular fibrillation, whereas a monophasic 200 J shock was only effective in 59%. This difference was significant; also the differences for the second (64% versus 96%) and third shock (69% versus 98%). The rate of surviving patients in the two groups was not significantly different, but the proportion of patients with minor cerebral damage after successful resuscitation was better in the group of patients treated with biphasic defibrillators.
Similar applications
Electrical cardioversion is related to defibrillation . Here, too, the heart is depolarized with an electric shock, but in order to end other cardiac arrhythmias. In contrast to defibrillation, the shock is only delivered automatically in a certain phase of the cardiac cycle (synchronized with the R-wave in the ECG ) in order to avoid the development of ventricular fibrillation.
Both defibrillation and cardioversion are very painful and should not be performed while the patient is awake. During defibrillation (effective cardiac arrest) the patient is deeply unconscious anyway, but for cardioversion the patient is usually put under brief anesthesia .
Individual evidence
- ↑ Harald Genzwürker, Jochen Hinkebein: Case book anesthesia, intensive care medicine and emergency medicine. Georg Thieme, Stuttgart / New York 2005, ISBN 3-13-139311-4 , pp. 200 and 202.
- ↑ Walied Abdulla: Interdisciplinary Intensive Care Medicine. Urban & Fischer, Munich a. a. 1999, ISBN 3-437-41410-0 , pp. 4-22 ( cardiopulmonary resuscitation ), here: p. 5.
- ↑ Defibrillators from ZOLL. In: Zoll.com. Retrieved March 15, 2017 .
- ↑ V. Lischke, HJ Wilke, P. Kessler, C. Byhahn, K. Westphal: Zur Technik der biphasic and monophasic Defibrillation, Comparison of Biphasic and Monophasic Defibrillation. Georg Thieme Verlag Stuttgart / New York. In: Notarzt , 1999, 15 (6), pp. 149–152, doi: 10.1055 / s-1999-10872
- ^ WD Weaver, LA Cobb, MK Copass et al .: Ventricular defibrillation - a comparative trial using 175-J and 320-J shocks. In: New England Journal of Medicine. Volume 307, 1982. pp. 1101-1106.
- ^ T. Schneider, PR Martens, H. Paschen, M. Kuisma, B. Wolcke, BE Gliner, JK Russell, WD Weaver, L. Bossaert, D. Chamberlain: Multicenter, randomized, controlled trial of 150-J biphasic shocks compared with 200- to 360-J monophasic shocks in the resuscitation of out-of-hospital cardiac arrest victims. Optimized Response to Cardiac Arrest (ORCA) Investigators. Circulation. 2000 Oct 10. Volume 102 (15). Pp. 1780-1787.