Periodontal status
The periodontal status (from ancient Greek παρά para , German 'next to' , ancient Greek ὀδούς , Gen. ὀδόντος odontos , German 'tooth' and Latin status 'condition') is understood in dentistry to mean the assessment of the periodontics (tooth support apparatus). The survey includes obligatory (mandatory) and optional (optional) findings to be collected, i.e. those findings that are absolutely necessary and those that do not necessarily have to be collected. The mandatory entries correspond to the minimum requirements of the statutory health insurances in Germany for the approval of the application for assumption of the costs in which the findings are to be entered. Numerous other forms are also offered to record the findings. Practice administration software contains appropriate programs for entering and visualizing the findings. Hellwege recommends using the term periodontitis risk protocol for patients instead of the specialist term periodontal status , which is intended to increase awareness of the pathological findings.
Anatomical basics
The tooth-holding apparatus consists of the gums ( gingiva propria ), the tooth cement ( cementum ), the tooth socket ( alveolus ), the periodontal membrane ( periodontium or periodontium ) and the Sharpey fibers . These connective tissue fibers of the tooth holding apparatus connect the cement of the tooth with the tooth socket.
Assessment
While the periodontal screening index (PSI) provides an overview of the need for treatment, the periodontal status documents all findings on each tooth. The survey consists of four parts, the survey of the general and specific medical history, the clinical examination, the radiological diagnosis and the laboratory diagnosis.
General and special medical history
First, a documentation of previous is tooth loss , tooth migration , risk diseases such as smoking or diabetes , blood diseases , HIV , genetic disorders , and previous periodontal disease treatments being held.
Clinical examination
The periodontal assessment includes first of all the determination of the dentition findings, in this case the determination of the existing teeth, their sensitivity (vitality test), existing caries , existing fillings and integrated dentures and the influence of restoration margins on periodontal health, for example protruding filling or crown margins . Furthermore, ground facets are recorded as an indication of bruxism .
The gingiva is then inspected . Changes in color (e.g. reddening), texture (e.g. glassy, shiny, or ulcerated) and tissue tone (e.g. oedematous ) indicate pathological changes in the marginal gingiva. In addition, any pocket secretions can be determined, for example in the form of a discharge of secretion from the sulcus, or abscesses and fistulas can be determined. The assessment of the gingival inflammation takes place with the survey of the plaque index according to Silness and Löe and the gingivitis index according to Löe. To assess periodontal attachment loss, pocket probes are carried out using a calibrated periodontal probe and gingival recessions and gingival hyperplasia are determined . The periodontal attachment loss results from this information. Finally, studies of furcation infestation and tooth mobility also provide conclusions about the degree of periodontal disease.
Laboratory diagnostics
In the case of progressive periodontal diseases and cases with a difficult prognosis, laboratory diagnostics can be carried out, such as tests to identify the causative periodontal pathogenic microorganisms. There is also molecular biological evidence of bacterial DNA / RNA and immunological detection methods.
X-ray diagnostics
A panoramic slice image or an X-ray status is made to collect an X -ray finding. Reference points such as the enamel-cement boundary, the limbus alveolaris , the physiological bone boundary , the periodontal gap and the lamina dura are used to assess the X-ray images . In the healthy periodontium, the alveolar limbus runs apically approx. Two millimeters and parallel to the enamel-cement junction. An apical displacement of the limbus alveolaris is a sign of a loss of the alveolar bone.
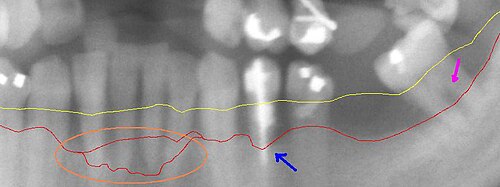
| Detail from a panoramic x-ray of advanced periodontitis in the left lower jaw with bone loss between 30% and 80%. The red line shows the current bone progression, which is transferred to the periodontal status. The yellow line shows the original course of the gingival margin, which runs about 1 to 2 mm above the limbus alveolaris . The pink arrow on the right shows an exposed bifurcation. The blue arrow in the middle points to particularly severe bone loss. The circled area shows a particularly aggressive course of periodontitis in the area of the lower front teeth. |
Completion instructions
- Teeth not clinically present are marked with horizontal lines. Teeth that need to be extracted (removed) are crossed.
- The results of the measurement of the pocket depths, which are determined on at least two opposing tooth surfaces, are drawn in millimeters in the fields of the tooth crown.
- The degree of mobility is noted in Roman numerals in the center of the tooth crown.
- Detected exposed furcations are drawn in the furcation area by means of a black point.
- An optional entry of the vestibular recession depth (in millimeters) is entered on the tooth root.
- Devital teeth are marked with a negative line above the root.
- An optional entry of the gingival course can be drawn in.
- For the individual periodontium, it is entered whether an open or closed procedure is planned.
See also
literature
Rudolf W. Ott: Clinic and Practice Guide Dentistry . Georg Thieme Verlag, 2003, ISBN 978-3-13-131781-0 , p. 220 ff.
Web links
- Example of a surveyed periodontal status , Spitta-Verlag. Retrieved December 21, 2015.
Individual evidence
- ↑ Klaus-Dieter Hellwege: The practice of professional tooth cleaning & ultrasonic scaling: instructions for the dentist and his team . Georg Thieme Verlag, 2007, ISBN 978-3-13-131283-9 , p. 41.
- ^ W. Ott, Anatomy and Histology of the Parodontium , Clinic and Practice Guide Dental Medicine, Thieme Verlag, Stuttgart, 1st edition: (2002) ISBN 3-13-131781-7 .
- ^ The Parodontal Screening Index (PSI) , Working Group Dental Health (AGZ-RNK).
- ↑ Mohammad Amiri Jetzeh: The influence of restoration margins on periodontal health - an overview . (PDF) In: Schweiz Monatsschr Zahnmed , 116, 2006, pp. 606–613; Retrieved December 20, 2015.
- ↑ H. Loe, J. Silness: Periodental disease in pregnancy. In: Acta odontologica Scandinavica. Volume 21, December 1963, pp. 533-551, PMID 14121956 .
- ↑ H. Loe: The gingival index, the plaque index and the retention index system. In: Journal of periodontology. Volume 38, Number 6, 1967 Nov-Dec, S. Suppl: 610-Suppl: 616, doi: 10.1902 / jop.1967.38.6.610 , PMID 5237684 .
- ^ Rainer Buchmann: Patient-friendly periodontology . Georg Thieme Verlag, November 24, 2010, ISBN 978-3-13-162431-4 , p. 51.



