Primary sclerosing cholangitis
| Classification according to ICD-10 | |
|---|---|
| K83.0 | Cholangitis, primarily sclerosing |
| ICD-10 online (WHO version 2019) | |
The primary sclerosing cholangitis ( PSC ) is a chronic inflammation of the bile ducts ( cholangitis ) inside and / or outside the liver. It leads to scarred hardening ( sclerosis ) and, associated with it, to a narrowing of the biliary tract.
Disease emergence
The exact mechanism of its formation is still unclear. The disease occurs particularly frequently (in 85% of patients) in connection with chronic inflammatory bowel disease , especially with ulcerative colitis . Men are affected significantly more often than women.
Clinical manifestations
| Symptoms | frequency |
|---|---|
| Weight loss | 25–80% after many years |
| Jaundice | 25-70% |
| itching | 10-70% |
| Upper abdominal discomfort | 50-70% |
| Fatigue, poor performance | |
| fever | |
| Diarrhea |
It should be noted that 35% of all patients are symptom-free.
Investigation methods
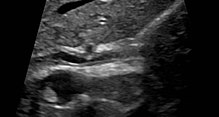
The clearest method is to visualize the biliary tract using ERC (endoscopic retrograde cholangiography) . Because of the relatively high rate of complications, however, the imaging method of choice today is MRCP (magnetic resonance cholangiopancreatography) . Also autoantibodies , called pANCA (perinuclear antineutrophil cytoplasmic antibodies) can be typically detected but they will contact the patients only at 70%.
Typical laboratory results
As with all diseases in which the outflow of bile from the liver cannot be guaranteed, the congestion parameters in the blood are increased. The autoantibody p- ANCA is found in about 70% of the cases . Patients with an increased value of the tumor marker CA 19-9 have a faster progressive course.
histology
There are focal periductal inflammatory infiltrates from lymphocytes , granulocytes and plasma cells . A progressive fibrosis ("onion skin-like") of the bile ducts develops , which turns into duct atrophy and leads to the bile ducts being replaced by fibrous strands. This results in the proximal biliary obstruction with the appearance of biliary duct dilatations.
course
PSC is a progressive disease that occurs in bursts. Patients notice a deterioration in their general condition and an increase in the above symptoms. It is particularly problematic that gallstones can form, which then lead to an additional increase in symptoms. Since PSC is an inflammatory disease, there is also the possibility that the bile duct mucosa may degenerate. Bile duct carcinoma was mentioned here particularly frequently . It is thought to develop in 5–10% of PSC patients.
therapy
The therapy of choice is ursodeoxycholic acid (UDC). It lowers the elevated liver values, v. a. AP and GGT . In addition, the itching is significantly reduced. In addition, if gallstones or biliary constrictions have formed, these must be removed, possibly as part of the ERCP performed for diagnosis . A regression of the structures of the liver that have already been rebuilt by connective tissue cannot be achieved with UDC; the drug has no influence on fibrosis. Therapy must be lifelong. In addition to the basic therapeutic UDC, other drugs are also available. Colestyramine and colestipol work similarly, if not as efficiently, as UDC.
The dominant problem in the long-term course of PSC is recurrent inflammation of the biliary tract, sometimes with severe attacks and courses that lead to a significant reduction in quality of life. These must be treated with antibiotics and also with antifungal agents, i. H. with drugs against bacteria and fungi. The latter become the leading problem, especially in the long term. For this reason, the guidelines of the German Medical Association were changed to allow these patients a transplant under the conditions of the MELD score . In addition, with the length of the disease, there is a significantly increased risk of developing biliary tract carcinoma , which as a rule cannot be diagnosed under the condition and usually only by the pathologist when processing the tissue of the liver removed as part of a liver transplant be diagnosed. In accordance with the guidelines of the German Medical Association, regular control and monitoring of the course is recommended. The liver transplant is the definitive and curative cure.
According to the data of a long-term study in Heidelberg, an annual ERCP and balloon dilatation of dominant stenoses can extend the time to terminal liver failure. Dominant stenoses are bile duct narrowings to <1.5 mm in the common hepatic duct or <1.0 mm in the dexter or sinist hepatic duct. In the study, one group was only dilated if the symptoms were appropriate. The second group received an annual ERCP and a dilatation of all dominant stenoses regardless of the symptoms. Survival without transplantation with annual ERCP and balloon dilatation was a median of 17.8 years, with dilatation only with symptoms (pruritus, jaundice or acute bacterial cholangitis ) only 11.1 years.
A guideline on diagnosis and therapy of PSC based on published scientific data and experience was published in 2017.
forecast
The median survival time without liver transplantation is around 10-20 years. A cure is currently not possible.
The 5-year survival rate after liver transplantation is 75–85%, but here (just as with PBC ) the disease in the transplant can recur in 20%.
The prognosis is primarily determined by the occurrence of frequently recurring attacks of inflammation associated with an increased risk of developing biliary tract cancer. The aim of therapy must therefore be to delay the progression of the disease as much as possible.
See also
literature
- Werner Böker, H. Denk, Ph. U. Heitz, H. Moch: Pathology . 4th edition. Urban & Fischer, Elsevier, 2008, ISBN 978-3-437-42382-6 .
- Roche Lexicon Medicine. 5th edition.
- Basic textbook internal medicine. Elsevier, 2006.
- Herbert Renz-Polster, Steffen Krautzig, Jörg Braun: Basic textbook internal medicine . 4th edition. Urban & Fischer Verlag, Elsevier, 2008, ISBN 3-437-41053-9 .
- J. Worthington, R. Chapman: Primary sclerosing cholangitis. In: Orphanet J Rare Dis. 2006 Oct 24; 1, p. 41. PMID 17062136 , PMC 1636629 (free full text)
- IL Steele, C. Levy, KD Lindor: Primary sclerosing cholangitis - approach to diagnosis. In: MedGenMed. 2007 Apr 25; 9 (2), p. 20. PMID 17955076 , PMC 1994832 (free full text)
- A. Michaels, C. Levy: The medical management of primary sclerosing cholangitis. In: Medscape J Med. 2008 Mar 12; 10 (3), p. 61. PMID 18449341 , PMC 2329756 (free full text)
- H. Lutz et al .: Primary sclerosing cholangitis: diagnosis and therapy . In: Deutsches Ärzteblatt Int . No. 10 (51-52) , 2013, pp. 867-874 ( review ).
Individual evidence
- ↑ a b B. Nashan et al .: Biliary malignancies in primary sclerosing cholangitis: timing for liver transplantation. In: Hepatology . 1996 May; 23 (5), pp. 1105-1111. PMID 8621141 .
- ↑ Guidelines for waiting lists and organ placement for liver transplantation, 2012 ( Memento of July 6, 2012 in the Internet Archive ) (PDF; 213 kB) bundesaerztekammer.de
- ↑ Christian Rupp, Theresa Hippchen, Thomas Bruckner, Petra Klöters-Plachky, Anja Schaible, Ronald Koschny, Adolf Stiehl, Daniel Nils Gotthardt, Peter Sauer: Effect of scheduled endoscopic dilatation of dominant strictures on outcome in patients with primary sclerosing cholangitis . In: BMJ (Ed.): GUT . August 17, 2019, p. epub ahead of print: [17.08.2019] ., doi : 10.1136 / gutjnl-2018-316801 .
- ↑ C. Strassburg, C. Schramm et al: S2k guideline autoimmune liver diseases. (PDF; 1.1 MB) Retrieved October 21, 2017 .
- ↑ a b Gerd Herold: Internal medicine: a lecture-oriented presentation . Herold, Cologne 2012, ISBN 978-3-9814660-1-0 .
- ↑ Herbert Renz-Polster, Steffen Krautzig, Jörg Braun: Basic textbook internal medicine with StudentConsult access: compact-tangible-understandable . 4th edition. Urban & Fischer Verlag, Elsevier, 2008, ISBN 3-437-41053-9 .
- ↑ Guidelines for waiting lists and organ placement for liver transplantation, 2013. (PDF; 213 kB) bundesaerztekammer.de