Thoracic outlet syndrome
| Classification according to ICD-10 | |
|---|---|
| G54.0 | Lesions of the brachial plexus, including thoracic outlet syndrome |
| ICD-10 online (WHO version 2019) | |
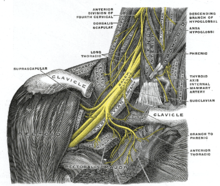
The thoracic outlet syndrome ( TOS ), also known as bottleneck syndrome thoracic or compression syndrome shoulder girdle will be referred to, is a neurovascular compression syndrome . This disease involves temporary or permanent compression of a vascular nerve bundle consisting of the brachial plexus , the subclavian artery, and the subclavian vein . This vascular nerve bundle runs from the neck towards the upper extremity and has to overcome three narrow points:
- the anterior or posterior scalene gap ,
- the costoclavicular space (space between the first rib and collarbone ) and
- the coracopectoral space (space between the coracoid process and the pectoralis minor muscle ).
Depending on the cause and the localization of the bottleneck, the clinical picture is characterized by circulatory disorders as well as sensory disorders and paralysis of the arm, which usually occur in the initial stage depending on the position.
Basics
The brachial plexus is a plexus of nerves that is formed by the anterior (ventral) branches of the spinal nerves C5 to C8 and TH1. From the brachial plexus emerge the nerves that supply the entire upper extremity with motor and sensitivity . The brachial plexus located in the depth of the lateral neck triangle and is formed after passing through the rear scalene that the anterior scalene muscle , middle scalene and the first rib is formed. In addition to the nerve fibers, the subclavian artery also passes through the posterior scalene gap. It supplies the upper extremity with oxygenated blood. The subclavian vein, which drains the oxygen-depleted blood from the upper extremity, runs through the so-called anterior scalene gap, which is located between the anterior scalenus muscle and the sternocleidomastoid muscle . After passing through the gaps in the scalenus, the nerve fibers of the brachial plexus as well as the arteria and subclavian vein unite to form a common neurovascular bundle that pulls towards the upper extremity and has to pass through two further narrow points. The costoclavicular gap lies between the first rib (Latin Costa) and the collarbone (Latin clavicula), the coracopectoral space between the coracoid process of the shoulder blade and the pectoralis minor muscle .
Forms and causes
The three constrictions to be passed by the vascular nerve trunk are the predispositions for the occurrence of a thoracic outlet syndrome.
The compression in the area of the gaps in the scalenus is also known as the scalene syndrome . It can occur through the presence of a cervical rib , which occurs only very rarely in humans, through exostoses or a steep position of the first rib, as well as through an enlargement ( hypertrophy ) of the scalene muscles. Muscle hypertrophy primarily affects the anterior scalenus muscle and is therefore also known as the anterior scalene syndrome . Thoracic outlet syndrome caused by a rib in the neck is also known as a rib cervical syndrome .
Compression in the area of the costoclavicular space leads to what is known as the costoclavicular syndrome , which occurs primarily after clavicle fractures as a result of excessive callus formation or is caused by functional compression during abduction , i.e. the arm spreading apart.
Compression of the vascular nerve bundle in the coracopectoral space is called hyperabduction syndrome or pectoralis minor syndrome . It occurs primarily as a result of hypertrophy of the pectoralis minor muscle.
In very rare cases, a Pancoast tumor can also trigger a thoracic outlet syndrome.
There are also some special forms of the thoracic outlet syndrome. If the compression of the vascular nerve bundle consists mainly of a narrowing of the subclavian vein, this is also referred to as thoracic inlet syndrome . Venous outflow disorders result. A venous outflow disorder increases the risk of thrombosis , that is, the formation of blood clots. A thrombosis in the subclavian vein leads to what is known as Paget-von-Schroetter syndrome .
Diagnosis
A suspected diagnosis can usually be made based on the description of typical complaints in the context of the patient survey ( anamnesis ). The symptoms of the clinical picture can often be triggered or intensified in those affected with the help of so-called provocation tests. These include the final fist test , the Adson test and the "Elevated arm stress test". The diagnosis also includes X-rays of the thorax and the cervical spine. This means that bony structures such as a cervical rib and exostosis of the first rib can be detected or excluded as possible causes. By determining the nerve conduction velocity using electroneurography , damage to the nerves supplying the arm can be detected. The method of choice for confirming the diagnosis is the representation and measurement of the blood flow in different positions of the arm and head by means of duplex sonography . This examination is also known as dynamic arm angiography .
therapy
In the treatment of Throracic outlet syndrome can conservative of operational distinguish measures. The conservative branch of therapy is chosen for milder symptoms and consists mainly of physiotherapeutic measures. These include manual grips, active exercises to strengthen the shoulder girdle muscles , massages and the use of heat to loosen up the muscles.
Surgical measures are indicated if the symptoms are pronounced and are aimed at eliminating the constriction, for example the removal of an existing cervical rib or the first rib in the scalene syndrome. The operation is also followed by physiotherapeutic measures.
literature
- S2 guideline Thoracic Outlet Syndrome of the German Society for Vascular Surgery. In: AWMF online (as of August 2008)
- Henne-Bruns, Dürig, Kremer: Dual series surgery. Thieme, 3rd edition, Stuttgart 2008, ISBN 978-3-13-125293-7 .
- Heinz-Walter Delank, Walter Gehlen. Neurology Thieme, Stuttgart 2004, ISBN 3-13-129780-8 .
- G. Koknel Talu: Thoracic outlet syndrome. In: Agri. Volume 17, Number 2, April 2005, pp. 5-9, ISSN 1300-0012 . PMID 15977087 . (Review).
- HC Urschel, MA Razzuk: Neurovascular compression in the thoracic outlet: changing management over 50 years. In: Annals of Surgery . Volume 228, Number 4, October 1998, pp. 609-617, ISSN 0003-4932 . PMID 9790350 . PMC 1191545 (free full text). (Review).