Distal radius fracture
| Classification according to ICD-10 | |
|---|---|
| S52.5 | Distal fracture of the radius |
| ICD-10 online (WHO version 2019) | |
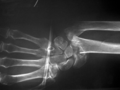
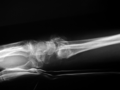
The distal radius fracture or the fracture of the radius near the wrist is the most common fracture in humans and accounts for up to 25% of all bone fractures, especially in children and in old age. Depending on the course of the accident , there is most often a kink (axis deviation ) to the extensor side (dorsal, Colles fracture ), less often to the flexor side (ventral / palmar, Smith fracture ). Occasionally other forms of fracture also occur, and the neighboring ulna is also often broken.
etiology
The radius shows a zone of less stability 2 cm proximal to the wrist with the metaphysis (locus minoris resistentiae). The stability of this zone is significantly influenced by systemic diseases. So it is by osteoporosis and thinning cortex (cortical bone) to decreased stability and a significant increase related to the distal radius fractures over the age of 60th
In the event of excessive force being exerted by a fall or impact, the maximum load limit will be exceeded. The so-called "Fractura radii in loco typico" occurs. The usual course of accident is a fall that is caught by hand. If the hand is overstretched (dorsally extended, usual posture when supporting), the extension type occurs, the more common Colles fracture. If the fall occurs on the palmarly flexed hand (bent towards the palm), a fracture of the flexion type, the Smith fracture, occurs. If the distal radius fragment is dislocated dorsally (towards the back of the hand), a fourchette position (French: fork) results; if the distal radius fragment is dislocated to the palmar and radial direction (towards the thumb side), a bayonet position results.
clinic
The main symptoms are pain and restricted functionality. Typically there is a painful swelling, widening of the wrist, a hematoma and painful limitation of mobility. Occasionally there is a feeling of instability.
diagnosis
The diagnosis is made with X-rays in two planes. Attention should be paid to accompanying injuries such as a fracture of the ulna, an avulsion fracture of the ulna styloid process and ligament injuries, especially the scapholunal (SL) ligament.
During the clinical examination, nerve lesions, vascular injuries and skin injuries must be specifically searched for, including palpation of the pulses of the radial and ulnar arteries , checking of capillary filling, finger function, thumb extensor vision and sensitivity. If vascular lesions are suspected, Doppler sonography and angiography can be used.
The question of the stability of the bone fracture is particularly important for the therapy decision. Radiological instability criteria have been established for this:
- Bone defect / debris zone
- Dorsal tilting primarily of> 20 °
- Volar tilting of the distal fragment
- dorsal or volar edge fragments
- Elbow feed of over 0.75 mm
- Avulsion of the ulna styloid process
- Step formation in the joint
In accordance with the recommendations of the Norwegian Society of Orthopedics, only the following criteria have been proven with sufficient evidence:
- Dorsal tilting of the distal radius ≥ 10 °
- Intra-articular step formation or diastasis ≥ 2 mm
- Ulnar advancement of ≥ 3 mm
- Incongruence of the distal radioulnar joint
- Debris zone / cortex loss of the distal radius
If one or more of the criteria mentioned apply to a primary X-ray, surgical treatment should be considered in adults ≥ 18 years of age.
Classification of distal radius fractures
| Surname | Type | Explanation |
|---|---|---|
| Colles fracture | Extension fracture (extension) | With around 25% of all fractures, it is the most common fracture in humans. |
| Smith fracture | Flexion fracture (flexion) | |
| Chauffeur fracture | intra-articular fracture | The stylus process breaks off at the distal radius |
| Barton fracture | intra-articular fracture | The dorsal edge of the distal radius is affected, sometimes with dislocation of the radio-carpal joint. |
| reverse barton fracture | intra-articular fracture | The palmar edge of the distal radius is affected. |
| Galeazzi fracture | distal radial shaft fracture | Simultaneous dislocation of the distal ulnar head |
AO classification
A common classification of distal radius fractures is, as with all bone fractures, the AO classification of the Association for Osteosynthesis Issues. The A fractures are located outside the joint (extra-articular) and can be further subdivided into types A1, A2 and A3. According to the AO classification, B fractures are partially intra-articular, i.e. that is, they partially affect the articular surface. Type C fractures are located in the joint itself (intra-articular). Different degrees of severity are assigned the numbers 1 to 3 in ascending order after the letters A, B and C.
treatment
Treatment of a simple radius fracture with no joint involvement depends on the degree of displacement and instability in the fracture area. Without shifting the ends of the fracture, a simple immobilization (retention) with a plaster cast takes place for approx. Six weeks; in the case of simple shifts (dislocation), first a device (reposition) and then the immobilization in a plaster cast.
If the fracture is unstable, i.e. it tends to shift again (secondary dislocation; often with smooth and transverse fractures), or if the establishment is unsuccessful or not possible due to its size, treatment is performed surgically.
Was for many years the Kirschner wire - osteosynthesis the standard method with introduction of wires in fracture anesthesia , plexus or general anesthesia in the art for Willenegger or Kapandji . Recently, plate osteosynthesis has increasingly established itself as the standard.
The procedure with drill wires is a closed procedure, so the break does not have to be exposed by a cut. With plate osteosynthesis, the skin is usually opened from the flexor side (volar) and the fracture is then opened again and fixed with the plate and screws. After a closed treatment with drill wires, a plaster of paris is usually also applied for four to six weeks. In the case of open fracture treatment with plate osteosynthesis, an additional plaster of paris can usually be dispensed with immediately, so that you can then quickly start exercising the wrist.
The flexion-side T-plate osteosynthesis procedure has become more and more popular in recent years and is being used more and more frequently for unstable fractures, complex fractures or those with joint involvement. This is mainly due to the fact that the displaced fracture fragments can be set up safely and precisely, even if comparative studies only show a slightly better result compared to the drill wire treatment and this is significantly more cost-effective. An English study found total costs of a mean £ 3,800 for the spike wire treatment and £ 4,400 for the plate fixation, which resulted in costs of £ 89,000 per quality-corrected life-year ( QALY ) gained due to the minimally better results .
In summary, depending on the type of fracture, the treatment can either be conservative in plaster of paris, surgically with plaster of paris and drill wires or surgically with a plate, but then without plaster of paris.
Open radius fractures usually require the application of an external fixator . The Smith fracture is treated by plating on the flexor side with a T-shaped plate.
- Spoke fractures near the wrist and their surgical treatment
Restoration by closed reduction with fixation with Kirschner wires
... and immobilization in the external fixator
See also
literature
- S2e guideline for distal radius fractures of the German Society for Trauma Surgery (DGU). In: AWMF online (as of 2015)
- S1 guideline for forearm shaft fractures in childhood of the German Society for Pediatric Surgery (DGKCH). In: AWMF online (as of 2013)
- A. Schierza, C. Meier: The conceptual and technical development of fracture management using the example of the distal radius fracture. (PDF) In: Swiss Medical Forum. 2010, Volume 10, pp. 325-329. (PDF; 1 MB)
- AJ Waldeyer: Anatomie des Menschen , Gruyter, 2009, ISBN 978-3-11-019353-4
- J. Grifka, J. Krämer: Orthopädie Unfallchirurgie , Springer, 2013, ISBN 978-3-642-28874-6
- FU Niethard, J. Pfeil, P. Biberthaler: Orthopädie und Unfallchirurgie, Duale Reihe, Thieme, 2014, ISBN 978-3-13-130817-7
Individual evidence
- ↑ Hebe Désirée Kvernmo, Leiv M. Hove, Katrine Bjørnebek Frønsdal, IngridHarboe, Adalsteinn Odinsson, Yngvar Krukhaug: Guidelines for treatment of distal radius fractures in adults. August 10, 2015, accessed October 3, 2016 .
- ↑ named after John Rhea Barton (1794–1871), the pioneer of arthroplasty . Cf. Barbara I. Tshisuaka: Barton, John Rhea. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 151 f.
- ↑ J. Schmidt: Pocket manual classifications in trauma surgery. 2nd Edition. blueprint, Berlin 2010.
- ↑ S. Tubeuf, G. Yu, J. Acht, NR Parsons, A. Rangan, SE Lamb, ML Costa: Cost effectiveness of Treatment with percutaneous Kirschner wires versus volar locking plate for adult patents with a dorsally displaced fracture of the distal radius . In: The Bone & Joint Journal , 2015, Volume 97-B, Issue 8, August 2015, pp. 1082-1090, doi: 10.1302 / 0301-620X.97B8.35234