Peroneal paralysis
| Classification according to ICD-10 | |
|---|---|
| G57 | Lower extremity mononeuropathies |
| G57.3 | Lesion of the common fibular nerve (peroneus) |
| ICD-10 online (WHO version 2019) | |
A peroneal paralysis is the result of damage to the common peroneal nerve (Synonyms: common peroneal nerve , common peroneal nerve ). This can affect the entire nerve or individual parts. This usually leads to a paralysis of the muscles that enable active foot and toe lifting. In animals, the ankle is stretched and the toes are bent, which means that the back of the foot is placed on the foot (so-called " killing ").
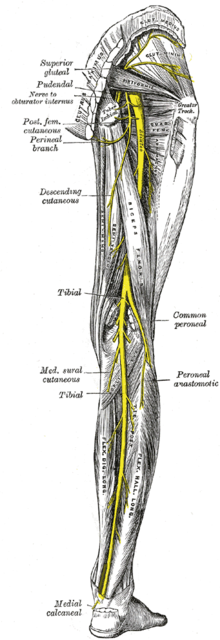
anatomy
The common peroneal nerve emerges from the sciatic nerve in the area of the thigh and divides in the area of the knee joint into its two main branches, the superficial peroneal nerve (“superficial fibrous nerve ”) and deep peroneal nerve (“deep fibula nerve ”). The superficial peroneal nerve is primarily sensitive , but also supplies the longus peroneal muscle and the brevis peroneus musculus , which are used for the pronation movement of the foot . The deep peroneal nerve supplies the muscles of the ankle joint and the muscles of the back of the foot that are required to lift the feet and has a sensitive supply area on the skin between the first and second toes.
Clinical picture
The failure pattern is also designed according to the above-mentioned supply area of the nerve.
If only the superficial peroneal nerve is affected, sensitive deficits occur on the front of the lower leg, back of the foot and extensor side of the first to fourth toes. However, the sensitivity remains in the area between the first and second toe. The loss of function of the peronei muscles means that the lateral edge of the foot cannot be actively lifted (impaired pronation ), which is why the foot is in a supination position , ie the outer edge of the foot is lowered in relation to the inner edge. It is possible to raise and lower the tip of the foot.
If only the deep branch (nervus peroneus profundus) fails, the patient cannot lift the tip of the foot by moving the ankle joint (disturbed dorsiflexion ). Raising the tips of the toes in the toe joints ( extension ) is also not possible. The tips of the feet and toes hang down, which is why when running in the swing leg phase, the entire foot must be lifted so that the hanging toe does not drag on the ground. This is done by increasing the flexion of the hip and knee joint . The resulting gait is called a " stepper walk " (other colloquial terms are "houndstooth" and "stork walk"). If left untreated, a so-called "pointed foot" can develop over time. In addition, the sensitivity of the skin between the first and second toe is disturbed.
In a lesion of the common peroneal nerve, both failure patterns are combined. Depending on the location of the lesion, the skin sensitivity also falls in a more or less large additional area on the lateral lower leg.
causes
Possible causes of peroneal paralysis are injuries, compression damage, masses and damage as part of medical measures ( iatrogenic ). Injuries (trauma) in the knee area (for example a fracture of the fibular head) can damage the nerve directly or indirectly (via accompanying soft tissue swelling or bleeding). Also dislocations at the level of the knee joint (Fibulaköpfchenluxation) or supination (twisting) of the foot are possible causes. A strong or rapid weight loss can also contribute to the development, since the cushioning function of body fat is limited. This can damage the myelin sheath of the nerve so that the conduction of stimuli is impaired. Compression damage can occur at pre-existing anatomical constrictions or can be caused by external pressure. An example of the first type of damage is the rare anterior tarsal tunnel syndrome . On the other hand, external pressure damage, such as with crossed-legs-palsy (by crossing the legs for too long) or by bandages (also with a plaster cast ), is much more common. Masses such as ganglia or neurofibromas can also lead to a functional failure of the nerve. As iatrogenic causes of peroneal paralysis, in addition to the bandages already mentioned, pressure damage caused by lying on the operating table or injuries during knee operations are possible.
Damage to the peroneal part of the sciatic nerve , from which the fibula nerve arises, can also result in peroneal paralysis. The main reasons for this are dislocations, fractures and operations in the pelvic, hip and thigh area as well as incorrectly placed intramuscular injections ( syringe paralysis ). Herniated discs can also damage the peroneal nerve.
Diagnosis
The damage can already be suspected on the basis of the clinical picture, but the differentiation from damage to the nerve root of L 5 is not always easy. The nerve conduction speed is reduced in the case of partial damage. The peroneal reflex may be weakened. The Achilles tendon reflex, which is generally easier to trigger, is preserved because the rear calf muscles are not supplied by the nerves. The nerve damage can also be objectified by measuring muscle action potentials in the supplied muscles.
Differential diagnosis
A herniated disc with root compression syndrome of the L 5 nerve root is a possible differential diagnosis . In addition, there are sensory disorders (loss of sensitivity and pain) in the dermatome L 5 , a weakening of the tibialis posterior reflex and possibly a so-called positive Trendelenburg sign . In the case of polyneuropathies , too, weakness in the foot and toe can be the main symptom. In contrast to peroneal paralysis, this shows the involvement of other nerves and the other leg. Damage to nerve cells in the central nervous system , for example through a stroke, can lead to what is known as the Wernicke-Mann gait, in which the affected leg is moved forward in an arc. The Amyotrophic Lateral Sclerosis always shows additional symptoms that they can be distinguished from a peroneal paralysis. Another differential diagnosis is tibialis anterior syndrome , a compartment syndrome in the lower leg compartment .
Therapy and prognosis
The therapy depends on the respective cause of the peroneal paralysis. The goal of therapy is to restore the nerve to full function or, if this is not possible, to avoid secondary complications such as equinus. A surgical procedure using nerve sutures in the case of partial or complete severing is possible and should be carried out in a specialized center as soon as possible in the case of fresh injuries. The results after nerve suturing or nerve transplantation with a defect are often moderate, depending on age and the soft tissue situation around the lesion. In the case of old injuries, the foot lift can be restored by repositioning the tendons from the calf. If the injury is fresh, redirecting a calf nerve to the muscle that is still intact that lifts the foot can produce very good results. If the patient does not qualify for an operation, the main focus is on physiotherapy to strengthen the other muscles. Putting on a so-called peroneal splint, which mechanically prevents the tip of the foot from dropping, can make walking much easier. Functional electrical stimulation (FES) can be used to support both disability compensation and long-term stimulation of neural reorganization with mobile foot lift systems. Peroneal paralysis as a result of pressure injuries such as crossing the legs for too long or after incorrect positioning have a good prognosis. On the other hand, if left untreated, peroneal paralysis as a result of nerve severance often results in permanent functional failure.
swell
- W. Pschyrembel: Clinical Dictionary. 260th edition. De Gruyter, Berlin / New York 2004, ISBN 3-11-014824-2 .
- P. Berlit: Clinical Neurology. 2nd Edition. Springer Verlag, Heidelberg 2006, ISBN 3-540-01982-0 .
- Karl F. Masuhr: Neurology. 5th edition. Hippokrates-Verlag, Stuttgart 1989, ISBN 3-7773-0840-4 .
- M. Mumenthaler, H. Schliack, M. Stöhr: Lesions of peripheral nerves and radicular syndromes. 7th edition. Georg Thieme Verlag, Stuttgart 1998, ISBN 3-13-380207-0 .
- FU Niethardt, J. Pfeil: Orthopedics . (= Dual row). 2nd Edition. Hippokrates-Verlag, Stuttgart 1992.
- Hans U. Steinau, et al .: Tendon transfers for drop foot correction: long-term results including quality of life assessment, and dynamometric and pedobarographic measurements. Arch Orthop Trauma Surg. 2011 Jul; 131 (7): 903-10. doi: 10.1007 / s00402-010-1231-z
- J. Kolbenschlag, et al .: Peroneal Palsy in Acute Diabetic Mononeuropathy with Complete Recovery after Surgical Decompression - A Case Report and Review of the Literature. Handchir Mikrochir Plast Chir. 2018 Dec; 50 (6): 439-442. doi: 10.1055 / s-0043-124186
- Theodor H. Schiebler: Anatomy. 8th edition. Springer-Verlag, Berlin / Heidelberg / New York 1995, ISBN 3-540-57240-6 .