disc prolapse
| Classification according to ICD-10 | |
|---|---|
| M50 | Cervical disc damage |
| M51 | Other disc damage |
| ICD-10 online (WHO version 2019) | |

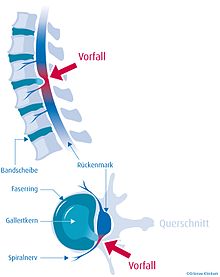
The herniated disc ( Latin: prolapsus nuclei pulposi , also intervertebral disc prolapse (BSP), disc hernia , disc prolapse ) is a disease of the spine in which parts of the disc protrude into the spinal canal - the space in which the spinal cord lies. In contrast to intervertebral disc protrusion (protrusion), the fibrous cartilage ring of the intervertebral disc (annulus fibrosus) is torn through completely or partially, while the posterior longitudinal ligament ( ligamentum longitudinal posterius)) can remain intact (so-called subligamentary disc herniation).
The cause is often an overload with previous damage to the intervertebral discs, but a herniated disc can also occur without an external cause. Symptoms of the herniated disc are severe pain, often radiating to the extremities, often with a feeling of numbness in the area supplied by the pinched nerve root; Treatment is usually conservative, serious incidents must be treated surgically.
history
The fact that a herniated disc can cause nerve root compression was first described in 1934 by neurosurgeon William Jason Mixter (1880-1958) and orthopedic surgeon Joseph Seaton Barr (1901-1963), who also performed a laminectomy as a surgical treatment for the first time .
causes

Intervertebral discs are bradytrophic tissue, which means that they are not supplied with nutrients directly from the bloodstream, but through diffusion . Here, playing semi-permeable membranes , which separate the cartilage rings from each other the decisive role. By shear forces , these membranes can tear, thereby losing their function and the disc along with the nucleus pulposus of the intervertebral disc (nucleus pulposus) dries out (black disc lesion). If there is a herniated disc, the nucleus is practically no longer present in its original form. The herniated disc usually arises from long-term previous damage to the intervertebral disc. The gelatinous nucleus (approx. 80% water) in a healthy intervertebral disc consists of a gelatinous, cell-poor tissue and, together with the cartilage rings and the membranes, takes on the function of a hydraulic ball ("water cushion") when stressed. The vertebral bodies and intervertebral discs at the front, together with the small vertebral joints at the rear (“facet joints”), enable the entire spine to be highly mobile and stable.
The human spine has 23 intervertebral discs. There is no intervertebral disc between the first vertebra (Latin atlas ) - counted from above - and the second vertebra ( axis ). This gives the head the necessary freedom of movement when nodding (atlas) and turning (axis). In addition, essential nerve cords and the blood supply to the head are concentrated there.
There are different causes for a herniated disc: genetic weaknesses, one-sided stress or a weakness of the paravertebral, i.e. the muscles next to the vertebrae. Damage to the intervertebral disc, exclusively due to accidents or injuries, has not yet been proven to be the cause - arguments contradicting this are very rarely recognized by professional associations and social courts. According to popular opinion, healthy intervertebral disc tissue should, if at all, tear out of the vertebral body together with a piece of bone. A herniated disc often occurs during pregnancy . There are many old people over 90 years of age who have never had problems with their spine or intervertebral discs in their busy lives. On the other hand, there are children who have already suffered a herniated disc.
Possible causes for the rapid increase in herniated discs today are a lack of exercise and poor posture, especially when working in office. In some studies, an increased risk of being overweight according to the body mass index compared to disc changes was found. A Finnish study showed a 2-fold increased risk of inpatient treatment for disc disease with a BMI> 27.5 kg / m².
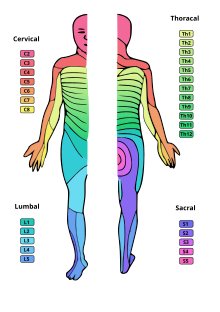
The average age of onset is 40 years, the vertebrae most frequently affected are in the lumbar region (lumbar region). The cervical vertebrae (cervical) are less frequently affected and the thoracic vertebrae (thoracic) only very rarely. The ratio is about 100 to 10 to 1.
Recent reports suggest that the severe pain may not be due to pinched nerves, but rather to an immune response or inflammation.
Symptoms
Many herniated discs are symptom-free and then do not require any treatment. In old healthy patients z. B. in more than 60% of the cases disc herniation found as an incidental finding. It is therefore important to determine before therapy whether the patient's symptoms can be explained by the affected intervertebral disc.
Typically, slipped discs cause back pain ( lumbar pain ) with or without radiation to the legs ( sciatica ) or arms ( brachialgia ). Depending on the severity of the symptoms, numbness or muscle failure in the supply area of the pinched nerve root can occur.
A herniated disc can lead to a positive Lasègue sign and Kernig's sign . In extreme cases it can lead to a cross-sectional syndrome . B. stool and / or urinary incontinence and breeches anesthesia occur.
Red flags
Red flags are anamnestic and clinical indications of an urgent need for further examinations in order to exclude other causes or to be able to treat them adequately. According to the German AWMF guideline, these are:
- accident
- Osteoporosis and minor trauma
- Tumor history
- infection
- Weight loss
- fever
- Pain intensification at night
- Progressive nerve failure
- Decreasing pain and paresis
- Kauda Syndrome
- Micturition disorder (typically urinary retention, overflow bladder, possibly incontinence)
Diagnosis

The spinal canal appears light in this evaluation technique, the dark protrusion coming from the left is the prolapse that clamps off the spinal canal.
A herniated disc can be diagnosed using MRI . As an alternative method, a herniated disc can also be detected by means of CT , which however has disadvantages compared to an MRI due to the radiation exposure and the poorer soft tissue contrast. Myelography is an older procedure that was used especially before the introduction of MRT and CT machines, but is still used today for special neurological questions or contraindications to an MRI examination . A contrast agent is injected into the liquor space.
After the examination, a neurologically experienced doctor should determine whether the changes found can explain the patient's symptoms or whether it is just an incidental finding.
Differential diagnosis
- Disc protrusion (disc tissue is only protruding outwards, the annulus fibrosus (fiber ring) is intact)
- Peripheral arterial disease (typically smokers. Increased discomfort when walking)
- Spinal stenosis (typically increased discomfort when walking)
- Hip wear (typically increased pain when rotating the hip)
- Sacroiliac joint osteoarthritis (typically sensitive to pressure)
- Facet joint arthrosis (typically only local back pain without radiating to the arms or legs)
- neuroforaminal stenosis (e.g. facet joint arthrosis)
- postoperative scar tissue
- Bannwarth syndrome (cases of painful inflammation of peripheral nerves)
treatment
If you maintain mobility, it is recommended that you return to normal activities as soon as possible. Bed rest is not recommended, as no therapeutic effect has been proven for this.
In the case of a lack of mobility, effective drug-based pain therapy should be carried out at an early stage.
Admission to hospital should take place in the event of Red Flags (see under symptoms), pain that cannot be controlled on an outpatient basis and increasing neurological deficits.
Heat therapy, massages with movement therapy, electrotherapy, connective tissue massages can alleviate the symptoms in individual cases. The benefit can be z. T. not scientifically proven.
A Manual medicine ( chiropractic , spinal manipulation) is contraindicated in radiating pain. In the case of acute, non-radiating pain, therapy can be helpful within the first 4–6 weeks.
Physiotherapy ( physical therapy ) is useful in chronic and sub-acute pain. So far, no benefit has been demonstrated in the acute stage.
The Feldenkrais method , Alexander technique , Hatha yoga , the McKenzie concept , spiral dynamics and acupuncture are among the many therapeutic and diagnostic approaches .
For patients who suffer from back pain that radiates into the leg, the so-called back school can be helpful for chronic complaints .
The Periradicular Therapy (PRT) is a process-control X-cortisone is injected to the affected nerve root at the under CT or that should be performed at least 2 ×. In 67% of the cases, pain relief can be achieved with a herniated disc. In Germany, the examination for statutory health insurance patients is usually not paid for by the health insurance company . Possibly. the costs are covered if a pain therapist refers the patient to a radiologist.
A bloodless procedure is the sclerosing of the synovium (synoviorthesis), in which varicocid or osmium tetroxic acid is injected into the inflamed joint . For older patients, radioactive isotopes are used instead of these chemical substances. Furthermore, there is the possibility of enzymatic treatment of the herniated disc by chemonucleolysis by injecting the enzyme chymopapain , which leads to the dissolution or volume reduction of herniated disc tissue .
Operative therapy
Because of the high rate of complications, there is a strict indication for surgery.
Clear indications for surgery according to the AWMF guidelines are:
- Cauda equina syndrome with acute paraparesis in the case of an extensive herniated disc or a fractured vertebral body.
- Bladder and rectal paralysis
- Increasing or acute severe muscle loss
Surgery can be performed as a last resort if all non-surgical procedures have been attempted and the pain is still unbearable.
Surgery complications a. be:
- Frequently postoperative scarring, which z. B. can pinch the nerve root or the dural sac .
- Often reprolapse / relapse
- Partly severe infection, possibly with abscesses
- Liquor leakage ( Liquor cerebrospinalis ) when the dura is injured, e.g. B. with severe headache
The recurrence rate in microsurgical operations is> 10%.
The implantation of artificial intervertebral discs for pain therapy is (as of 2005) assessed critically.
In 2013, the AOK Hospital Report showed that the number of intervertebral disc operations doubled between 2005 and 2010.
The SPORT study (SPORT = Spine Patient Outcomes Research Trial) came to the conclusion that in the case of persistent sciatica due to a herniated disc, the operation still has an advantage over conservative treatment after 8 years because of the difficulty in allocating to the different treatment groups and the summary a number of different studies on a large study leave some room for interpretation.
The most frequently performed surgical method is microdiscectomy, in which the slipped disc tissue is removed through a 3–5 cm long incision above the spine. So-called minimally invasive interventions and microsurgical procedures, such as percutaneous laser disc decompression (PLDD), are being used more and more often, even if the results in clinical studies are not better. It is argued, however, that access, i.e. H. the scar is smaller and therefore less traumatizing. Endoscopic transforaminal disc surgery is also gaining in popularity.
prevention
Since the so-called " connective tissue weakness " is hereditary as the primary cause, a herniated disc can only be prevented to a limited extent by building muscle. It will not always be possible to avoid accidents either. In any case, each individual has the option of consistently building muscles in the back area through gymnastic exercises or sport, as well as avoiding lifting heavy loads. There are techniques that can be learned to handle heavy loads in a “back-friendly” manner, but avoiding such actions is not possible in every profession (e.g. nursing).
Bodybuilding and fitness training can be problematic in studios with less qualified staff, as malpositions are not always recognized there.
Also worth mentioning are the "orthopedic sports", swimming , dancing , running (or jogging, Nordic walking), riding and cycling , which, in addition to building muscle, enable the changing pressure load that is important for intervertebral discs. According to the findings of modern sports medicine, whether sports such as riding or running (on asphalt / cemented ground) as well as cycling in a strongly bent posture are to be avoided after a herniated disc always depends on the individual damage.
An important measure to prevent a herniated disc is correct ergonomics in the workplace. In addition to physical work, this also applies to activities that are performed while sitting. Nowadays there are many ergonomic solutions for working at the screen, at the desk and for work that requires long static sitting positions. Since the intervertebral disc is not supplied by blood vessels, it is dependent on changing pressure loads to exchange the nutrient fluid, which means that static sitting positions should be avoided as far as possible.
Web links
- AWMF guidelines on lumbar radiculopathy
- Bernhard Meyer : Operation for a herniated disc - neurosurgeons warn of patient uncertainty . (PDF) Press release, DGNC annual conference , April 2014
Individual evidence
- ↑ William Jason Mixter, Joseph Seaton Barr: Rupture of the intervertebral disc with involvement of the spinal canal . New England Journal of Medicine 1934; Volume 211, pp. 210-215
- ↑ CH Flame: Obesity and damage to the intervertebral disc. Biology, biomechanics and epidemiology. In: Der Orthopäde , 34, 7/2005, pp. 652-657, doi: 10.1007 / s00132-005-0817-6 .
- ↑ L. Kaila-Kangas, P. Leino-Arja, H. Riihimäki, R. Luukonen, J. Kirjonen: Smoking and overweight as predictors of hospitalization for back disorders. In: Spine , 28, 2003, pp. 1860-1868.
- ↑ A herniated disc causes inflammation of the spinal cord . Aachen News Online
- ↑ a b c long version of the AWMF guideline on radiculopathy, lumbale from September 30, 2012 ( Memento from February 22, 2014 in the Internet Archive ) (PDF; 901 kB)
- ↑ A. Indahl, EH Haldorsen, S. Holm et al .: Five-year follow-up study of a controlled clinical trial using light mobilization and an informative approach to low back pain. Spine (Phila Pa 1976) 1998; 23: 2625-2630
- ↑ O. Airaksinen, JI Brox, C. Cedraschi et al .: Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J 2006; 15 (Suppl. 2), pp. S192-S300
- ^ JA Hayden, MW van Tulder, A. Malmivaara et al .: Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev 2005a; 3: CD000335
- ^ JA Hayden, MW van Tulder, G. Tomlinson: Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med 2005b; 142, pp. 776-785
- ^ WC Peul, HC van Houwelingen, WB van den Hout et al .: Surgery versus prolonged conservative treatment for sciatica. N Engl J Med 2007; 356, pp. 2245-2256
- ↑ SS Kang, BM Hwang, HJ Son et al .: The dosages of corticosteroid in transforaminal epidural steroid injections for lumbar radicular pain due to a herniated disc. Pain Physician 2011; 14, pp. 361-370
- ↑ Wolfgang Miehle: Joint and spinal rheumatism. Eular Verlag, Basel 1987, ISBN 3-7177-0133-9 , pp. 81 and 173.
- ↑ J. Kramer, H. Kleinert, A. Senge et al .: Intervertebral disc prostheses: review, moment, outlook. Z Orthopedics and border areas 2005; 143, pp. 281-286
- ↑ Is a back operation really necessary? Medipress; Retrieved June 19, 2013
- ↑ Jon D. Lurie, Tor D. Tosteson, Anna NA Tosteson, Wenyan Zhao, Tamara S. Morgan, William A. Abdu, Harry Herkowitz, James N. Weinstein: Surgical Versus Nonoperative Treatment for Lumbar Disc Herniation. In: Spine. 39, 2014, pp. 3-16, doi: 10.1097 / BRS.0000000000000088 .
- ↑ Sciatica: SPORT study sees disc surgery as an advantage in the long term . aerzteblatt.de
- ^ JN Alastair Gibson, Gordon Waddell, Surgical interventions for lumbar disc prolapse . Cochrane Database of Systematic Reviews 2007, Issue 2, Art. No .: CD001350. doi: 10.1002 / 14651858.CD001350.pub4 .
- ↑ J. Lagarrigue, P. Chaynes: Comparative study of disk surgery with or without microscopy. A prospective study of 80 cases . Neurosurgery Volume 40, Issue 2, pp. 116-120.
- ↑ JN Alastair Gibson et al .: Transforaminal endoscopic spinal surgery: The future 'gold standard' for discectomy? - A review. The Surgeon , Volume 10, Issue 5, pages 290-296
- ↑ J. Hildebrandt (ed.), M. Pfingsten (ed.): Back pain and lumbar spine: Interdisciplinary practice book - in accordance with the national care guidelines. 2nd Edition. Urban & Fischer, 2011