Peri-implantitis
As periimplantitis (peri- Greek. : Περί around something in- lat. , In ', plantar , plants', itis , Greek. -Ίτις , inflammatory disease) is defined as analogous to periodontitis , which describes an inflammation of the tooth bed , the inflammation of the implant bed of dental implants . The preliminary stage of peri-implantitis is mucositis , an inflammation of the mucous membrane surrounding the implant neck.
causes
Peri-implantitis is caused by a mixed anaerobic microflora in which gram-negative bacteria are in the foreground. Also Staphylococcus aureus may be involved. The germs that cause periodontitis, such as Aggregatibacter actinomycetemcomitans , Prevotella intermedia, Porphyromonas gingivalis and Treponema denticola , are not specific. The germs Tannerella forsythia , Campylobacter species and Peptostreptococcus micros , however, are directly related to peri-implantitis. Peri-implantitis leads to osteolysis . Comparable to periodontitis, plaque deposits on implants are primarily responsible for the inflammatory process, which suggests inadequate oral hygiene . The peri-implant mucosa is less well supplied with blood than the periodontal tissue of the tooth, which results in a reduced resistance to infection in this area.
With assembled implants there are gaps and cavities between the actual implant and the abutment, into which germs from the oral cavity can penetrate. These germs later find their way back into the adjacent tissue and can thus cause peri-implantitis. As a prophylaxis, these implant interiors should be sealed.
predisposition
Peri-implantitis can be favored by diabetes , nicotine consumption , bisphosphonate therapy, osteoporosis , immunosuppression , radiation , bruxism but also by genetic disposition .
Medical malpractice
Damage to the implant bed due to surgical errors during the procedure can lay the foundation for peri-implantitis. This includes thermal or mechanical trauma to the bone, the latter due to compression of vital bone tissue, subcrestal positioning of the polished implant neck or incorrect positioning of the implant.
A faulty superstructure can also promote peri-implantitis. These include inadequate hygiene of the implant, tension due to prosthetic malfitting or micro-movements of the superstructure. Failure to remove excess subgingival cement, with which the superstructure (tooth crown) is attached to the implant, also creates an inflammatory stimulus that leads to peri-implantitis with bone loss.
Diagnosis
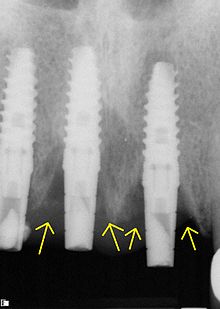
The diagnosis of peri-implantitis takes place in two steps. First, the clinical diagnosis is carried out by probing the peri-implant area using periodontal probes . Bleeding, which can also be accompanied by evacuation of pus , leads to the suspected diagnosis of peri-implantitis, which can then be differentiated or confirmed from pure mucositis by means of x-rays , preferably by intraoral dental film recordings. The mucositis runs supracrestal, i.e. above the bone border. The defect classification is based on Schwarz et al.
| class | description |
|---|---|
| Class I. | intraosseous |
| Class I a | Vestibular or oral dehiscence defects * |
| Class I b | Vestibular or oral dehiscence defects with semi-circular bone resorption up to the middle of the implant body * |
| Class I c | Dehiscence defects with circular bone resorption while preserving the vestibular or oral compact layer * |
| Class I d | Circular bone resorption with vestibular and oral loss of the compact layer * |
| Class I e | Circular bone resorption while preserving the vestibular and oral compact layer |
| Class II | supracrestal |
- Position of the implant body inside or outside the envelope
Peri-implantitis is painless for a long time. Depending on the extent of bone loss, the implant may be loose.
therapy
Mucositis
Initially, peri-implantitis is usually preceded by mucositis , an inflammation of the mucosa ( mucous membrane ) surrounding the implant neck , whereby the transition from mucositis to peri-implantitis is fluid. The therapy consists of debridement , mechanical cleaning of the implant surface. The additional use of local or systemic antibiotics or disinfectants , such as chlorhexidine digluconate , did not result in any improvement in therapy.
Peri-implantitis
In contrast to mucositis, peri-implantitis requires surgical intervention to achieve long-term success. After the granulation tissue has been removed and the implant has been cleaned, augmentative measures ( bone augmentation procedures ) can be used. Xenogenic (alien) bone substitute materials of bovine origin (cattle) show better results than autogenic or alloplastic materials. Other methods, such as the use of polytetrafluoroethylene (PTFE) barrier membranes , did not improve the results.
forecast
The peri-implant mucositis can be treated with a high chance of success. With a timely diagnosis or close recall and professional teeth cleaning , a recurrence can be avoided.
The prognosis of peri-implantitis depends on the severity, i.e. the extent of the bone loss. The augmentative procedures and resective treatment procedures can bring the inflammation to a standstill and in some cases also lead to a regeneration of the broken down bone. The results are assessed differently in the specialist literature.
The last resort is explantation, i.e. removal of the implant. The bone can then be rebuilt in order to place another implant.
Cost effectiveness
An assessment of the cost-effectiveness of various therapeutic strategies against peri-implant inflammation is only possible to a limited extent due to the lack of robust clinical evidence.
Billing
Just like implant services (apart from a few exceptional indications), treatment methods for the treatment of peri-implantitis are not part of the list of benefits provided by the statutory health insurance , for example:
- Augmentative procedures (bone building procedures )
- Free Ginigiva Grafts ( Grafting )
- Bone grafts
- Functional therapeutic services
- Widening of the fixed gingiva,
- Professional tooth cleaning
In the case of private patients, these can be settled in accordance with the schedule of fees for dentists (GOZ) or the schedule of fees for doctors (GOÄ) or by means of a private written additional agreement before the start of treatment for statutory health insurance patients .
See also
Individual evidence
- ↑ PL Casado, IB Otazu u. a .: Identification of periodontal pathogens in healthy peri-implant sites. In: Implant dentistry. Volume 20, Number 3, June 2011, pp. 226-235, ISSN 1538-2982 . doi: 10.1097 / ID.0b013e3182199348 . PMID 21613949 .
- ↑ G. Tabanella, H. Nowzari, J. Slots: Clinical and microbiological determinants of ailing dental implants. In: Clinical Implant Dentistry and Related Research . Volume 11, Number 1, March 2009, pp. 24-36, ISSN 1708-8208 . doi: 10.1111 / j.1708-8208.2008.00088.x . PMID 18384407
- ↑ CU Fritzemeier, W. Schmüdderich: Peri-implantitis prophylaxis by sealing the implant interiors, Implantologie 2007; 15 (1), pp. 71–80.
- ↑ a b c Peri-implantitis: Prevention - Diagnostics - Therapy 3rd European Consensus Conference (EuCC) Cologne 2008.
- ↑ F. Schwarz, M. Herten u. a .: Comparison of naturally occurring and ligature-induced peri-implantitis bone defects in humans and dogs. In: Clinical Oral Implants Research . Volume 18, Number 2, April 2007, pp. 161-170, ISSN 0905-7161 . doi: 10.1111 / j.1600-0501.2006.01320.x . PMID 17348880 .
- ↑ S. Reinhardt: Soft tissue thickening with a xenogenic connective tissue substitute. (PDF; 75 kB) In: Bayerisches Zahnärzteblatt. 4/2012.
- ↑ a b p Renvert, A. Aghazadeh, H. Hallstrom, GR Persson: Factors related to peri-implantitis - a retrospective study. In: Clinical oral implants research. [electronic publication before printing] June 2013, ISSN 1600-0501 . doi: 10.1111 / clr.12208 . PMID 23772670 .
- ↑ AM Roos-Jansåker, C. Lindahl u. a .: Long-term stability of surgical bone regenerative procedures of peri-implantitis lesions in a prospective case-control study over 3 years. In: Journal of Clinical Periodontology . Volume 38, Number 6, June 2011, pp. 590-597, ISSN 1600-051X . doi: 10.1111 / j.1600-051X.2011.01729.x . PMID 21488935 .
- ↑ Stefan Listl, Nadine Frühauf, Bettina Dannewitz, Christiane Weis, Yu-Kang Tu, Huei-Ju Chang, Clovis M. Faggion: Cost-effectiveness of non-surgical peri-implantitis treatments. In: Journal of Clinical Periodontology. 42, 2015, p. 470, doi : 10.1111 / jcpe.12402 .