Bisphosphonates
Bisphosphonates (also diphosphonates ) are chemical compounds that have two phosphonate groups .
use
Bisphosphonates belong to a group of drugs that have been developed for diagnostic and therapeutic purposes in bone and calcium metabolism diseases since the 1980s . Some compounds of this type are used in drugs for the treatment of osteoporosis . They are approved in Germany for the treatment of osteoporosis in postmenopausal women, osteodystrophia deformans and tumor-associated hypercalcemia . They are also used in the treatment of bone metastases and fibrous dysplasia .
In a 2009 study, the addition of zoledronate (a bisphosphonate substance) to endocrine therapy for hormone-sensitive breast cancer resulted in a longer relapse-free survival time.
Bisphosphonates are also used in conjunction with 99m technetium as tracers in the nuclear medical examination method skeletal scintigraphy . They are used in a very low, pharmacologically ineffective dose.
The bisphosphonate Lexidronam is used in conjunction with the predominantly beta emitter 153 samarium for palliative analgesic therapy in bone metastases ( radionuclide therapy ).
Mechanism of action
Bisphosphonates can only cross biomembranes with great difficulty, but the osteoclasts ingest bisphosphonates as part of the breakdown of bone substance through phagocytosis . This uptake leads to the fact that the lifespan of the osteoclasts is shortened. This in turn ultimately brings about the therapeutically desirable reduction in bone loss.
Bisphosphonates have several effects on the bones: By attaching to the bone surface, on the one hand they inhibit the mineralization of the bone substance, on the other hand they inhibit bone breakdown by inhibiting osteoclast activity: in particular, the nitrogen-rich bisphosphonates inhibit proton ATPase (direct toxic effect) and inhibit the enzymes involved in mevalonic acid metabolism . Their direct influence on the monocyte - macrophage system has also been experimentally and clinically proven by torpedoing the recruitment and fusion of osteoclast precursors. They also cause the reduction of osteoclastic life due to induction of apoptosis , probably associated with a prolongation of osteoblastic life: Inhibition of farnesyl pyrophosphate - synthase , the products of this enzyme farnesyl and geranyl small G proteins (u a.. Ras no longer) Anchoring the cell membrane. If these G proteins are missing , growth factors bound to cell receptors no longer have any effect on the cell. As a result, the osteoclasts die as part of apoptosis. Finally, they act to inhibit prostacyclins and other cytokinins in bone tissue.
Active ingredients
The bisphosphonates are esters and salts of methylenediphosphonic acid (medronic acid). They are diphosphate - analogs in which the oxygen of the P-O-P bond by carbon is replaced. Compounds of this type are among the phosphonates . They are not subject to enzymatic hydrolysis in the body . Before their therapeutic effect on osteoporosis was discovered, bisphosphonates were used, among other things, as detergent additives. Modifications of the molecular structure gradually improved their therapeutic properties. The latest bisphosphonates are 20,000 times more potent than etidronate , the first-generation bisphosphonate. They differ in the side chains and therefore form four groups:
- Bisphosphonate without nitrogen: etidronate, clodronate , tiludronate
- Aminobisphosphonates: pamidronate , alendronate
- aminobisphosphonates substituted on nitrogen: ibandronate
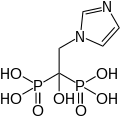
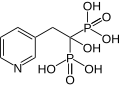
- Bisphosphonates with a basic heterocycle: risedronate , zoledronate .
The following bisphosphonates are approved in Germany: alendronate, clodronate, etidronate, ibandronate, pamidronate, risedronate, tiludronate and zoledronate . Oxidronate (HDP) (only approved in Switzerland) is used for skeletal scintigraphy .
- Bisphosphonates used in medicine
Alendronic acid, used to treat osteoporosis
Hydroxyethylidene
diphosphonate (HEDP, etidronic acid) for skeletal scintigraphyIbandronic acid, used to treat bone metastases in breast cancer and osteoporosis
Zoledronic acid, used to treat osteoporosis , TIH and bone metastases
Risedronic acid, used to treat osteoporosis (including steroid-induced) and Paget's disease
Pharmacokinetics
Bisphosphonates are poorly absorbed in the intestine and form insoluble complexes with calcium . The absorption rate after oral ingestion is between 1 and 10% of the dose taken , in some cases it is even lower. The intake rules must therefore be strictly adhered to. Bisphosphonates should be taken on an empty stomach with a full glass of tap water at least 30 minutes before further food or other medication. These regulations do not apply to intravenous administration by infusion or syringe .
About 20–50% of the amount absorbed is stored in the bone . The remainder is excreted in the urine or stool within 24 hours . The half-life of bisphosphonates in the skeleton is many years, similar to that of tetracyclines or strontium .
Side effects
When administered orally, gastrointestinal symptoms such as nausea, abdominal pain, vomiting and diarrhea occur in two to ten percent of patients. An upright posture during use can prevent backflow into the esophagus (gastroesophageal reflux) and thus gastrointestinal disturbances. Occasionally, hypocalcaemia can occur due to the formation of complexes with calcium ions in the intestine . In pregnancy and lactation bisphosphonates are contraindicated.
Recently, growing evidence on bisphosphonatassoziierte osteonecrosis of the jaw (bonj, bisphosphonate-associated osteonecrosis of the jaw or BRONJ, bisphosphonate-related osteonecrosis of the jaw ), the clinically symptoms of ORN are similar and are very resistant to therapy. A relevant risk for BP-associated ONJ exists when bisphosphonates are administered intravenously in high doses and over a longer period of time because of an underlying malignant disease. The CHMP (Committee for Medicinal Products for Human Use) of the EMA (European Medicines Agency) confirmed these undesirable effects from the data of the eudravigilance project in a communication dated September 24, 2009 and called for further research into the causes. But even with oral medication alone, cases of jawbone necrosis are now known, mostly in connection with a previous tooth extraction. The bisphosphonates inhibit endothelial cells and thus disrupt intraosseous angiogenesis of the bone. The damaged bone is therefore limited in its ability to react to infections or trauma.
Bisphosphonate-associated jaw necrosis was described as a syndrome after a latency period of a good ten years after the first bisphosphonates were approved in the late 1980s. These were similar to the jaw Phosphornekrosen the jaw , English phossy jaw , after poisoning by white phosphorus as in the 19th century from the match were known -Industrie. The clinical diagnosis of bisphosphonate-associated jaw necrosis is difficult to make. By definition, it arises from the anamnesis with pretreatment with oral or intravenous bisphosphonates. In some studies, the facial skull has up to 20 times more bony remodeling activity than the rest of the skeleton, which could explain the increased storage of bisphosphonate in the jawbone.
Bisphosphonates used in skeletal scintigraphy have no side effects due to the extremely low dosage. Only in the event of a faulty injection into the tissue next to the vein does a very brief burning sensation occur. The restrictions on the indication of nuclear medical examinations during pregnancy and breastfeeding as well as radiation exposure from the radionuclide must be observed.
According to the HORIZON study, treatment with the bisphosphonate zoledronic acid also developed severe atrial fibrillation in not a few patients (1.3 percent) , which had not previously been observed with bisphosphonates. Atrial fibrillation was below the rate expected for this age group and was not seen in other studies with zoledronic acid.
More recent studies on the long-term use of alendronic acid led to a reference in the WHO Pharmaceuticals newsletter in the Safety of Medicines section to the publication of the MHRA regarding possible atypical fractures of the femoral shaft ( corpus ossis femoris ). Atypical fractures of the femur usually occur on the proximal shaft and show typical radiological features. They can be triggered by minimal trauma, but they also occur without trauma. The fractures are often bilateral and have a poor tendency to heal. The suspicion that bisphosphonates disrupt bone remodeling in the long term and significantly increase the risk of fractures is corroborated by a more recent study. However, after five years of treatment, the benefit-risk ratio is still favorable. On the basis of epidemiological evidence, the CHMP at the European Medicines Agency (EMA) has comprehensively assessed a possible connection between atypical femoral fractures and the administration of bisphosphonates on the basis of the available data.
Other possible side effects of bisphosphonates are confusion and visual, acoustic and olfactory hallucinations .
Individual evidence
- ↑ R. Chapurlat: Current pharmacological treatment for fibrous dysplasia and perspectives for the future. In: Joint Bone Spine . Volume 72, number 3, 2005, pp. 196-198, doi: 10.1016 / j.jbspin.2004.08.001 .
- ↑ M. Gnant, B. Mlineritsch, W. Schippinger et al .: Endocrine therapy plus zoledronic acid in premenopausal breast cancer. In: N Engl J Med . Volume 360, Number 7, February 2009, pp. 679-691, PMID 19213681 .
- ↑ Heinz Lüllmann , Klaus Mohr , Lutz Hein : Pharmacology and Toxicology. Thieme, Stuttgart 2006, ISBN 978-3-13-368516-0 , pp. 262-264.
- ↑ R. Bartl, C. Bartl, R. Gradinger: Use of bisphosphonates in orthopedics and trauma surgery . In: The orthopedist . tape 37 , no. 6 , June 2008, p. 595-614 , doi : 10.1007 / s00132-008-1280-y .
- ^ Bisphosphonates and osteonecrosis of the jaw. (PDF; 171 kB) EMA , September 24, 2009, accessed on June 9, 2017 (English).
- ↑ Robert E Marx: Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic . In: Journal of Oral and Maxillofacial Surgery . tape 61 , no. 9 , September 2003, p. 1115–1117 , doi : 10.1016 / S0278-2391 (03) 00720-1 .
- ↑ Stefan Lachmann, Siegmar Reinert, Sebastian Hoefert: Topic with great practical relevance. Tübingen bisphosphonate symposium. In: ZM . Volume 102, No. 6A, March 16, 2012, pp. 716-720 ( online ).
- ↑ Results of the randomized HORIZON study: Once-Yearly Zoledronic Acid for Treatment of Postmenopausal Osteoporosis. In: New England Journal of Medicine . Volume 356, 2007, pp. 1809-1822, doi: 10.1056 / NEJMoa067312 . Quoted here from: Deutsches Ärzteblatt . May 3, 2007 (online) .
- ^ Bisphosphonates: atypical femoral fractures . In: Drug Safety Update . tape 4 , no. June 11 , 2011 ( online ).
- ↑ E. Shane, D. Burr, PR Ebeling et al .: Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. In: J Bone Miner Res . Volume 25, No. 11, 2010, pp. 2267-2294, doi: 10.1002 / jbmr.253 .
- ↑ Laura Y. Park-Wyllie, Muhammad M. Mamdani, David N. Juurlink, et al .: Bisphosphonate Use and the Risk of Subtrochanteric or Femoral Shaft Fractures in Older Women . In: JAMA . tape 305 , no. February 8 , 2011, doi : 10.1001 / jama.2011.190 .
- ^ European Medicines Agency concludes class review of bisphosphonates and atypical fractures. EMA , April 15, 2011, accessed June 9, 2017 .