Breast cancer
| Classification according to ICD-10 | |
|---|---|
| C50 | Breast cancer |
| C50.0 | Nipple and areola |
| C50.1 | Central glandular body of the mammary gland |
| C50.2 | Upper inner quadrant of the mammary gland |
| C50.3 | Lower inner quadrant of the mammary gland |
| C50.4 | Upper outer quadrant of the mammary gland |
| C50.5 | Lower outer quadrant of the mammary gland |
| C50.6 | Axillary recess of the mammary gland |
| C50.8 | Mammary gland, overlapping several areas |
| C50.9 | Mammary gland, unspecified |
| ICD-10 online (WHO version 2019) | |

Breast cancer or breast carcinoma (from the Latin mamma "teat, breast; female mammary gland") is the most common malignant tumor of the human mammary gland . It occurs mainly in women; only about every hundredth of these cancers occurs in men. Breast cancer is the most common type of cancer in women in western states. More women die from breast cancer than from any other cancer. Most diseases are sporadic (random), but there are both hereditary and acquired risk factors. In addition to healing, the preservation of the breast concerned and above all the quality of life are the declared goals of medical treatment.
The therapy usually consists of a combination of surgery and cytostatic , hormone and radiation therapy adapted to the stage of the disease . New approaches in the field of cancer immunotherapy are also made possible by monoclonal antibodies (such as the administration of trastuzumab or pertuzumab ). The medical procedure is based to a large extent on experience from studies, often follows evidence-based medicine and is standardized in globally accepted guidelines . Numerous national and international programs for early detection and structured treatment are intended to reduce mortality (mortality) in the future.
Epidemiology
Breast cancer in women
In Germany, breast cancer is the most common cancer in women, accounting for 32% of all new cancer cases . The lifetime risk is given as 12.9%, i.e. H. around one in eight women will develop breast cancer at some point in their lives. In Germany, this is around 71,900 new cases per year (2019) or 171 cases per 100,000 inhabitants per year.
In international comparisons, the different age distribution of the national populations must be taken into account. The age-standardized incidence (rate of new cases) in Germany in 2010 for women according to the so-called European Standard (ESR) was 119.6 / 100,000. The death rate ( mortality ) from breast cancer in the same year, standardized for age, was 24.0 / 100,000 according to the ESR. The number of cases has doubled since 1970, while mortality has tended to decline.
Breast cancer is the most common invasive tumor disease in women worldwide. According to estimates by the WHO (2003), there are around 1,050,000 new cases of the disease worldwide every year, 580,000 of them in industrialized countries. The disease is comparatively less common in Africa and Asia. Around 412,000 women worldwide died of breast cancer in 1998, that is 1.6% of all women who died. This makes breast cancer the leading cause of cancer-related death in women worldwide. In the western world, breast cancer is the leading cause of death in women between the ages of 30 and 60.
It is estimated that there are about 17,460 breast cancer-related deaths per year in Germany and about 40,200 in the United States. In Germany, the average five-year survival rate is currently 86–90%. However, while the death rate is falling in rich countries, it is high in poorer countries. This is related on the one hand to the ever increasing life expectancy and on the other hand to the poorer diagnostic and therapeutic options in poorer countries. According to the WHO, about 72 percent of all people with cancer died in 2007 in middle- and low-income countries. However, there is currently a phenomenon of rising breast cancer rates in young women in the United States for which there is no satisfactory explanation.
| Number of women who died of breast cancer in Germany by age group |
||||
| Age | 2003 | 2004 | 2005 | 2006 |
|---|---|---|---|---|
| 0-30 | 16 1 | 20 2 | 16 | 13 |
| 30-40 | 348 | 318 | 294 | 294 |
| 40-50 | 1,271 | 1,296 | 1,283 | 1,176 |
| 50-60 | 2,493 | 2,404 | 2,419 | 2,489 |
| 60-70 | 4.158 | 4,441 | 4,252 | 4,035 |
| 70-80 | 4.140 | 4,354 | 4,273 | 4,283 |
| > 80 | 4,747 | 4,759 | 4,918 | 4,996 |
| total | 17.173 | 17,592 | 17,455 | 17,286 |
|
1 A girl 5–10 years
2 A girl aged 10–15
|
||||
| Share of cause of death "breast cancer" in percent by age group (women only, Germany) |
||||
| Age | 2003 | 2004 | 2005 | 2006 |
|---|---|---|---|---|
| 0-30 | 0.4 | 0.5 | 0.5 | 0.4 |
| 30-40 | 10 | 11 | 10 | 11 |
| 40-50 | 13 | 14th | 14th | 13 |
| 50-60 | 14th | 14th | 13 | 14th |
| 60-70 | 9 | 10 | 10 | 10 |
| 70-80 | 4th | 5 | 4th | 5 |
| > 80 | 2 | 2 | 2 | 2 |
Breast cancer in men
Men are less likely to develop breast cancer. In Uganda, five percent of all breast cancer patients are male, in Zambia the proportion is as high as 15 percent. According to current statistics for 2019, there are around 700 men a year in Germany. The ratio of diseases in men to women is 1: 100. The standardized global incidence rates for breast cancer were 0.40 per 10 5 person-years for men (66.7 per 10 5 for women). The diagnosis is made in men at a higher median age (69.6 years). Male patients have a poorer relative 5-year survival rate than women (0.72 [95% CI : 0.70-0.75] and 0.78 [95% CI: 0.78-0.78] ), which corresponds to a relative increased mortality risk of 1.27 (95% CI: 1.13–1.42), but after adjustment for age and year of diagnosis, stage and therapy, they show a significantly better relative breast cancer-associated survival than Patients. Mortality in men is around 200 deaths per year. A study by the European Organization for Research and Treatment of Cancer (EORTC) together with other professional associations from Europe and North America aims to elucidate the causes of this gender difference in detail.
Risk factors for breast cancer in men
The incidence of breast cancer in men is increased by demographic, genetic, environmental, and endocrine factors:
| group | Risk factor |
|---|---|
| Demographics | older age |
| African American | |
| familial risk | |
| genetics | BRCA2 |
| BRCA1 | |
| CHEK2 | |
| PALB2 | |
| environment | Radiation exposure |
| Endocrine factors | Serum estradiol increased |
| Klinefelter Syndrome | |
| Gynecomastia | |
| Liver dysfunction | |
| Obesity | |
| Disorder of testicular function |
Notes: CHEK2 is involved in DNA repair. The gene encodes a cell cycle checkpoint kinase. PALB2 is named partner and localizer of BRCA2. The gene encodes a protein that interacts with the breast cancer risk factor BRCA2.
The establishment and support of the first self-help network “Network Men with Breast Cancer e. V. ”has taken over the nationwide women's self-help after cancer (FSH) in Bonn under the patronage of the German Cancer Aid Foundation . In addition to the network Men with breast cancer and the Infonetz cancer also offers cancer information service information on this topic.
Symptoms of a disease are liquid discharge from the nipple , small inflammations or sores that do not heal or recover the breast skin at one point or the nipple.
For treatment, both areas that are suspected of being tumors and neighboring lymph nodes can be removed from the armpit in one operation . It is through such lymph nodes that tumor cells are most likely to spread in the body. Radiotherapy of the chest wall and possibly chemotherapy is also possible . Anti-hormonal therapy can also be useful for men if their tumor grows in an estrogen-dependent manner, and / or therapy with antibodies that are directed against special characteristics of some breast cancer cells. Men also make the hormone estrogen , but to a much lesser extent than women.
Causes and Risk Factors
Genetic Risk Factors
About 5 to 10% of breast cancers can be hereditary. Defined, disease-causing mutations are only found in a small group of women (around 1 in 500) . Genetic changes that increase the susceptibility (receptivity) for breast cancer to external factors are much more common .
The highest probability of developing the hereditary form of breast cancer is in women with mutations in the genes BRCA1 and BRCA2 ( BRCA1 / 2 = Breast Cancer Gene 1/2 ). It already comes with a mutation in one allele of these genes to disease (one speaks of so-called tumor suppressor genes with autosomal - dominant inheritance ). The probability of developing breast cancer in the course of life is given as 65% for carriers of the mutated BRCA1 and 45% for carriers of the mutated BRCA2.
Mutations in the p53 gene, one of the tumor suppressor genes , are inherited in an autosomal dominant manner ( Li-Fraumeni syndrome ). Other genetic changes that increase the risk include mutations of PTEN ( Cowden syndrome ), STK11 ( Peutz-Jeghers syndrome ) and CDH1 (E- cadherin ); however, its frequency and increased risk of breast cancer are not exactly known. The probability is moderately increased if the rare genetic changes with moderate penetrance exist ; these affect the following genes, among others: ATM ( Ataxia telangiectatica), CHK2 (checkpoint kinase 2) and BRIP-1 . Overall, no more than five percent of breast cancers can be traced back to these high or medium risk genetic changes.
The much more frequent allele changes with low penetrance increase the risk of breast cancer at most to 1.25 times for heterozygous changes and 1.65 times for homozygous changes. These include changes in FGFR2 (fibroblast growth factor receptor 2) and on chromosome 2q . It is estimated that such low penetrance mutations play a role in 58% of breast cancers.
The probability of developing the disease increases, statistically demonstrably, if there are two or more people with breast cancer in direct relatives. Families in which several people have breast or ovarian cancer are recommended to receive tumor genetic counseling in a counseling center, for example from the joint project on familial breast cancer of the German Cancer Aid .
In women with a corresponding predisposition (high probability of the occurrence of the disease), a bilateral prophylactic mastectomy ( mastectomy ) and / or an ovarian removal can be carried out on request : A certain protection against breast cancer seems to be provided by the extensive suppression of estrogen production by removing both ovaries. Various authors report a 50 to 70% reduction in the risk of developing breast cancer if the family has already developed breast cancer.
Hormonal factors
Human body cells, including tumor cells, carry receptors for the sex hormone groups estrogens and gestagens . Breast carcinomas with estrogen and / or gestagen receptors can be treated with endocrine therapy, e.g. B. Tamoxifen, are slowed in their growth. It is discussed whether estrogens and progestins influence the development of breast cancer. By blocking the estrogen receptor with tamoxifen, the frequency of breast cancer (incidence) could be reduced. It only lowered the incidence of breast cancers with receptors. Receptor-negative carcinomas were not affected. In addition to tamoxifen, raloxifene and exemestane can also lower the incidence of breast cancer. For clinical use, risks and side effects must be carefully weighed. Long-term hormone replacement therapy for menopausal symptoms using drugs containing estrogen and gestagen can increase the risk of the disease by up to 45%. In the Women's Health Initiative, the relative risk of breast cancer was 1.26 (confidence level 1.00-1.59) after postmenopausal use of estrogens and progestins. Even women with early menarche (first menstrual period during puberty ) and late menopause (end of menstruation, "menopause") carry a slightly higher risk of the disease , whereas women who have children early and breastfeed for a long time are at a lower risk.
The extent to which the contraceptive pill increases the risk is just as dependent on the substance and dose as it is with hormone replacement therapy and therefore cannot be generally quantified. However, the Nurses' Health Study and other studies were able to show a typical increase in risk of 1.2 to 1.4 times after taking the pill for more than five years.
According to a meta-analysis from 2004, termination of pregnancy does not increase the risk of breast cancer . Such a connection could not be proven in other studies with high case numbers either.
Phytoestrogens are phytonutrients with an estrogen-like effect. It is not known whether diets that are rich in such substances ( e.g. based on soy ) increase the risk of the disease or, on the contrary, reduce it by interacting with the body's own hormone production, as the results of scientific studies are contradictory.
Left handedness
A study in September 2005 that found that left-handed women were up to twice as likely to develop breast cancer before menopause as right-handed women sparked increased public interest. Another study had already come to a similar result five years earlier (risk increase + 42%). A study from 2007 even found that left-handed women were 2.59 more likely to have breast cancer.
The mechanisms for the increased risk of breast cancer in left-handed women are still largely unclear. One hypothesis that has been discussed in professional circles is that prenatal exposure of the embryo to increased doses of sex hormones is the cause. The sex hormones cause - according to the hypothesis - on the one hand, that the child becomes left-handed and, on the other hand, that the breast tissue changes and becomes more susceptible to cancer. Left-handedness is, so to speak, an indicator of increased concentrations of steroids in the uterus . The hypothesis that the basis for the development of breast cancer can be formed by the action of sex hormones in the embryonic stage has been discussed since 1990 and is based on the Geschwind-Behan-Gallura model . It was already shown in 1985 that sex hormones - especially testosterone - in utero can influence the development of handedness.
Left breast more common than right breast
Statistically, the left breast is more likely to be affected by breast cancer than the right, in both women and men. All populations are affected. The difference increases with age. This increased rate for the left breast obviously does not apply to tumors that originate in the upper outer quadrant. The probability that the left breast will develop cancer is - depending on the study - five to seven percent higher than that of the right. In men, this value is even ten percent.
The causes of this phenomenon are still largely unclear. Discussions include sleeping habits, handedness , differences in breast size and brain structures, and breastfeeding preferences . Another hypothesis sees the embryonic development of the heart on the left side of the body as a possible cause.
A similar statistical accumulation can be observed in other organs, such as the lungs and testicles. With these two organs, the right half of the organ is 13% more likely to be affected. In these cases this difference is explained by the mostly smaller tissue volume of the left half of the organ.
Other factors
Several other factors appear to have an effect on breast cancer development:
- Ionizing radiation at a young age increases the risk of breast cancer later on. Mammography examinations in women over 40 years of age do not lead to any significant increase in risk.
- Significantly overweight women fall ill 2.5 times as often as normal weight women.
- Heavy and long-term cigarette smoking increases the likelihood of illness by 30%.
- Women who drink at least 20 g of alcohol per day have a 30% higher risk of developing breast cancer, possibly because of the higher sex hormone levels.
- Low iodine intake could also play a role. In countries with high iodine content in the diet (e.g. Japan) there are significantly fewer cases of breast cancer than in iodine-deficient areas. In addition to this correlation, more specific metabolic relationships are suspected.
- In a survey in 2017, patients with breast cancer reported symptoms that are more characteristic of Flammer's syndrome than women in a (healthy) control group , especially cold extremities, pain sensitivity, impaired heat regulation (they freeze easily), and low blood pressure and reddish patches of skin.
- Another risk factor could be sun or vitamin D deficiency. When ( postmenopausal ) women take calcium and vitamin D to prevent bone fractures , their risk of developing the disease appears to be greatly reduced. These studies are very controversial. In some cases there seem to be clear signs of publication bias . In a 2013 meta-study , no significant association could be found between the intake of vitamin D and a reduced risk of breast cancer in postmenopausal women.
- For some years now, an active role of endothelin and endothelin-converting enzyme (ECE) in the development of breast cancer and in particular in the metastasis of breast cancer cells has been discussed.
- According to a cohort study, those who consumed a lot of red meat in young adulthood also have an increased risk of breast cancer.
- A lack of exercise increases the likelihood of illness in women by around 25%.
Breast cancer triggering through an infection (" breast cancer virus ") has not yet been proven. Breast implants do not cause breast cancer, and neither does wearing bras .
Protective factors
In addition to avoiding risk factors, there are also some protective behaviors against breast cancer.
These include:
- Omega-3 fatty acids from fatty fish: While longer observational studies have shown a clear effect, a new study shows that the protection is only minimal.
Early detection and screening
About 80 to 90% of all tumors in the female breast have so far been discovered by the women themselves. These palpable and visible tumors are often relatively large when they are discovered and are therefore usually associated with a poor prognosis. The consistent early detection of smaller, non-palpable tumors could, according to large studies, reduce mortality by 25%. Programs for systematic self-examination and breast ultrasound as well as screening mammography are used for early detection . The medical benefits of early detection are controversial. A meta-study published in 2013 in the Cochrane library of over 600,000 women found no survival benefit for women who participated in screening. This was also confirmed in a 2014 Canadian study of 45,000 women who had been followed for 25 years.
Self examination
Systematic training courses for women on breast self-examination are controversial in their benefits. Not every breast cancer causes a palpable tumor. Conversely, only about every twelfth self-felt change is malignant. According to studies, systematic breast self-examination does not reduce mortality. The US Preventive Services Task Force (USPSTF) does not give any recommendation for or against breast self-examinations due to insufficient data. The Canadian Task Force on Preventive Health Services issued a recommendation against self-examination in 2001 because the detection rate was poor and false positives were frequent.
To learn about self-examination, there are breast models made of silicone that contain different types of knots; accompanying video and instructions are attached. However, in Germany this is not a benefit from statutory health or long-term care insurance .
In Germany, self-examination is recommended by the medical societies because it helps to raise awareness among women and thus promotes the actual early detection by means of apparatus. The self-examination, which should be carried out monthly about five to seven days after the onset or shortly after the end of the menstrual period, follows a certain, repetitive pattern. If any abnormalities are felt, women should consult a specialist.
Medical early detection of cancer
The clinical examination of the breast by a doctor is part of the statutory cancer early detection program from the age of 30. In principle, the same restriction applies to the informative value of the medical palpation examination as to the self-examination.
Breast cancer early detection by the blind
Blind people usually have an above-average sense of touch . This special ability is used for the early detection of breast cancer. As part of in North Rhine-Westphalia settled model project "Discovering hands" (discovering hands) was the training course created the Medical Tastuntersucherin.
Imaging procedures
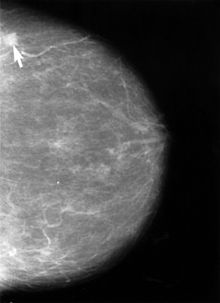
According to an S3 guideline from 2010, X-ray mammography is currently the only method generally recognized as effective for the detection of breast cancer precursors or early tumor stages. Magnetic resonance imaging may be superior, but it is too expensive for mass screening. In Germany, a quality-assured mammography screening program was therefore set up on the basis of the "European guidelines for quality assurance in mammography screening" for women aged 50 to 69. For this purpose, Germany was divided into 94 regions, for each of which a screening unit is responsible. In the USA there was a recommendation in 2002 to start mammography screening at the age of 40.
Triple diagnosis and additional diagnostics are intended to ensure that as few benign breast tumors as possible are biopsied or even removed. The EUREF guideline requires that malignant tumors can be detected in at least 50% of the tissue samples taken; in some examination programs up to 80% is achieved.
CAD systems (computer-assisted detection) can support the radiologist in evaluating the mammograms. Such examinations can be paid for by health insurance companies in the USA and the Netherlands. According to studies published so far, the devices available so far do not improve the detection rate. In the European screening programs, double diagnosis by two doctors (and by a third in case of abnormalities) is therefore preferred.
Mammography is limited in its informative value in women with dense glandular tissue. With extremely dense tissue, around 50% of breast tumors are not detected with mammography. This primarily affects younger women for whom sonography , and in individual cases magnetic resonance mammography , is recommended. After systematic literature research, the IGeL-Monitor (initiator and client: MDS (Medical Service of the Central Association of Health Insurance Funds)) rates the sonography (ultrasound) as “unclear”, the magnetic resonance tomography (MRT, nuclear spin) as “tends to be negative”. The IGeL-Monitor scientists found no studies in either case that examined the question of whether the studies could actually save women from dying from breast cancer. This applies to examinations in addition to mammography screening as well as an alternative to mammography screening. With MRI, damage from the contrast agent that is injected is possible. These ratings are for women aged 40 and over who are not at an increased risk of breast cancer.
Early detection through biomarkers (liquid biopsy)
At the beginning of 2019, a liquid biopsy method for early breast cancer diagnosis was published by Heidelberg University. In the meantime, the Heidelberg public prosecutor has started preliminary investigations. Uniklinikum and spin-off Heiscreen described the test as a “milestone” in early breast cancer diagnosis, despite the lack of data. Financial entanglements by doctors, but also by celebrities, are said to have favored the PR campaign.
On the basis of the innovative liquid biopsy method, it is possible to diagnose breast cancer non-invasively. The new method recognizes cancer using biomarkers from the blood . The test can be performed on women of all ages; Younger women under the age of 50 and women with a familial high-risk situation for breast cancer, for whom mammography provides little information, for example due to the dense breast tissue, or for whom conventional imaging methods are contraindicated due to other risk factors, benefit in particular . Current results have shown a sensitivity of 75 percent in 500 breast cancer patients. The Gynecological Oncology Working Group (AGO) of the German Cancer Society expressly welcomes research into liquid biopsy technology, but warns against premature application of the test. A scientific publication is not yet available. The clinical consequences of the test in relation to the results of other diagnostic procedures, e.g. B. Mammography and sonography must first be verified in studies.
diagnosis
Clinical examination
During the self-examination or during the medical, clinical examination , a new, indistinctly delineated tumor can be noticed. Other signs are hardening, changes in the size and shape of the breast when compared from the side, reduced movement of the breast when lifting the arms, permanent reddening of the skin, skin retraction or orange peel (thickened skin with retracted areas), retraction or inflammation of the nipple, secretions from the nipple. Nodes in the armpit can lymph nodes - metastases , respectively. General symptoms of very advanced diseases include: a. Loss of performance, unwanted weight loss or bone pain.
A breast carcinoma that has not been treated for a long time or a local tumor recurrence that cannot be controlled can expand lymphangitically or subcutaneously infiltrating to such an extent that the entire chest wall appears to be armored; this condition is known as cancer en cuirasse (crayfish).
Imaging diagnostics
If abnormalities are found during the palpation or ultrasound examination, the next examination is usually mammography: the X-rays are taken from two directions of view (from the side and from above); certain changes sometimes require additional images. The Galactography is performed only when the nipples secrete secretions. In addition, ductoscopy , a reflection of the milk ducts, is available at some centers for such a secretion .
Conversely, changes discovered with mammography are always further examined sonographically. This will detect benign cysts . The National Association of Statutory Health Insurance Physicians prescribes transducers with a frequency of at least 5 MHz .
The MRI of the breast (breast MR, MRI) is currently only recommended for invasive lobular breast cancer to determine the resection BOUNDARY and generally in the presence of several suspected tumor foci, if appropriate, an MRI guided biopsy is possible. After breast-conserving therapy, MRI can be used to distinguish between scarred densities in the operated breast and new tumor growth. In addition to outpatient care for patients with statutory health insurance, there are other indications.
The positron emission tomography is currently no routine method, but can be used to search for the primary tumor or its metastases, if this can not be found with other methods.
Bone scintigrams , computer tomographies , x-rays of the lungs, sonographies of the liver and, if necessary, magnetic resonance tomographies are used to search for metastases, i.e. to identify the spread of the disease. In view of the fact that PET / CT is more accurate except for the MRI brain and breast examinations and at the same time can also rule out other cancer diseases, PET / CT appears to be more useful than bone scintigrams, computed tomography, x-rays of the lungs and sonographies of the liver combined.
In the radiological diagnosis also can be a by exudate incurred pleural effusion , as can occur in breast cancer, more reliable than by percussion are detected.
Tissue sampling
If a tumor has been diagnosed with the ultrasound and the mammography, it is examined for its benign or malignant nature. For this purpose , several tissue samples are taken from each tumor using a punch biopsy , in rare cases using a vacuum biopsy and examined for cancer cells under the microscope. The method of choice for taking samples of palpable and sonographically visible findings is the punch biopsy, and for findings and microcalcifications visible in the magnetic resonance imaging, the stereotactically supported vacuum biopsy. If the tumor is recognized as malignant, the carcinoma is determined by further examinations of the removed tissue. This includes the status of the hormone and HER2 / neu receptors as well as the degree of degeneration .
After the surgery, the removed from the mammary gland is surgical specimen in the histological examination measured for its exact size and examined the tissue to further attack. The removed lymph nodes are checked for metastases. The size of the carcinoma and the number of affected lymph nodes are important for TNM classification , prognosis, and further treatment. The surgical specimen is also measured to determine whether the distance between the carcinoma and the remaining healthy tissue is sufficiently large. If this is not the case, a follow-up operation may be necessary so that an appropriate safety margin is achieved between healthy and diseased tissue.
Gene expression tests
There are now a number of gene expression tests for patients with early and hormone-receptor-positive breast cancer. They examine the activities of various genes ( gene expression ) in tissue samples from a breast cancer tumor and thus help to differentiate between those patients who can benefit from adjuvant chemotherapy and those patients who can be spared this therapy, which has many side effects. The most important gene expression tests for breast cancer are the EndoPredict , Oncotype DX and MammaPrint .
classification
The classification of a tumor is its exact description based on the pathological examination of a tissue sample or the surgical specimen and the lymph nodes removed.
Histological classification
Source:
The most common type of breast cancer is an adenocarcinoma with no special features, accounting for around 70–80%; this type of tumor is known as invasive ductal carcinoma (IDC). Invasive lobular carcinoma (ILC), invasive tubular, mucinous, medullary, papillary carcinoma (each about 2%), mixed and other tumor types are less common (around 10–15%) . These tumor types differ in their clinical presentation, the findings on imaging examinations, the histological spread pattern and in the prognosis. Almost all tumor types also have a non-invasive (ductal or lobular) tumor component from which they arose and which is one of the decisive factors for the size of the operation. Rare breast cancer goes straight from benign diseases produced (some of which in mammary tumor are mentioned, but not is here to malignant tumors).
As inflammatory breast cancer is referred to no histologic type of tumor, but a visible and tactile change, namely, a redness of at least one third of the breast skin and swelling of the breast by infiltration of the lymphatic system. Usually there is a locally advanced involvement of the breast and the surrounding lymphatic system.
Non-invasive carcinomas are defined as carcinomas within the mammary ducts ( ductal carcinoma in situ , DCIS) or lobules ( lobular carcinoma in situ , LCIS or lobular neoplasia, LN) without stroma invasion. Paget's disease of the nipple (nipple) occupies a special position , which is based on a non-invasive spread of tumor into the nipple skin and is usually associated with intraductal breast cancer, more rarely with invasive breast cancer. This Paget's carcinoma of the nipple can clinically be mistaken for eczema or benign ulcer .
Degree of differentiation
The histological tumor types are divided into three degrees of differentiation (synonym for degree of malignancy , also grading ) on the basis of structural and cellular properties as well as their core division rate . The classification of invasive carcinoma is based on the three criteria tubule formation (formation of tube-like tumor glands), nuclear polymorphism (diversity of cell nuclei) and mitotic rate (rate of division of cells) according to Elston and Ellis. The higher the grading, the less favorable the behavior of the tumor cells. A distinction is made between tumors with a degree of differentiation 1, 2 or 3 (G1 = well differentiated, G2 = moderately differentiated, G3 = poorly differentiated).
TNM classification
The TNM classification describes the size of the tumor (T), the number of affected lymph nodes (N) and any distant metastasis (M). The tabulated short version of the TNM classification for breast cancer:
|
|
|
||||||||||||||||||||||||||||||||||||||
Staging
From the TNM classification (or pTNM classification, the "p" stands for histologically confirmed data) of breast cancer, the stage grouping according to UICC or AJCC (TNM 6th edition. 2003) results as follows:
| Stage 0 | Tis | N0 | M0 |
| Stage I. | T1 | N0 | M0 |
| Stage IIA | T0, T1 | N1 | M0 |
| T2 | N0 | M0 | |
| Stage IIB | T2 | N1 | M0 |
| T3 | N0 | M0 | |
| Stage IIIA | T0, T1, T2 | N2 | M0 |
| T3 | N1, N2 | M0 | |
| Stage IIIB | T4 | N0, N1, N2 | M0 |
| Stage IIIC | Every T | N3 | M0 |
| Stage IV | Every T | Every N | M1 |
Hormone receptor and HER2 status
The estrogen receptor and progesterone receptor status (ER and PgR expression) is also examined histologically, more precisely immunohistologically . The percentage of those tumor cells on which the receptors can be detected is determined and a 12-point immunoreactive score (IRS), or the internationally more common 8-step Allred score, is calculated from the percentage and the staining intensity .
| Color intensity (IS) | Positive cells (PP) | ||
|---|---|---|---|
| 0 | no reaction | 0 | no |
| 1 | weak response | 1 | less than 10% |
| 2 | moderate response | 2 | between 10 and 50% |
| 3 | strong reaction | 3 | between 51 and 80% |
| 4th | more than 80% | ||
| IRS | |
|---|---|
| 0-2 | negative |
| 3-4 | weak positive |
| 6-8 | moderately positive |
| 9-12 | strongly positive |
For the HER2 receptor , which is used to decide whether a follow-up treatment with trastuzumab (also in combination with pertuzumab and docetaxel ) is useful, a 4-point score is used that is based on the immunohistochemical staining intensity (ASCO recommendation 2007). If no cells can be stained, the result is negative: Score 0. Score 1+ is also negative, i.e. H. treatment with trastuzumab would have no effect on the tumor. If the staining intensity is medium (score 2), the tumor is re - examined with the FISH test and a decision is made on the basis of the amplification of the HER2 gene whether it is a HER2-positive tumor.
| Positive cells | Membrane staining | Staining intensity | Score |
|---|---|---|---|
| no | no | no | 0 |
| 1% or more | incomplete | weak | 1+ |
| less than 10% | Completely | weak to moderate | 1+ |
| 10% or more | Completely | weak to moderate | 2+ |
| 30% or less | Completely | strong | 2+ |
| more than 30 % | Completely | strong | 3+ |
Risk groups, classification according to the results of the consensus conferences in St. Gallen
The consensus conference held every two years in St. Gallen deals primarily with adjuvant therapy. In order to be able to use chemotherapy and hormone therapy as targeted as possible, following the recommendation from 2007, the operated patients are divided into three risk, better treatment groups:
| Low risk | Medium risk | High risk | |
|---|---|---|---|
| Number of affected lymph nodes: |
none and all of the following criteria: | 1 to 3 or none, but at least one additional criterion: |
more than 4 or 1 to 3 and |
| Tumor size: | T1 (max. 2 cm) | T2 to T4 (larger than 2 cm) | |
| Differentiation: | G1 | G2 and G3 | |
| Tumor invasion: | Invasion into vessels | ||
| Hormone status : | ER / PR positive (estrogen / progesterone positive) | ||
| HER2 / new status: | HER2 / neu negative | HER2 / neu positive | HER2 / neu positive |
| Age: | 35 years and older | or younger than 35 years |
Molecular tumor classification
On the basis of the gene expression profile, which can be obtained from the tumor tissue with DNA microarrays , one can differentiate between five main groups of breast cancer: Hormone receptor-positive tumors with less or more aggressiveness (called Luminal-A and Luminal-B , from lumen = cavity of the milk ducts) , HER2-positive tumors (erbB2 phenotype) and hormone receptor and HER2-negative carcinomas with or without basal cell properties ( basal-like and normal-like phenotypes). The currently still experimental molecular tumor classification could enable a better assessment of the prognosis and the likely effect of adjuvant hormone and chemotherapy in the future.
Gene expression analysis
A central question in the treatment of operable breast cancer is the question of how high the risk of the disease recurring (risk of recurrence) is. Patients with a high risk of recurrence should receive adjuvant chemotherapy, while patients with a low risk should be spared chemotherapy, which has many side effects. The estimate of the risk of recurrence, which was used in the past and based on purely clinical factors such as tumor size, menopausal status, age, etc., has proven to be inaccurate. Some patients classified as "low risk" still suffer a relapse. On the other hand, it is believed that many chemotherapies are given unnecessarily; H. many patients would be cured without one.
In order to enable a more precise prediction of the risk of recurrence, so-called gene signatures have been developed with the aim of predicting the risk of the disease recurring more precisely. The gene expression of a number of genes in the tumor tissue is measured and a point value (risk score) is calculated, which should indicate the risk of a relapse. From a certain point value onwards, chemotherapy is recommended.
Four commercial gene expression tests were available in July 2019. All four tests were evaluated in clinical trials for early-stage breast cancer.
|
Oncotype DX (Genomic Health) |
Mammaprint (Agendia) |
EndoPredict (Myriad) |
ProSigna (nanostring) |
|
|---|---|---|---|---|
| Number of genes | 21st | 70 | 11 | 50 |
| tumor | HR +, HER2- | HR +/-, HER2- | HR +, HER2- | HR +, HER2- |
| Menopausal status | pre and post | pre and post | pre and post | only post |
| Nodal status | N0 | N0, N + | N0, N + | N0, N + |
| evidence | TAILORx study (9 years prospective) |
MINDACT study (5 years prospective) |
prospective-retrospective data from various studies | prospective-retrospective data from various studies |
- ↑ HR + / HR-: hormone receptor positive / negative, HER2-: HER2 negative
- ↑ premenopausal: patient is before menopause, postmenopausal: patient is in or after menopause
- ↑ N0: no lymph node (nodal) involvement, N +: with lymph node involvement
According to a decision by the Federal Joint Committee (GBA) on June 20, 2019, the costs of the Oncotype DX gene expression test will in future be reimbursed by the statutory health insurance companies (standard benefit).
therapy
To standardize and improve patient care , breast centers in hospitals certified by OnkoZert on behalf of the German Cancer Society and the German Society for Senology have existed in Germany since 2003, and a disease management program for breast cancer in which resident doctors can also participate since 2004 . The common guideline of level S3 of the German Cancer Society and the medical societies is the orientation for the treatment of breast cancer for these programs. This guideline is updated regularly, most recently in February 2020.
The strategy for breast cancer treatment is usually planned as part of a tumor conference in which gynecologists , internal oncologists , radiologists , radiation therapists and pathologists take part. The involvement of the patient in the decision-making process is of great importance, as with any interventional medical measure (see informed consent ). The German legislator also speaks clearly of the status of the informed patient in the DMP directive .
The treatment of breast cancer is intended to cure the disease in the early stages, to extend the life of metastatic carcinoma and to alleviate the symptoms of the disease in the later stages. When choosing a specific therapy, the focus is on maintaining quality of life. Therefore, in addition to the tumor classifications described above, the patient's physical, psychosocial and emotional situation is also taken into account. There is no such thing as a “standard therapy”; the consideration of all the various factors leads to an individual adaptation of the therapy to the disease and the respective patient.
Breast cancer can spread very quickly in the body and is therefore treated with systemic therapy (effective throughout the body) at an early stage . This “Fisher Doctrine”, named after the American surgeon Bernard Fisher , is the basis of chemotherapy and hormone therapy for breast cancer. Today treatment almost always consists of a combination of different forms of therapy. If additional measures are carried out before an operation, they are called neoadjuvant , if they are used after an operation, they are called adjuvant .
Neoadjuvant Therapy
In some cases, chemotherapy or anti-hormonal therapy is carried out before the tumor is surgically removed. This primary or neoadjuvant therapy aims, on the one hand, to reduce the size of the tumor in order to enable complete removal of the tumor or even a breast-conserving operation; on the other hand, the success of a further adjuvant treatment can be assessed on the basis of the change that can be achieved with the neoadjuvant treatment. Standard is the neoadjuvant therapy for inflammatory carcinoma and for initially inoperable (T4) tumors. The chemotherapy regimens are the same as for postoperative treatment (see below).
surgery
Breast cancer surgery has two objectives: on the one hand, by removing the degenerated cells as completely as possible, the tumor cells should be prevented from spreading (metastasis) to other parts of the body, if this has not yet happened, and on the other hand, the signs of the disease should reappear on the spot ( a relapse ) can be prevented.
Breast-conserving surgery vs. Mastectomy


Breast-conserving therapy (BET) is now possible in 60–70% of patients if the relationship between tumor size and breast volume is favorable and the tumor has not yet penetrated the muscles or skin. During this operation, either the tumor and the surrounding tissue ( lumpectomy ), a larger segment, or an entire quadrant ( quadrantectomy ) is removed. In order to obtain a cosmetically appealing result, a so-called intramammary displacement plasty is carried out in the case of larger tissue removal, especially from both lower quadrants . The mammary gland is completely or partially detached from the skin and muscles and moved in such a way that a balanced breast shape is maintained after the operation despite the loss of tissue. If relocation plastic surgery is not possible, the breast can either be reconstructed immediately after the tumor has been removed or after all treatments have been completed.
If it is not possible to preserve the breast, the entire mammary gland and part of the overlying skin are removed ( ablation , mastectomy ). The recommendation for a mastectomy is given if:
- the tumor is very large (> 3 cm) or has infiltrated the pectoral muscle,
- an inflammatory carcinoma has been diagnosed
- extensive involvement of the lymphatic vessels of the mammary gland has been demonstrated,
- the tumor has formed extensive "arms" in the milk ducts ( ductal in situ carcinoma ),
- the entire mammary gland contains microcalcification detected by mammography,
- the tumor could not be removed with a sufficient safety margin to the healthy tissue despite reoperation,
- the patient wishes this. Some patients decide against the option of breast-conserving surgery in order to feel safer or to avoid the otherwise necessary radiation therapy.
The recommendation for a mastectomy is also given if a multicenter (tumor nodule in several quadrants) or multifocal (several tumor nodules in the same quadrant) carcinoma has been diagnosed. This recommendation can sometimes be put into perspective if the surgeon can remove all tumors with a sufficient safety margin from healthy tissue. Even if a cancer has already metastasized to other organs, the original tumor can be operated on more gently if the radical surgical procedure would not bring any advantage.
Breast prostheses and breast compensation parts made of silicone are used for the care of women both after mastectomy and after breast-conserving surgery (surgery) or after reconstruction with an inadequate cosmetic result. Women after breast surgery are usually entitled to a breast prosthesis (also called breast epithesis) or a breast compensation part, the costs of which, including advice and adjustment, are then covered by the health insurance companies as a medical aid. As a holder for the prosthesis, there are special prosthetic bras and prosthetic swimsuits with integrated pockets, which are available from medical supply stores together with the breast compensation.
Axillary lymph nodes
The armpit lymph nodes are usually the first place where metastases develop. In order to record this infestation, the lymph nodes, at least some of them, are often removed during the operation.
In order to keep the consequential damage ( lymphedema ) as low as possible, only a single lymph node can initially be removed and examined if the tumor in the breast is smaller than 2 cm and the axillary lymph nodes cannot be felt. For this purpose, a dye or a radionuclide is injected into the breast concerned in order to show the lymphatic drainage. The first lymph node in which the injected material can be detected is removed and examined. Only when these so-called sentinel lymph nodes (sentinel node) is afflicted with tumor cells, more lymph nodes in the armpit are also removed (partial or complete axillary dissection ).
Non-invasive tumor destruction
In 2013, a procedure was first tested in Rome in which tumor tissue can be destroyed non-invasively by means of ultrasound waves during outpatient treatment. In the subsequent operation, no tumor residues could be found in 10 of 12 patients with tumors smaller than 2 cm. However, the process still needs to be tested and optimized.
Adjuvant therapy
Almost all patients receive adjuvant (supportive) treatment after the operation .
chemotherapy
After the operation, many patients with a higher risk of relapse are followed by chemotherapy to kill any remaining tumor cells. The need for chemotherapy is assessed based on the type of tumor, stage, and other factors. If the tumor is hormone-dependent, smaller than 2 cm and the lymph nodes are free of metastases, chemotherapy can be dispensed with in most cases. With this constellation, anti-hormonal therapy can achieve similar results (St. Gallen 2007).
Which chemotherapy is administered depends on the patient's condition and on the classification of the tumor, especially on the risk group according to the St. Gallen recommendation. The treatment is carried out in several cycles, for example a total of four times with an interval of three weeks or six times with an interval of two weeks. The time interval between the individual doses is intended to give the body the opportunity to regenerate on the one hand, and on the other hand it is hoped that micrometastases (dormant tumor cells) or cancer stem cells start dividing during the recovery phases and can be destroyed when the cytostatic drugs are administered again.
As a rule, the cytostatics are used as combinations. The most common schemes currently are AC or EC, FAC or FEC. If the lymph nodes are infected with metastases, supplementing the respective combination with taxanes ( paclitaxel and docetaxel ) is recommended (St. Gallen, 2007). The older CMF scheme is hardly used anymore. (A = adriamycin , C = cyclophosphamide , E = epirubicin , F = fluorouracil , M = methotrexate , T = taxanes ) In the meantime, chemotherapies have also been successfully combined with other therapies such as targeted antiangiogenesis ("Therapy of metastatic breast cancer", see below).
Since July 2019, the statutory health insurance companies have also covered the costs of a gene expression test that can be used to answer the question of whether adjuvant chemotherapy is necessary in the early stages of an operated breast cancer (→ gene expression analysis ).
HER2 / neu positive tumors
To reduce the risk of the disease recurring ( relapse ), HER2 / neu positive tumors are usually treated with the HER2 antibody trastuzumab for one year after chemotherapy ("Antibody therapy", see below) ), more rarely without prior chemotherapy. The duration and the composition of the chemotherapy are determined by the extent of the affected lymph nodes (St. Gallen 2007). After trastuzumab treatment, neratinib can be used for the same purpose.
Irradiation
After the breast-conserving operation, radiation therapy should be given to the breast. It lowers the recurrence rate from 30% to less than 5%. Microscopic remnants of tumors (not visible to the naked eye) can remain in the mammary gland even with the most careful surgery.
Post-irradiation is also recommended after a mastectomy if the tumor was larger than 5 cm (T3 or T4), the mammary gland contained several tumors, or the tumor had already penetrated the skin or muscles. Infection of lymph nodes is also a reason for re-irradiation of the chest wall, especially if more than three lymph nodes are affected.
In women under 60 years of age, the former tumor area should be irradiated with a dose that is 10-16 Gy higher so that no recurrences can develop at the incision margins.
Radiation therapy begins around 4-6 weeks after the operation and lasts six to eight weeks. A feared increase in coronary events as a long-term consequence of the radiation effect on the heart could not be confirmed, there is a certain increase in risk, but the absolute risk is very low and can possibly be further reduced with modern radiation therapy.
Anti-hormonal therapy
If the carcinoma is hormone-sensitive, therapy with hormone antagonists is also carried out. There are different variants depending on the menopausal status of the woman and the exact type of tumor.
Before menopause
Surgical ovariectomy or radiotherapeutic deactivation of ovarian function is rarely performed. According to studies, a temporary shutdown of hormone production over two years is sufficient, which can be achieved with medication.
In women who are still having their periods, chemotherapy already disrupts the hormonal function of the ovaries. This effect is also directed against the hormone-dependent tumor cells and is therefore desirable. Women who want to have children or women who are at risk of premature menopause can protect their ovaries from the damaging effects with GnRH analogues (which suppress the ovarian production of estrogen and progesterone ) and at the same time switch off hormones . GnRH analogues are usually given for two years.
After chemotherapy, an estrogen receptor modulator such as tamoxifen , which prevents the body's own estrogen from binding to the tumor's estrogen receptors , is usually given for 5 years. Aromatase inhibitors are not indicated before menopause.
After menopause
If the patient is postmenopausal, she is given either tamoxifen or an aromatase inhibitor, which blocks the formation of estrogen in muscle and fat tissue for five years, as a rule. More recent study results indicate that the aromatase inhibitors are more effective than the tamoxifen, that is, the disease-free survival time increases. In studies, the aromatase inhibitor is sometimes used immediately (upfront) , usually only after two to three years on tamoxifen ( switch , dt. 'Change'), or after five years (extended) . The respective side effects of the substances must be taken into account in the decision. Due to their better effectiveness, aromatase inhibitors are the first choice at the start of therapy and are accordingly prescribed more frequently. Tamoxifen, on the other hand, has been prescribed less and less since 2003. Another possibility is the administration of a pure estrogen receptor antagonist ( fulvestrant ; trade name Faslodex), which, however, has only been approved by the drug authorities for advanced breast cancer.
In many patients with hormone-dependent tumors, tamoxifen loses its protective effect after a few years (so-called tamoxifen resistance ). According to laboratory tests, on the contrary, cell growth can even accelerate. Affected women should be treated better with other substances. However, it is not yet possible to predict the behavior of an individual tumor in this regard. An indication could be the simultaneous occurrence of HER2 / neu and AIB1 expression in an ER-positive tumor.
Androgen receptor dependent tumor types
Most breast cancers also have receptors for the male sex hormone testosterone and other androgenic hormones. For ER + tumor types, the proportion of AR + tumors is stated to be over 80%, for “triple-negative” tumor types ( triple-negative breast cancer , TNBC) the proportion is estimated at around 10–50%.
Depending on the estrogen receptor status, testosterone can have a growth-inhibiting effect in ER + tumors or a growth- inducing effect in ER- / PR tumor types. The androgen receptor also partially reacts with other androgen hormones and progestins .
The treatment with the antiandrogen bicalutamide was tested with good success in a phase II study between 2007 and 2012, especially for AR + / ER- / PR- tumor types in locally advanced or metastatic stages .
Since the patent protection of Bicalutamide (Casodex) has expired, the newer enzalutamide is now being tested for this area of application, but so far only in vitro experiments are known.
The use of testosterone in ER + tumor types has also been historically proven; the results achieved were roughly comparable to tamoxifen, but associated with stronger side effects. A similar mechanism of action is suspected in part in the experimental treatment with progestins.
antibody
About a quarter of all breast cancers show overexpression of the HER2 / neu receptor. The detection of this receptor stands for an aggressive course of the disease and an unfavorable prognosis, but is also a condition for treatment ( cancer immunotherapy ) with the antibody trastuzumab . In addition to the administration of trastuzumab alone, it is also used in combination with the monoclonal antibody pertuzumab and the cytostatic drug docetaxel .
In 1998 the active ingredient (trade name: Herceptin ) was approved in the USA and in 2000 in the European Union, initially for patients with metastatic breast cancer. Trastuzumab is a monoclonal antibody against the growth receptor HER2 / neu on the cell surface of cancer cells. Studies have shown that with these so-called targeted cancer therapy (targeted therapy) could be the risk of recurrence (recurrence) reduced by about 50%. Many clinical studies show that women without metastases also benefit. HER2 antibody therapy can prevent relapses and thus contribute to healing. Trastuzumab has therefore also been approved for adjuvant therapy since 2006.
Therapy of metastatic breast cancer
Distant metastases worsen the prognosis rapidly, since multiple micrometastases are usually present in the presence of a visible distant metastasis. Therefore, the treatment is aimed at extending the life span and maintaining an adequate quality of life with a long-term stabilization of the physical and psychological condition. Breast cancer very often forms bone metastases .
Relapses and metastases can be surgically removed or treated with radiation therapy. Despite the side effects, administration of chemotherapy, hormone therapy or targeted cancer therapy can under certain circumstances improve the quality of life and extend the time until the disease progresses ( progression-free survival ). Paclitaxel albumin (trade name: Abraxane ), a member of the taxane group , is indicated - in monotherapy - for the treatment of metastatic breast cancer in adult patients who have failed first-line therapy for metastatic disease and are not indicated for standard anthracycline-containing therapy is.
In addition to the active ingredients used in adjuvant therapy, the tyrosine kinase inhibitor lapatinib is also used in HER2 / neu-positive metastatic breast cancer . Metastatic HER2 / neu-negative tumors have been treated with the angiogenesis inhibitor bevacizumab since 2007 . This targeted cancer therapy can be used in combination with chemotherapy consisting of paclitaxel or docetaxel. Studies on further possible combinations are currently ongoing. By the anti-angiogenesis triggered by the tumor formation of blood vessels is inhibited. As a result, the tumor is no longer adequately supplied and the tumor cells are said to perish.
Eribulin (trade name: Halaven ) is a non-taxane-based, highly effective new cytostatic agent (approval in the USA in November 2010; in Europe in March 2011) that is used in monotherapy for the treatment of heavily pretreated patients with locally advanced or metastatic breast cancer.
When the cancer has progressed so far in its spread that it can no longer be pushed back, treatment focuses primarily on controlling pain and other ailments. For palliative care includes psychosocial care and pain management , which should be done quickly and completely, and early and adequate administration of opiates including, see WHO pain ladder .
Aftercare
Follow-up care for treated patients usually lasts five years and is mostly based on the guidelines of the German Cancer Society. Particular attention must be paid to the side effects of radiation therapy (lymphedema, lung or heart problems), chemotherapy (changes in the blood count, organ damage) and hormone therapy (thrombosis, osteoporosis). In addition to the questioning and clinical examination, a mammogram should be taken every six months for the first three years, since this is where most recurrences occur. From the fourth year onwards, the mammography is carried out annually - as is the case with the second, healthy breast from the beginning. According to the S3 guideline, the patient no longer returns to a two-year interval or to the screening program. To monitor the progress, the tumor markers CA 15-3 and CEA can be determined in the blood test , but this is not provided for in the guidelines and is usually more the case if there is a specific suspicion. It must be considered very carefully for each individual patient whether the follow-up care should actually be carried out in the form specified here; every small, proven change can result in considerable psychological stress, which in turn can have a decisive influence on the quality of life.
Physical activity is also helpful as an accompanying healing method for rehabilitation after breast cancer and subsequent successful treatment.
The German statutory health insurances have been offering the disease management program "Breast Cancer" since 2004 to ensure uniform quality in follow-up care . The participating physicians orient themselves during therapy to the current guidelines for treatment and follow-up care for breast cancer. Participation is possible with all doctors who have joined these quality assurance programs. For the patients, participation in this program means a restriction of the free choice of doctor.
history
The first documentation of breast cancer is from the time of 2650 BC. From ancient Egypt . At that time they were treated with a branding iron. In the Edwin Smith Papyrus (around 1600 BC) eight breast cancers were described, including that of a man, which were also treated by cauterization . The Ebers papyrus also contains a description of breast cancer. The diseases were considered incurable at the time.
The case of breast cancer was also described in the Corpus Hippocraticum . Surgical treatment of deep-seated tumor diseases was not advised there, as patients who had not been operated on lived longer.
The Greek doctor Galen saw breast cancer as a result of a fluid disorder and thus as a systemic disease , a disease of the whole organism. Up to the Middle Ages, a wide variety of formulations were used as a treatment to liquefy and remove the thickened bile. Components were, among other things, lead and zinc carbonate , rose oil and deer droppings .
The first surgery for breast cancer is said to have been performed by Leonidas from Alexandria around 100 AD. He used a branding iron to stop the bleeding and remove tumor residues. Around 1543, Andreas Vesalius recommended removal of the breast (mastectomy) for breast cancer, in which he preferred hemostasis with sutures to cautery.
The French surgeon Jean-Louis Petit (1674–1750) presented the first concept for the surgical treatment of breast cancer, but it was only published 24 years after his death. His colleague Henry François Le Dran (1685–1770) said in 1757 that breast cancer, at least initially, was local in nature. Only when it has made its way into the lymphatic system is the prognosis for the patient bad. He therefore removed the entire breast, including the armpit lymph nodes . The Scottish surgeon Benjamin Bell (1749–1806) also recognized the importance of removing the lymph nodes from the armpit.
Rudolf Virchow (1821–1902) was able to prove in 1840 that the disease develops from the epithelial cells and spreads along the fasciae and lymphatic tracts. This changed the view of breast cancer, which was now viewed more as a local disease.
This concept was followed by William Stewart Halsted (1852-1922), who in 1882 performed the first radical mastectomy with removal of the fascia, the chest muscles ( pectoralis minor , pectoralis major ) and the axillary lymph nodes. For the circumstances at the time, this enabled local tumor control with a 5-year local recurrence rate of six percent. In German-speaking countries, Josef Rotter (1857–1924) was a pioneer of this method, which he carried out on his patients from 1889 onwards.
In 1874, the English surgeon James Paget (1814-1899) described an eczema-like change in the nipple with an adjacent ductal adenocarcinoma, which was later referred to as Paget's disease .
The Scottish surgeon Sir George Thomas Beatson discovered in 1895 that the removal of the ovaries in one of his patients shrunk the breast tumor. Breast cancer was irradiated for the first time in 1897. In 1927 the first breast-conserving operation for breast cancer was reported in Germany.
In 1948 David H. Patey and WH Dyson published a somewhat less radical surgical method than Rotter and Halsted with equally good results, in which the chest muscles could be preserved. It is still known today as a modified radical mastectomy according to Patey. A further decline in operative radicalism began with Robert McWhirter, who performed radiation therapy in 1948 after a simple mastectomy.
With the work of Bernhard and ER Fisher, the view prevailed in the 1960s that breast cancer can be a disease that is spread throughout the body even in its early stages and that the lymph nodes do not represent a barrier against spreading in the body. Rather, the involvement of the lymph nodes was viewed as an indicator of systemic spread. The removal of the lymph nodes would therefore only have prognostic and no therapeutic significance. For this reason, the current concept of surgery and radiation therapy was supplemented by subsequent chemotherapy in order to also destroy micrometastases. From 1969 chemotherapy took place as a combination of several preparations with an improvement in effectiveness.
Since the 1970s, breast cancers have increasingly been operated on in a breast-conserving manner. Since the end of the 20th century, the removal of sentinel or sentinel lymph nodes has often spared the need to completely remove the lymph nodes from the armpit. This further reduced the operational radicalism.
In 1990, a group of researchers led by the American JM Hall discovered the breast cancer gene , later named BRCA1 . In 1994, BRCA2, a second breast cancer gene, was recognized.
The Breast Cancer Month October initiative launched in 1985 by the American Cancer Society is attracting growing attention in developed countries. In 2011, the BRA Day was launched.
Breast cancer sign in art
The medical literature has repeatedly discussed signs of breast cancer in historical images. Signs such as an emerging tumor, changes in the size and shape of the breast compared to the sides, reddening of the skin, skin retraction or orange peel can be found in works by Raffael , Rembrandt van Rijn and Rubens , for example . However, whether the changes shown are actually breast cancer cannot be proven and has therefore been questioned.
- Examples of breast cancer signs in art
literature
Guidelines
- Interdisciplinary S3 guideline for the early detection, diagnosis, therapy and follow-up care of breast cancer. Version 4.1 - September 2018. AWMF registration number: 32-045OL. Publisher: Oncology guideline program of the Working Group of the Scientific Medical Societies in Germany (AWMF), the German Cancer Society (DKG) and the German Cancer Aid (DKH). Leading professional societies: German Society for Gynecology and Obstetrics (DGGG) long version , short version
- AGO guideline ( Working Group on Gynecological Oncology ): Recommendations for gynecological oncology, Commission Mamma Guideline 2018
- ESMO guidelines ( European Society of Medical Oncology ): E. Senkus, S. Kyriakides, S. Ohno, F. Penault-Llorca, P. Poortmans, E. Rutgers, S. Zackrisson, F. Cardoso on behalf of the ESMO Guidelines Committee: Primary breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. In: Annals of Oncology. Volume 26, Supplement 5, September 1, 2015, pp. V8 – v30.
- NCI guidelines ( National Cancer Institute , USA): version for patients , version for healthcare professionals
- NCCN guideline (National Comprehensive Cancer Network, USA). William J Gradishar, Benjamin O Anderson, Ron Balassanian and others: NCCN Guidelines Insights Breast Cancer, Version 1.2017. Featured Updates to the NCCN Guidelines. In: Journal of the National Comprehensive Cancer Network. Volume 15, Issue 4, 2017, pp. 433–451.
Textbooks
- David J. Winchester, David P. Winchester, Clifford A. Hudis, and Larry Norton (Eds.): Breast Cancer (Atlas of Clinical Oncology) . BC Decker, Hamilton, Ontario 2006, ISBN 1-55009-272-3 ( limited preview in Google Book Search).
- Orlando Silva, Stefano Zurrida (Ed.): Breast Cancer: Diagnostics and Therapy . Urban & Fischer, Munich 2007, ISBN 3-437-24260-1 ( limited preview in Google book search).
- Anne C. Regierer, Kurt Possinger: Breast cancer: Manual diagnostics and therapy . Deutscher Ärzte-Verlag , 2005, ISBN 3-7691-0487-0 ( limited preview in the Google book search).
- Manuela Eicher, Sara Marquard (Ed.): Breast cancer. Textbook for Breast Care Nurses, Nurses, and Health Professions . Huber, Bern 2008, ISBN 978-3-456-84556-2 .
counselor
- Hermann Delbrück: Breast cancer - advice and help for those affected and their families . 8th edition. Kohlhammer, Stuttgart 2009, ISBN 978-3-17-020469-0 .
- Heinrich Schmidt-Matthiesen , Gunther Bastert , Diethelm Wallwiener (eds.): Gynecological oncology . 7th edition. Schattauer, Stuttgart 2002, ISBN 3-7945-1974-4 .
- Various information brochures on breast cancer from the German Cancer Society . 2019 ( krebsgesellschaft.de [PDF]).
- Clemens Unger: Metastatic Breast Cancer: Patients Ask - Doctors Answer . Georg Thieme Verlag, Stuttgart 2004, ISBN 3-13-133561-0 ( limited preview in the Google book search).
- Marius Wunderle: Familial breast and ovarian cancer . Specialist consultation hour. W. Zuckschwerdt, Munich 2019, ISBN 978-3-86371-244-0 .
Documentation
- Renate Zeun : Affected - pictures of cancer . Verlag Volk und Gesundheit, Berlin 1990, ISBN 3-333-00380-5 . (Renate Zeun studied photography when she developed breast cancer and had to undergo an operation. This book contains her thesis with her own photos of her disease and how she dealt with it)
Web links
- Breast cancer - information at Gesundheitsinformation.de (online offer of the Institute for Quality and Efficiency in Health Care )
- Breast Cancer Patient Guideline: The First Disease and DCIS - A Guideline for Patients . (PDF; 0.48 MB) German Cancer Society
- Breast cancer patient guidelines: advanced disease, relapse and metastasis (PDF; 1 MB) German Cancer Society
- Overview of national, European and international breast cancer guidelines Breast Cancer Action Germany
- Breast cancer ( Memento of November 13, 2012 in the Internet Archive ) (PDF; 860 kB) - the blue guide No. 2 of the German Cancer Aid Foundation
- Breast cancer patient guide (PDF; 1.5 MB) German Cancer Society
- Female sexuality in breast cancer (PDF; 812 kB) Swiss Cancer League
- Breast cancer. Cancer information service of the German Cancer Research Center (DKFZ), Heidelberg
- Breast cancer patient information. Internet portal of the German Cancer Society
- Decision-making aids: breast cancer - what comes after? and breast-conserving therapy or breast removal? AOK
- Breast cancer information. Center for cancer registry data at the Robert Koch Institute
Individual evidence
- ↑ MA Roubidoux: Breast cancer, male. In: Emedicine. As of September 24, 2008.
- ↑ K. Rhiem, RK Schmutzler: Risk factors and prevention of breast cancer. In: Oncologist. Volume 21, 2015, pp. 202-210. doi: 10.1007 / s00761-014-2837-5
- ↑ a b c d e https://www.krebshilfe.de/informieren/presse/neues-aus-der-forschung/brustkrebs-neue-therapie-mit-cholesterinsenkern/ accessed on October 10, 2019
- ↑ Alexander Katalinic, Carmen Bartel: Epidemiologie Mammakarzinom. University of Lübeck, 2006. ( krebsregister-sh.de ( Memento from October 6, 2007 in the Internet Archive ))
- ^ WHO / IARC: World Cancer Report. Lyon 2003 ( Memento of February 1, 2008 in the Internet Archive )
- ↑ J. Eucker, P. Habbel, K. Possinger: Metastatic breast carcinoma: Differentiated, as targeted as possible drug therapy. In: Oncologist. Volume 19, 2013, pp. 487-493. doi: 10.1007 / s00761-013-2450-z
- ↑ Breast cancer leading cause of death in women. In: Doctors newspaper . September 1, 2008.
- ^ RH Johnson, FL Chien, A. Bleyer: Incidence of breast cancer with distant involvement among women in the United States, 1976 to 2009. In: JAMA . Volume 309, Number 8, February 2013, pp. 800-805, doi: 10.1001 / jama.2013.776 . PMID 23443443 .
- ↑ a b Compilation of the data from the Federal Statistical Office Germany from 2003 to 2006, Fach Series 12, Series 4, data set: Cause of death, breast cancer (PDF)
- ↑ a b rme / aerzteblatt.de: Breast cancer is different in men. In: aerzteblatt.de . December 15, 2014, accessed December 27, 2014 .
- ↑ https://www.krebshilfe.de/informieren/presse/neues-aus-der-forschung/brustkrebs-neue-therapie-mit-cholesterinsenkern/ accessed on October 10, 2019.
- ↑ Jael Backe: Breast cancer in men . In: Deutsches Ärzteblatt . tape 99 , no. 17 . Deutscher Ärzte-Verlag , April 26, 2002, p. A-1168 / B-970 / C-913 .
- ↑ Hui Miao, Helena M. Verkooijen, Kee-Seng Chia, Christine Bouchardy, Eero Pukkala, Siri Larønningen, Lene Mellemkjær, Kamila Czene, Mikael Hartma: Incidence and Outcome of Male Breast Cancer: An International Population-Based Study. In: Journal of Clinical Oncology . Volume 29, 2011, pp. 4381-4386, doi: 10.1200 / JCO.2011.36.8902 .
- ↑ Breast Cancer in Men | NEJM. Retrieved December 17, 2018 .
- ^ Brustkrebs-beim-mann.de website of the network.
- ↑ Breast cancer in men. (krebsinformationsdienst.de)
- ↑ Hereditary breast cancer .
- ^ A. Antoniou, PD Pharoah, S. Narod et al. a .: Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case series unselected for family history: a combined analysis of 22 studies. In: Am J Hum Genet. Volume 72, 2003, pp. 1117-1130. PMID 12677558 .
- ^ MR Stratton, N. Rahman: The emerging landscape of breast cancer susceptibility. In: Nature Genetics . Volume 40, No. 1, 2008, pp. 17-22. PMID 18163131 .
- ↑ R. Schmutzler, A. Meindl: Hereditary breast cancer: Genetics and prevention. In: Current recommendations for the treatment of primary and advanced breast cancer. (Ed. C. Thomssen for the Mamma Commission of the Gynecological Oncology Working Group). Zuckschwerdt-Verlag, 2007, ISBN 978-3-88603-916-6 .
- ↑ K. Hemminki, A. Försti, J. Lorenzo Bermejo: Surveying germline genomic landscape of breast cancer. In: Breast Cancer Res Treat . Volume 113, 2009, pp. 601-603. PMID 18297427 .
- ↑ Familial breast cancer. In: The Lancet . Volume 358, 2001, pp. 1389-1399, quoted from Uta Wagenmann: In search of the magic cancer gene. In: Friday. April 26, 2002 (freitag.de)
- ↑ Katharina Schmutzler, Markus Löffler, Jürgen Windeler, Stefanie Thomas, Johannes Bruns, Thomas Rath: Familial breast and ovarian cancer: From research to standard care . In: Deutsches Ärzteblatt . tape 102 , no. 50 . Deutscher Ärzte-Verlag , December 16, 2005, p. A-3486 / B-2948 / C-2461 ( aerzteblatt.de ).
- ↑ Internet, makeshift source : Hereditary breast and ovarian cancer - funding for genetic counseling secured throughout Austria for the next three years! (No longer available online.) Archived from the original on August 1, 2012 ; accessed on October 11, 2014 .
- ^ EV Jensen, HI Jacobson: Basic guides to the mechanism of estrogen action. In: Recent Progress in Hormone Research . tape 18 , 1962, pp. 387-414 .
- ↑ Early Breast Cancer Trialists' Collaborative Group: Tamoxifen for early breast cancer: An overview of the randomized trials. In: Lancet . tape 351 , 1998, pp. 1451-1467 .
- ↑ B. Fisher, JP Costantino, DL Wickerham et al: Tamoxifen for prevention of breast cancer: Report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. In: Journal of the National Cancer Institute . tape 90 , 1998, pp. 1371-1388 .
- ↑ Kala Visvanathan, Patricia Hurley, Elissa Bantug et al .: Use of Pharmacologic Interventions for Breast Cancer Risk Reduction: American Society of Clinical Oncology Clinical Practice Guideline. In: Journal of Clinical Oncology . tape 31 , 2013, p. 2942-2962 .
- ↑ Nicola Siegmund-Schultze, Vera Zylka-Menhorn, Renate Leinmüller, Rüdiger Meyer: Hormone therapy and breast cancer: A look at the current data situation . In: Deutsches Ärzteblatt . tape 105 , no. 6 . Deutscher Ärzte-Verlag , February 8, 2008, p. A-260 / B-234 / C-230 ( aerzteblatt.de ).
- ↑ JE Rossouw, GL Anderson, RL Prentice, AZ LaCroix, C. Kooperberg, ML Stefanick, RD Jackson, SA Beresford, BV Howard, KC Johnson, JM Kotchen, J. Ockene; Writing Group for the Women's Health Initiative Investigators .: Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women's Health Initiative randomized controlled trial. In: JAMA . tape 288 , no. 3 , 2002, p. 321-333 .
- ↑ J. Straszewski: Age at menarchy and breast cancer. In: Journal of the National Cancer Institute . tape 47 , 1971, p. 935 .
- ↑ D. Trichopoulos, B. MacMahon, P. Cole: Menopause and breast cancer risk. In: Journal of the National Cancer Institute . tape 48 , 1972, p. 605 .
- ↑ SN Dwivedi, P. Singh, N. Sareen, AS Bhadoria, U. Kapil: Reproductive factors and risk of breast cancer: A Review . In: Indian Journal of Cancer . tape 51 , no. 4 , October 1, 2014, ISSN 0019-509X , p. 571 , doi : 10.4103 / 0019-509X.175345 , PMID 26842199 ( indianjcancer.com [accessed December 21, 2018]).
- ↑ U. Ackermann-Liebrich: Breastfeeding as a prevention against breast cancer. ( Memento of October 24, 2007 in the Internet Archive ) infomed.org, November / December 2002. After a publication in The Lancet , 260/2002, pp. 187-195.
- ↑ V. Beral et al.: Breast cancer and abortion: collaborative reanalysis of data from 53 epidemiological studies, including 83,000 women with breast cancer from 16 countries. In: The Lancet. 363/2004, pp. 1007-1016. PMID 15051280 .
- ↑ DH Brewster et al .: Risk of breast cancer after miscarriage or induced abortion: a Scottish record linkage case-control study. In: J Epidemiol Community Health. 59/2005, pp. 283-287. PMID 15767381 .
- ↑ X. Paoletti, F. Clavel-Chapelon: Induced and spontaneous abortion and breast cancer risk: results from the E3N cohort study. In: Int J Cancer 106/2003, pp. 270-276. PMID 12800205 .
- ^ GK Reeves et al.: Breast cancer risk in relation to abortion: Results from the EPIC study. In: Int J Cancer. 119/2006, pp. 1741-1745. PMID 16646050 .
- ^ S. Rice, SA Whitehead: Phytoestrogens and breast cancer – promoters or protectors? In: Endocrine-related cancer. Volume 13, Number 4, December 2006, pp. 995-1015, doi: 10.1677 / erc.1.01159 . PMID 17158751 . (Review).
- ↑ Phytoestrogens and Breast Cancer. Cornell University, July 2001; Retrieved November 25, 2009.
- ↑ MK Ramadhani, SG Elias et al .: Innate left handedness and risk of breast cancer: case-cohort study. In: BMJ (Clinical research ed.). Volume 331, Number 7521, October 2005, pp. 882-883, doi: 10.1136 / bmj.38572.440359.AE . PMID 16186135 . PMC 1255796 (free full text).
- ↑ Breast cancer: increased risk in left-handed women. In: Spiegel Online . September 26, 2005, accessed December 27, 2014 .
- ↑ Harald Frater: scinexx - More breast cancer in left-handed women: relationship between handedness and cancer incidence uncovered - cancer, breast cancer, left-handed people - Kre. (No longer available online.) In: go.de. September 26, 2005, archived from the original ; accessed on December 27, 2014 .
- ↑ a b c L. Titus-Ernstoff, PA Newcomb et al .: Left-handedness in relation to breast cancer risk in postmenopausal women. In: Epidemiology (Cambridge, Mass.). Volume 11, Number 2, March 2000, pp. 181-184. PMID 11021617 .
- ↑ L. Fritschi et al.: Left-handedness and risk of breast cancer. In: Br J Cancer . 97, 2007, pp. 686-687. PMID 17687338 . PMC 2360366 (free full text)
- ↑ D. Trichopoulos: Hypothesis: does breast cancer originate in utero. In: The Lancet . 335, 1990, pp. 939-940. PMID 1970028 .
- ↑ N. Geschwind, AM Galaburda: Cerebral lateralization. Biological mechanisms, associations, and pathology: I. A hypothesis and a program for research. In: Archives of neurology. Volume 42, Number 5, May 1985, pp. 428-459. PMID 3994562 .
- ^ V. Llaurens u. a .: Why are some people left-handed? An evolutionary perspective. In: Phil Trans R Soc B. 364, 2009, pp. 881-894. doi: 10.1098 / rstb.2008.0235 PMID 19064347 (Review)
- ↑ a b c R. Roychoudhuri et al.: Cancer and laterality: a study of the five major paired organs (UK). In: Cancer Causes & Control 17, 2006, pp. 655-662. PMID 16633912 .
- ^ A. Ekbom et al.: Epidemiologic correlates of breast cancer laterality (Sweden). In: Cancer Causes & Control. 5, 1994, pp. 510-516. PMID 7827237 .
- ^ HA Weiss et al: Laterality of breast cancer in the United States. In: Cancer Causes & Control. 7, 1996, pp. 539-543. PMID 8877052 .
- ^ CI Perkins et al: Association between breast cancer laterality and tumor location, United States, 1994-1998. In: Cancer Causes Control. 15, 2004, pp. 637-645. PMID 15280621 .
- ↑ MT Goodman et al .: Comparative epidemiology of breast cancer among men and women in the US, 1996 to 2000. In: Cancer Causes Control. 17, 2006, pp. 127-136. PMID 16425090 .
- ^ S. Dane et al.: Asymmetries in breast cancer lateralization and both axillary lymph node number and metastatic involvement. In: Lymphology. 41, 2008, pp. 75-79. PMID 18720914 .
- ↑ a b O. Hallberg, O. Johansson: Sleep on the right side-Get cancer on the left? In: Pathophysiology. 17, 2010, pp. 157-160. PMID 19647986 .
- ^ MA Kramer, S. Albrecht, RA Miller: Handedness and the laterality of breast cancer in women. In: Nursing research. Volume 34, Number 6, Nov-Dec 1985, pp. 333-337. PMID 2866491 .
- ↑ Frequently asked questions. ( Memento of March 9, 2009 in the Internet Archive ) Retrieved November 27, 2009.
- ↑ E. Nekolla: Epidemiology of radiation-induced breast cancer. Dissertation, LMU Munich, 2004.
- ^ FA Mettler, AC Upton et al.: Benefits versus risks from mammography: a critical reassessment. In: Cancer. Volume 77, Number 5, March 1996, pp. 903-909. PMID 8608482 (Review).
- ↑ a b Women’s Health Initiative, Gyne online, June 4, 2007 quoted according to the breast cancer risk in overweight ( memento of February 11, 2009 in the Internet Archive )
- ^ P. Reynolds, S. Hurley et al .: Active smoking, household passive smoking, and breast cancer: evidence from the California Teachers Study. In: Journal of the National Cancer Institute. Volume 96, Number 1, January 2004, pp. 29-37. PMID 14709736 .
- ↑ C. Aceves, B. Anguiano, G. Delgado: Is iodine a gatekeeper of the integrity of the mammary gland? In: Journal of Mammary Gland Biology and Neoplasia . tape 10 , no. 2 , April 2005, p. 189-196 , doi : 10.1007 / s10911-005-5401-5 , PMID 16025225 .
- ↑ P. Zubor, A. Gondova, J. Polivka Jr, P. Kasajova, K. Konieczka, J. Danko, O. Golubnitschaja: Breast cancer and Flammer syndrome: any symptoms in common for prediction, prevention and personalized medical approach? In: EPMA Journal. Volume 8, No. 2, Apr 10, 2017, pp. 129-140.
- ↑ Lack of sun promotes cancer! ( Memento of September 30, 2007 in the Internet Archive ) (PDF; 2.0 MB). In: Medical Tribune. Volume 42, No. 23, June 8, 2007, p. 21.
- ↑ JM Lappe u. a .: Vitamin D and calcium supplementation reduces cancer risk: results of a randomized trial. In: The American journal of clinical nutrition. 85/2007, pp. 1586-1591. PMID 17556697 .
- ↑ AM Misotti, P. Gnagnarella: Vitamin supplement consumption and breast cancer risk: a review. In: Ecancermedicalscience. Volume 7, 2013, p. 365, doi: 10.3332 / ecancer.2013.365 . PMID 24171049 . PMC 3805144 (free full text). (Review).
- ^ AA Rose, C. Elser et al .: Blood levels of vitamin D and early stage breast cancer prognosis: a systematic review and meta-analysis. In: Breast cancer research and treatment. Volume 141, Number 3, October 2013, pp. 331-339, doi: 10.1007 / s10549-013-2713-9 . PMID 24104883 . (Review).
- ↑ F. Sperati, P. Vici et al.: Vitamin D supplementation and breast cancer prevention: a systematic review and meta-analysis of randomized clinical trials. In: PloS one. Volume 8, number 7, 2013, p. E69269, doi: 10.1371 / journal.pone.0069269 . PMID 23894438 . PMC 3718745 (free full text). (Review).
- ↑ M. Smollich, M. Götte et al .: On the role of endothelin-converting enzyme-1 (ECE-1) and neprilysin in human breast cancer. In: Breast cancer research and treatment. Volume 106, Number 3, December 2007, pp. 361-369, doi: 10.1007 / s10549-007-9516-9 . PMID 17295044 .
- ↑ MS Farvid, E. Cho et al .: Dietary protein sources in early adulthood and breast cancer incidence: prospective cohort study. In: BMJ (Clinical research ed.). Volume 348, 2014, pg3437. PMID 24916719 . PMC 4051890 (free full text).
- ↑ BM Lynch, HK Neilson, CM Friedenreich: Physical activity and breast cancer prevention. In: Recent results in cancer research. Volume 186, 2011, pp. 13-42, doi : 10.1007 / 978-3-642-04231-7_2 . PMID 21113759 . (Review).
- ↑ a b cancer.org: Detailed Guide: Breast Cancer - What Are the Risk Factors for Breast Cancer? ( Memento of the original from April 29, 2009 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. Retrieved May 6, 2008.
- ↑ M. Gago-Dominguez, JM Yuan, CL Sun, HP Lee, MC Yu: Opposing effects of dietary n-3 and n-6 fatty acids on mammary carcinogenesis: The Singapore Chinese Health Study. In: British Journal of Cancer . Volume 89, Number 9, November 2003, pp. 1686-1692, doi: 10.1038 / sj.bjc.6601340 . PMID 14583770 . PMC 2394424 (free full text).
- ↑ K. Wakai, K. Tamakoshi, C. Date, M. Fukui, S. Suzuki, Y. Lin, Y. Niwa, K. Nishio, H. Yatsuya, T. Kondo, S. Tokudome, A. Yamamoto, H. Toyoshima, A. Tamakoshi: Dietary intakes of fat and fatty acids and risk of breast cancer: a prospective study in Japan. In: Cancer Science . Volume 96, Number 9, September 2005, pp. 590-599, doi: 10.1111 / j.1349-7006.2005.00084.x . PMID 16128744 .
- ↑ JS Zheng, XJ Hu u. a .: Intake of fish and marine n-3 polyunsaturated fatty acids and risk of breast cancer: meta-analysis of data from 21 independent prospective cohort studies. In: BMJ (Clinical research ed.). Volume 346, 2013, p. F3706. PMID 23814120 . (Review).
- ↑ Anthony B. Miller, Claus Wall, Cornelia J. Baines, Ping Sun, Teresa To: Twenty five year follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study: randomized screening trial . In: BMJ (Clinical research ed.) . tape 348 , February 11, 2014, ISSN 1756-1833 , p. g366 , doi : 10.1136 / bmj.g366 , PMID 24519768 , PMC 3921437 (free full text).
- ↑ EJ Aiello, DS Buist et al .: Rate of breast cancer diagnoses among postmenopausal women with self-reported breast symptoms. In: The Journal of the American Board of Family Practice / American Board of Family Practice. Volume 17, Number 6, Nov-Dec 2004, pp. 408-415. PMID 15575032 .
- ^ DB Thomas, DL Gao et al .: Randomized trial of breast self-examination in Shanghai: final results. In: Journal of the National Cancer Institute. Volume 94, Number 19, October 2002, pp. 1445-1457. PMID 12359854 .
- ↑ JP Kösters, PC Gøtzsche: Regular self-examination or clinical examination for early detection of breast cancer. In: Cochrane Database Syst Rev. 2/2003, Art. CD003373. PMID 12804462 .
- ^ A b Agency for Healthcare Research and Quality: Screening for Breast Cancer. ( Memento of January 5, 2007 in the Internet Archive ) February 2002, accessed on November 27, 2009.
- ↑ Jolie Ringash and the Canadian Task Force on Preventive Health Care: Preventive health care, 2001 update: screening mammography among women aged 40-49 years at average risk of breast cancer. ( Memento of January 2, 2007 in the Internet Archive ). Retrieved December 27, 2009.
- ↑ Silicone model for breast self-examination. In: Constanze Schäfer, Ingo Donieth: Aids and medical products. Wissenschaftliche Verlagsgesellschaft , Stuttgart 2003, ISBN 3-8047-1948-1 .
- ↑ a b Patient brochure for the AWMF guideline (077/001) "Breast Cancer Early Detection" of the German Cancer Society and the German Cancer Aid Early Detection of Breast Cancer - A Decision -Making Guide for Women (PDF) accessed on November 12, 2018.
- ↑ MRI finds more tumors. In: curado.de. March 29, 2007, accessed December 27, 2014 .
- ^ Mammography Screening Program. ( Memento of September 4, 2011 in the Internet Archive ) January 20, 2011, accessed on January 10, 2012.
- ↑ S. Fabbri et al: Benign Breast Diseases in Breast Cancer Screening Programs in Italy 2000-2001. ( Memento from January 31, 2012 in the Internet Archive ) (PDF; 155 kB). In: Tumori. 90, 2004, pp. 547-549.
- ^ P. Taylor, HW Potts: Computer Aids and Human Second Reading as Interventions in Screening Mammography. In: Eur J Cancer . 44, 2008, pp. 798-807. PMID 18353630 .
- ↑ IGeL-Monitor, Assessment of MRI of the breast for early cancer detection and ultrasound of the breast for early cancer detection , accessed on October 19, 2018.
- ↑ University reports after blood test PR. In: Süddeutsche Zeitung. April 8, 2019. Retrieved April 14, 2019.
- ↑ Press release Heidelberg University Hospital , February 21, 2019. Accessed February 21, 2019.
- ↑ Jens-Uwe Blohmer, Annette Hasenburg, Wolfgang Janni: Joint statement on reporting on new blood test for early detection of breast cancer. (PDF) Arbeitsgemeinschaft Gynäkologische Onkologie eV, February 27, 2019, accessed on March 8, 2019 .
- ↑ J. Baltzer, H.-G. Meerpohl, J. Bahnsen: Practice of gynecological oncology - practice of gynecology. 2nd Edition. Volume 3, Georg Thieme Verlag, 2000, ISBN 3-13-109912-7 , p. 296. ( limited preview in the Google book search)
- ↑ Ultrasound agreement according to Section 135 (2) SGB V, as of 2003. ( Page no longer available , search in web archives ).
- ↑ a b c d e S3 guideline early detection, diagnosis, therapy and follow-up care for breast cancer in 2020. In: AWMF online
- ↑ Berthold Jany, Tobias Welte: Pleural effusion in adults - causes, diagnosis and therapy. In: Deutsches Ärzteblatt. Volume 116, No. 21, 2019, pp. 377-385, here: pp. 379 and 383.
- ↑ S. Lakhani, IO Ellis, SJ Schnitt, MJ van de Vijver: WHO Classification of Tumors of the Breast, Fourth Edition . International Agency for Research on Cancer, Lyon 2012, ISBN 978-92-832-2433-4 ( online ).
- ↑ S3 guideline for breast cancer of the Dt. Cancer Society ( Memento from January 18, 2012 in the Internet Archive ) (PDF; 1.67 MB) pp. 28–29, p. 185.
- ↑ AC Wolff, ME Hammond et al: American Society of Clinical Oncology / College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. In: Journal of Clinical Oncology. Volume 25, Number 1, Jan 2007, pp. 118-145. (ascopubs.org) . doi : 10.1043 / 1543-2165 (2007) 131 [18: ASOCCO] 2.0.CO; 2 . PMID 19548375 .
- ^ A. Goldhirsch, WC Wood et al. a .: Progress and promise: highlights of the international expert consensus on the primary therapy of early breast cancer 2007. In: Annals of Oncology . Volume 18, Number 7, July 2007, pp. 1133-1144, doi: 10.1093 / annonc / mdm271 . PMID 17675394 . (Review).
- ↑ LA Carey, CM Perou et al. a .: Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. In: JAMA. Volume 295, Number 21, June 2006, pp. 2492-2502, doi: 10.1001 / jama.295.21.2492 . PMID 16757721 .
- ↑ a b c d Nadine Eckert: Breast cancer: More certainty for therapy . In: Dtsch Arztebl . tape 116 , no. 29-30 , 2019, pp. A-1373 / B-1135 / C-1119 ( online ).
- ↑ JA Sparano, RJ Gray, DF Makower, KI Pritchard, KS Albain, DF Hayes, CE Geyer Jr, EC Dees, MP Goetz, JA Olson Jr, T. Lively, SS Badve, TJ Saphner, LI Wagner, TJ Whelan, MJ Ellis, S. Paik, WC Wood, PM Ravdin, MM Keane, HL Gomez-Moreno, PS Reddy, TF Goggins, IA Mayer, AM Brufsky, DL Toppmeyer, VG Kaklamani, JL Berenberg, J. Abrams, GW Sledge, Jr. : Adjuvant Chemotherapy Guided by a 21-Gene Expression Assay in Breast Cancer . In: N Engl J Med . tape 379 , no. 2 , June 12, 2018, p. 111-121 , doi : 10.1056 / NEJMoa1804710 , PMID 29860917 (English).
- ↑ F. Cardoso, LJ van't Veer, J. Bogaerts, L. Slaets, G. Viale, S. Delaloge, JY Pierga, E. Brain, S. Causeret, M. DeLorenzi, AM Glas, V. Golfinopoulos, T. Goulioti, S. Knox, E. Matos, B. Meulemans, PA Neijenhuis, U. Nitz, R. Passalacqua, P. Ravdin, IT Rubio, M. Saghatchian, TJ Smilde, C. Sotiriou, L. Stork, C. Straehle, G. Thomas, AM Thompson, JM van der Hoeven, P. Vuylsteke, R. Bernards, K. Tryfonidis, E. Rutgers, M. Piccart; MINDACT Investigators: 70-Gene Signature as an Aid to Treatment Decisions in Early-Stage Breast Cancer . In: N Engl J Med . tape 375 , no. 8 , August 25, 2016, p. 717-729 , doi : 10.1056 / NEJMoa1602253 , PMID 27557300 (English).
- ^ German Cancer Society: The German Cancer Society officially awards the first “Breast Center Certificate”. ( Memento from December 3, 2012 in the web archive archive.today ) July 21, 2003.
- ↑ a b c “Requirements for structured treatment programs for patients with breast cancer”, Appendix 3 to §§ 28b to 28g of the Risk Structure Adjustment Ordinance according to § 137f SGB Fifth Book (V).
- ↑ K. Travis: Bernard Fisher reflects on a half-century's worth of breast cancer research. In: Journal of the National Cancer Institute. Volume 97, Number 22, November 2005, pp. 1636-1637, doi: 10.1093 / jnci / dji419 . PMID 16288112 .
- ↑ a b c d e Wolfgang Janni, Bernd Gerber, Harald Sommer, Michael Untch, Annette Krause, Darius Dian, Ingo Runnebaum , Brigitte Rack, Klaus Friese: Certified medical training: Therapy of primary, invasive breast cancer . In: Deutsches Ärzteblatt . tape 102 , no. 41 . Deutscher Ärzte-Verlag , October 14, 2005, p. A-2795 / B-2360 / C-2226 .
- ↑ a b c V. Naraynsingh et al. a .: Immediate breast reconstruction following segmentectomy using a latissimus dorsi 'myoadipose' flap through a single axillary incision: a case series. In: Cases Journal. 2, 2009, 8116. PMID 19830050 ( Open Access , under CC-by-3.0 license).
- ↑ a b S. Reefy u. a .: Oncological outcome and patient satisfaction with skin-sparing mastectomy and immediate breast reconstruction: a prospective observational study. In: BMC Cancer. Volume 10, 2010, p. 171 doi: 10.1186 / 1471-2407-10-171 ( Open Access , under CC-by-2.0).
- ↑ WF Hartsell et al .: Should multicentric disease be an absolute contraindication to the use of breast-conserving therapy? In: Int J Radiat Oncol Biol Phys 30, 1994, pp. 49-53. PMID 8083128 .
- ^ O. Gentilini, E. Botteri et al: Conservative surgery in patients with multifocal / multicentric breast cancer. In: Breast cancer research and treatment. Volume 113, Number 3, February 2009, pp. 577-583, doi: 10.1007 / s10549-008-9959-7 . PMID 18330695 .
- ↑ T. Kühn et al. a .: Sentinel node biopsy in breast cancer. (PDF). In: obstetric women's health. Volume 63, 2003, pp. 835-840.
- ↑ Beatrice Cavallo Marincola, Luisa Di Mare, Federica Pediconi, Luca Bertaccini, Fabrizio Boni, Alessandro Napoli, Carlo Catalano: Clinical Experience in Noninvasive Treatment of Focal Breast Cancer with Magnetic Resonance Guided High Intensity Focused Ultrasound (MRgFUS) (PDF).
- ↑ a b E. H. Romond, EA Perez, J. Bryant include: Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. In: The New England Journal of Medicine . Volume 353, Number 16, October 2005, pp. 1673-1684, doi: 10.1056 / NEJMoa052122 . PMID 16236738 .
- ↑ a b E. A. Perez, EH Romond et al .: Updated results of the combined analysis of NCCTG N9831 and NSABP B-31 adjuvant chemotherapy with / without trastuzumab in patients with HER2-positive breast cancer. In: J Clin Oncol 2007 ASCO Annual Meeting Proceeding. 25 (Suppl 18S): 2007, 6s (abstract 512).
- ↑ a b M. J. Piccart-Gebhart, M. Procter et al .: Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. In: The New England Journal of Medicine . Volume 353, Number 16, October 2005, pp. 1659-1672, doi: 10.1056 / NEJMoa052306 . PMID 16236737 .
- ↑ L. Gianni, A. Goldhirsch et al: Update of the HERA trial and the role of 1 year trastuzumab as adjuvant therapy for breast cancer. In: The Breast . Volume 18, Suppl 1, 2009, p. S11 (abstract S25).
- ↑ Summary of Product Characteristics , EMA EPAR, accessed on October 29, 2019.
- ↑ SC Darby, M. Ewertz et al. a .: Risk of ischemic heart disease in women after radiotherapy for breast cancer. In: The New England Journal of Medicine . Volume 368, Number 11, March 2013, pp. 987-998, doi: 10.1056 / NEJMoa1209825 . PMID 23484825 .
- ^ Sören von Otte, Michael Friedrich , Klaus Diedrich, Markus Kupka: Preserving fertility in oncological patients: status and perspectives . In: Deutsches Ärzteblatt . tape 103 , no. 38 . Deutscher Ärzte-Verlag , September 22, 2006, p. A-2479 / B-2149 / C-2073 .
- ↑ Medicine - Communication: DGE: Hormone deficiency damages the brain. Working Group of Scientific Medical Societies, press release from 2007-11-06 at Informationsdienst Wissenschaft (idw-online.de), accessed on December 27, 2014.
- ^ G. von Minckwitz: For The Breast Commission of the German Gynaecological Oncology Working Group (AGO). Evidence-based treatment of metastatic breast cancer - 2006 recommendations by the AGO Breast Commission. In: Eur J Cancer. Volume 42, 2006, pp. 2897-2908. PMID 17046240 .
- ↑ dapi.de: 46% more breast cancer patients have been supplied with modern aromatase inhibitors since 2003. Association of the German Drug Testing Institute, from November 13, 2012.
- ↑ ema.europa.eu: Faslodex. (PDF; 46 kB) European Medicines Agency, March 2010.
- ↑ DF Hayes: Tamoxifen: Dr. Jekyll and Mr. Hyde? In: Journal of the National Cancer Institute. Volume 96, Number 12, June 2004, pp. 895-897. PMID 15199102 .
- ↑ CK Osborne, V. Bardou, TA Hopp, GC Chamness, SG Hilsenbeck, SA Fuqua, J. Wong, DC Allred, GM Clark, R. Schiff: Role of the estrogen receptor coactivator AIB1 (SRC-3) and HER-2 / new in tamoxifen resistance in breast cancer. In: Journal of the National Cancer Institute. Volume 95, Number 5, March 2003, pp. 353-361. PMID 12618500 .
- ↑ A. Gucalp, S. Tolaney et al .: Phase II trial of bicalutamide in patients with androgen receptor-positive, estrogen receptor-negative metastatic breast cancer. In: Clinical cancer research. Volume 19, Number 19, October 2013, pp. 5505-5512, doi: 10.1158 / 1078-0432.CCR-12-3327 . PMID 23965901 . PMC 4086643 (free full text).
- ^ DR Cochrane, S. Bernales, BM Jacobsen, DM Cittelly, EN Howe, NC d Amato, NS Spoelstra, SM Edgerton, A. Jean, J. Guerrero, F. Gómez, S. Medicherla, IE Alfaro, E. McCullagh, P. Jedlicka, KC Torkko, AD Thor, AD Elias, AA Protter, JK Richer: Role of the Androgen Receptor in Breast Cancer and Preclinical Analysis of Enzalutamide. In: Breast Cancer Research. Volume 16, No. 1, 2014, p. R7. doi: 10.1186 / bcr3599 . PMC 3978822 (free full text). PMID 24451109 .
- ↑ Data From Omnitarg Clinical Program Presented at the American Society of Clinical Oncology Meeting. Genentech, accessed June 28, 2014 .
- ↑ D. Slamon , W. Eiermann, N. Robert a. a .: BCIRG 006: 2nd interim analysis phase III randomized trial comparing doxorubicin and cyclophosphamide followed by docetaxel (ACT) with doxorubicin and cyclophophamide followed by docetaxel and trastuzumab (ACTH) with docetraxel, carboplatin and trastuzumab (TCH) in HER2neu positive early breast cancer patients. In: Breast Cancer Res Treat. Volume 100, Suppl 1, 2006, abstr 52.
- ↑ D. Slamon, W. Eiermann, N. Robert et al .: Presentation at the 29th SABCS. San Antonio, Texas, USA, December 14-17, 2006.
- ↑ B. Krempien: The development of bone pain in bone metastases and their treatment by bisphophonates. In: HH Bartsch, W. Hornstein (Ed.): Interdisciplinary pain therapy for tumor patients. Karger Publishers, 1998, ISBN 3-8055-6594-1 . ( limited preview in Google Book search)
- ↑ NJ Robert V. Dieras include: RIBBON-1: randomized, double-blind, placebo-controlled, phase III trial of chemotherapy with or without bevacizumab for first-line treatment of human epidermal growth factor receptor 2-negative, locally recurrent or metastatic breast cancer. In: Journal of clinical oncology. Volume 29, number 10, April 2011, pp. 1252-1260, doi: 10.1200 / JCO.2010.28.0982 . PMID 21383283 .
- ↑ J. Cortes, J. O'Shaughnessy et al. a .: Eribulin monotherapy versus treatment of physician's choice in patients with metastatic breast cancer (EMBRACE): a phase 3 open-label randomized study. In: Lancet. Volume 377, number 9769, March 2011, pp. 914-923, doi: 10.1016 / S0140-6736 (11) 60070-6 . PMID 21376385 .
- ↑ Freerk T. Baumann, Klaus Schüle (Ed.): Movement therapy and sport in cancer: guidelines for practice . 1st edition. Deutscher Ärzte-Verlag, 2008, ISBN 978-3-7691-0564-3 , p. 274 .
- ↑ Sameh M. Arab: Medicine in Ancient Egypt 2. In: arabworldbooks.com. Retrieved December 27, 2014 .
- ↑ a b c A History of Breast Cancer. ( Memento of July 30, 2010 in the Internet Archive ).
- ↑ a b c d e f Orlando E. Silva, Stefano Zurrida: Breast cancer: diagnosis and therapy . Elsevier, Urban & Fischer Verlag, 2007, ISBN 978-3-437-24260-1 ( full text in the Google book search).
- ^ The History of Cancer. (No longer available online.) In: American Cancer Society. March 9, 2009, archived from the original on October 9, 2006 ; Retrieved March 26, 2010 .
- ↑ Corpus Hippocraticum : Epidemics 5,101.
- ^ Corpus Hippocraticum : Aphorisms 6.38.
- ↑ a b c d Hermann Delbrück: Breast cancer: advice and help for those affected and their families . W. Kohlhammer Verlag, 2008, ISBN 3-17-020469-6 ( full text in the Google book search).
- ↑ a b c d Manfred Kaufmann , Ismail Jatoi, Jean Petit: Atlas of breast surgery . Springer Verlag, 2007, ISBN 3-540-48881-2 ( full text in the Google book search).
- ↑ Benjamin Bell: teaching concept of Wundarzney art . 3. Edition. tape 6 . Weidmann, 1809 ( full text in the Google book search).
- ^ William Stewart Halsted : The results of operations for the cure of cancer of the breast performed at the Johns Hopkins Hospital from June, 1889 to January, 1894. In: Ann Surg . Volume 20, 1894, p. 497.
- ↑ Josef Rotter : Favorable long-term success through an improved surgical procedure for breast cancer. In: Berl. clin. Wschr. Volume 33, 1896, p. 69.
- ↑ J. Hirsch: Radiosurgery of breast cancer. In: Dtsch Med Wochenschr. Volume 34, 1927, pp. 1419-1421.
- ^ DH Patey, WH Dyson: The prognosis of carcinoma of the breast in relation to the type of operation performed. In: British Journal of Cancer . Volume 2, Number 1, March 1948, pp. 7-13. PMID 18863724 . PMC 2007539 (free full text).
- ↑ R. McWhriter: Simple mastectomy and radiotherapy in the treatment of breast cancer. In: The British journal of radiology. Volume 28, Number 327, March 1955, pp. 128-139. PMID 14351717 .
- ↑ B. Fisher, ER Fisher: Transmigration of lymph nodes by tumor cells. In: Science. Volume 152, Number 3727, June 1966, pp. 1397-1398. PMID 5949244 .
- ↑ Renate Leinmüller: Breast Cancer: Primary chemotherapy as a prognostic marker . In: Deutsches Ärzteblatt . tape 95 , no. 44 . Deutscher Ärzte-Verlag , October 30, 1998, p. A-2753 / B-2344 / C-2082 .
- ↑ Y. Miki, J. Swensen et al: A strong candidate for the breast and ovarian cancer susceptibility gene BRCA1. In: Science. Volume 266, Number 5182, October 1994, pp. 66-71. PMID 7545954 .
- ^ R. Wooster, SL Neuhausen et al .: Localization of a breast cancer susceptibility gene, BRCA2, to chromosome 13q12-13. In: Science. Volume 265, Number 5181, September 1994, pp. 2088-2090. PMID 8091231 .
- ↑ Terea Wagner among others: Hereditary breast and ovarian cancer. In: Detlev Ganten, Klaus Ruckpaul: Molecular medical principles of hereditary tumor diseases. Birkhäuser, 2001, ISBN 3-540-67808-5 , p. 257 full text in the Google book search
- ↑ JJ Gray, J. Estapé, M. Diaz-Padron: Breast cancer in Rubens paintings. In: Breast cancer research and treatment. Volume 68, Number 1, July 2001, pp. 89-93. PMID 11678312 .
- ↑ CH Espinel: The portrait of breast cancer and Raphael's La Fornarina. In: Lancet. Volume 360, Number 9350, April 21-28 Dec 2002, pp. 2061-2063, doi: 10.1016 / S0140-6736 (02) 11997-0 . PMID 12504417 .
- ^ PA Braithwaite, D. Shugg: Rembrandt's Bathsheba: the dark shadow of the left breast. In: Annals of the Royal College of Surgeons of England. Volume 65, Number 5, September 1983, pp. 337-338. PMID 6351705 . PMC 2494383 (free full text).
- ↑ James Stuart Olson: Bathsheba's Breast . JHU Press, 2005, ISBN 0-8018-8064-5 ( full text in the Google book search).
- ^ A. Gross: An epidemic of breast cancer among models of famous artists. In: Breast cancer research and treatment. Volume 84, number 3, April 2004, p. 293, doi: 10.1023 / B: BREA.0000019965.21257.49 . PMID 15026627 .