BRCA1
| BRCA1 | ||
|---|---|---|

|
||
| after 1jm7 | ||
| other names |
RING finger protein 53 |
|
|
Existing structure data: 1JM7 , 1JNX , 1N5O , 1OQA , 1T15 , 1T29 , 1T2U , 1T2V , 1Y98 , 2ING , 3COJ , 3K0H , 3K0K , 3K15 , 3K16 , 3PXA , 3PXB , 3PXC , 3PXD , 3PXE , 4IFI , 4IGK , 4JLU , 4OFB , 4U4A , 4Y18 , 4Y2G |
||
| Mass / length primary structure | 7 to 210 kilodaltons / 63 to 1884 amino acids (depending on isoform) | |
| Isoforms | 8th | |
| Identifier | ||
| Gene name (s) | BRCA1 RNF53 | |
| External IDs | ||
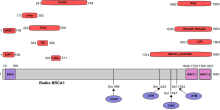
BRCA1 ( BR east CA ncer 1 , early-onset ), also referred to as breast cancer gene 1 in some publications , is a human gene or its gene product , i.e. a protein . It is a tumor suppressor gene , which means that the function of the gene contributes to the suppression of tumors.
Function of BRCA1
BRCA1 plays an important role in the repair of double strand breaks. A loss-of-function mutation or deletion of the BRCA1 gene increases the likelihood of tumor formation, especially for breast cancer, ovarian cancer , colon cancer, and prostate cancer . The protein encoded by BRCA1 consists of 1863 amino acids and has a molar mass of 207,732 Daltons . It interacts in the cell nucleus of many normal body cell types with the protein encoded by BRCA3 ( RAD51C ) and the protein encoded by BRCA2 . All three proteins work together to repair breaks in damaged DNA. These interruptions can be caused, for example, by ionizing radiation . But these interruptions can also occur naturally during cell division. The functions and interactions of the three DNA repair proteins are the subject of intensive research and have not yet been fully clarified or understood.
The location of BRCA1 in the genome
In humans, the BRCA1 gene is located on the long arm (q arm) of chromosome 17 gene locus q21.31 between base pairs 41,196,311-41,277,500. At the moment 31 different transcripts ( isoforms ) are known.
Effects of BRCA1 mutations
It is assumed that around 5 to 10 percent of all breast cancers are inherited as an autosomal dominant one . BRCA1 is by far the most important causative gene. Women with an inherited, i.e. germline mutation in BRCA1 or BRCA2 fall ill on average around 20 years earlier than women without a familial-hereditary risk. The risk of developing breast cancer for a woman with a BRCA1 or BRCA2 mutation is around 50 to 80 percent. If a mutation carrier has already developed breast cancer in one breast, the probability that cancer will later develop in the other breast is around 60 percent. In addition, BRCA1 mutations also represent a risk factor for the development of ovarian , colon , pancreatic and prostate cancer . The lifelong risk of BRCA1 or BRCA2 mutation carriers of developing ovarian cancer is estimated at around 10 to 40 percent.
Mutations in the genes RAD51C (BRCA3) and RAD51D (both on the long arm of chromosome 17 ) , which were identified only a few years ago, also seem to convey a similarly high risk of breast cancer.
The American National Cancer Institute (NCI) emphasizes that most of the research into the effects of the BRCA1 and BRCA2 genes has been carried out on families with a high incidence of these cancers. Since family members share other genes and are often subjected to the same environmental influences, the risk assessments of these studies may not adequately reflect the risk of cancer due to BRCA gene mutation in the general population. In addition, there are no figures from the general population comparing the cancer risk of carriers of a BRCA1 or BRCA2 mutation with that of women without this mutation.
BRCA1 genetic test
There is a genetic test that can be used to determine whether a patient has a mutated form of the BRCA1 gene. The cost of the test in 2004 was around 2500 euros. The combined BRCA1-BRCA2 test now costs less than 1500 euros in Europe.
For women with a family history of breast and ovarian cancer, the statutory health insurance companies cover the costs for advice, genetic testing and the early detection program. Performing the test is considered useful if one of the following criteria applies:
- at least two women in the family have or have had breast cancer, at least one of them before the age of 51
- three women with breast cancer in the family (regardless of age)
- a family disease with unilateral breast cancer and an age of onset before the age of 31
- a family history of bilateral breast cancer with the first disease occurring at age 41 or earlier
- a family history of ovarian cancer if the disease started before the age of 41
- a family case with breast and ovarian cancer
- two or more cases of ovarian cancer in the family.
Before and after performing the genetic test, it is very important to have intensive discussions with the patient.
In 2008 at the University College Hospital in London, the fertilized embryos of a woman after in vitro fertilization were examined for the BRCA1 gene using pre-implantation diagnosis (PGD) for the first time. Six of the eleven embryos created in the “test tube” carried the mutated BRCA1 gene during the PGD carried out three days after fertilization and were destroyed. Two of the remaining embryos were transplanted into the uterus . One of the embryos successfully implanted. The mother gave birth to a girl in early January 2009. The process led to controversial discussions as this form of genetic selection of babies is extremely controversial.
Prevention
Patients with a genetic predisposition to BRCA1 currently have several primary and secondary preventive measures.
Primary prevention
Primary prevention , also known as prophylaxis, refers to measures to promote health or to keep the patient healthy.
Chemoprevention
In several studies, the adjuvant therapy with tamoxifen , compared to the placebo , was examined with regard to the primary prevention of breast cancer. Tamoxifen is a selective estrogen receptor modulator that is used as a drug for the treatment of breast cancer. The active ingredient has also been approved by the American FDA for the prevention of breast cancer in women at increased risk.
Four years after the start of the so-called NASABP P-1 study, tamoxifen reduced the risk of estrogen receptor-positive forms of breast cancer by 49 percent. However, this risk reduction could not be proven in the two subsequent studies.
Preventive removal of the ovaries and fallopian tubes
Several studies have shown that bilateral preventive removal of the ovaries and fallopian tubes (a salpingo-ovariectomy ) reduces the risk of cancer in carriers of a BRCA1 mutation. Both fallopian tubes and ovaries should always be removed, as the fallopian tubes are also at risk of cancer.
The overall survival rate over 30 years is increased by 15% (absolute) with a salpingo-oovariectomy at the age of 40 years. An earlier salpingo-ovariectomy does not increase the survival rate and leads to increased undesirable side effects, especially menopausal symptoms and osteoporosis. With BRCA2 mutations, ovariectomy brings at best a marginal improvement in overall survival.
Preventive removal of the breasts
Preventive amputation of the breasts (prophylactic mastectomy) has become largely unnecessary due to advances in screening and treatment of breast cancer. While the breast cancer risk is largely eliminated, the resulting survival benefit is marginal at best.
Several randomized studies have shown that the breast cancer risk in mutation carriers of BRCA1 and BRCA2 can be reduced by more than 90 percent through preventive bilateral breast removal (bilateral prophylactic mastectomy).
Secondary prevention
The goal of secondary prevention is to reduce mortality through screening tests.
Mammography
Series mammography examinations from the age of 50 can reduce mortality by up to 30 percent. The main reason for this success lies in the early detection of small, lymph node- negative and highly differentiated carcinomas. Breast cancers based on BRCA1 and BRCA2 are only slightly differentiated ( degree of differentiation G3). In addition, the majority of the women at risk are younger than the average breast cancer patients. This gives them a denser glandular tissue that is difficult to assess mammographically.
Another potential problem with mammography in BRCA1 and BRCA2 high-risk patients is the ionizing X-rays of the examination method, which may cause DNA damage in the patients' cells. The mutations of the BRCA1 and BRCA2 genes with the corresponding proteins may not be able to adequately repair this damage (see BRCA1 and ionizing radiation ).
Sonography
Ultrasound examinations of the breast are significantly more sensitive than mammograms in young women with an increased familial breast cancer risk. However, too little data from studies are available for a final assessment.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) is currently the method with the highest sensitivity for diagnosing genetically caused breast cancer. The specificity, on the other hand, is less high, so that false positive results are sometimes obtained and the correct evaluation requires a high level of experience on the part of the radiologist. It should be the diagnostic method of choice for young women with a genetically proven increased risk of breast cancer.
BRCA1 and ionizing radiation
Ionizing radiation , such as X-rays , can damage DNA. This damage to DNA can cause tumors. Since the cells of the body have a DNA repair system, in most cases the damage caused by the ionizing radiation can be repaired. However, carriers of mutations in the BRCA1 or BRCA2 genes have a reduced ability to repair DNA in their body cells.
A retrospective study at the International Agency for Research on Cancer in Lyon investigated whether chest x- rays might increase the risk of breast cancer. After a single chest x-ray, BRCA1 / 2 carriers were 54 percent more likely to develop breast cancer. The risk increased significantly in women under 40 years of age, and women who had an examination before the age of 20 were more than four times more likely to get the disease than women who had never had a chest x-ray.
However, this first study does not allow a conclusive assessment of the risks of x-ray examinations or especially mammograms in high-risk patients. Retrospective studies are often falsified by the so-called recall bias . For example, women who have breast cancer may have remembered previous x-rays more often. In addition, the study lacks data on the dose in the X-ray examination. Causal associations can be made much more clearly via the dose-response relationship.
A study on the increase in breast cancer risk from mammography in women with BRCA1 or BRCA2 gene mutations concludes that there is apparently no connection between mammography and a significant increase in cancer in this group of people.
The discovery of BRCA1
In 1990, a group of researchers led by the American JM Hall discovered the gene, later named BRCA1, through linkage analyzes in Mormon families on chromosome 17. The discovery of the breast cancer gene was revolutionary and highly controversial at the time. A genetic predisposition as a cause of cancer spoke against the doctrine of the time. In 1994, Miki cloned BRCA1 as the first breast cancer gene .
In 1994 a second breast cancer gene was mapped and positionally cloned with BRCA2 on chromosome 13 gene locus q12-13.
To date, more than 75 different mutations of BRCA1 have been described in more than 100 families.
BRCA1 patents
In January 2001 the European Patent Office in Munich granted the US biotech company Myriad Genetics a patent (EP 699 754) on BRCA1. This led to significant international protests. In 2004 the European Patent Office revoked Myriad's rights. The reason for the revocation was an error in the gene sequence described by Myriad in the patent. In November 2004, Myriad ceded the US patent rights to the University of Utah . A new application was then submitted to the European Patent Office, which was finally granted in December 2008. The University of Utah can now charge license fees for every BRCA1 and BRCA2 test on the market. It is not yet known whether it will continue to do so in the future. While the combined BRCA1 / 2 test costs a maximum of 1500 euros in Europe, the BRCA1 test in the USA is more than twice as expensive due to license fees. However, smaller European countries were not included in the list of countries in the University of Utah's European patent application. This means that the test in countries such as Belgium will also be possible in the future without license fees.
See also
further reading
- SV Hodgson, PJ Morrison, M. Irving: Breast cancer genetics: unsolved questions and open perspectives in an expanding clinical practice. In: American journal of medical genetics. Part C, Seminars in medical genetics Volume 129C, Number 1, August 2004, pp. 56-64, doi: 10.1002 / ajmg.c.30019 . PMID 15264273 . (Review).
- AR Venkitaraman: Cancer susceptibility and the functions of BRCA1 and BRCA2. In: Cell Volume 108, Number 2, January 2002, pp. 171-182, PMID 11832208 . (Review).
- SN Powell, LA Kachnic: Roles of BRCA1 and BRCA2 in homologous recombination, DNA replication fidelity and the cellular response to ionizing radiation. In: Oncogene Volume 22, Number 37, September 2003, pp. 5784-5791, doi: 10.1038 / sj.onc.1206678 . PMID 12947386 . (Review).
- A. Antoniou, PD Pharoah, S. Narod, HA Risch, JE Eyfjord, JL Hopper, N. Loman, H. Olsson, O. Johannsson, A. Borg, B. Pasini, P. Radice, S. Manoukian, DM Eccles , N. Tang, E. Olah, H. Anton-Culver, E. Warner, J. Lubinski, J. Gronwald, B. Gorski, H. Tulinius, S. Thorlacius, H. Eerola, H. Nevanlinna, K. Syrjäkoski , OP Kallioniemi, D. Thompson, C. Evans, J. Peto, F. Lalloo, DG Evans, DF Easton: Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case series unselected for family history: a combined analysis of 22 studies. In: American Journal of Human Genetics Volume 72, Number 5, May 2003, pp. 1117-1130, doi: 10.1086 / 375033 . PMID 12677558 . PMC 118026 (free full text).
- Genetic testing and prophylactic surgery in the case of familial accumulation of the BRCA1 or BRCA2 mutation . In: Der Gynäkologe 33, 2000.
- Statement on the discovery of the breast cancer gene BRCA1. , Commission for Public Relations and Ethical Issues of the Society for Human Genetics e. V. , 7th edition October 2001. (PDF; 18 kB)
Web links
- Matthews / reactome: Phosphorylation of BRCA1 at multiple sites by ATM
- Penelope Farmer : Life within Fiction. Blog about the fight with BRCA1 cancer; from May 8, 2015.
Individual evidence
- ^ SJ Boulton: Cellular functions of the BRCA tumor-suppressor proteins. In: Biochemical Society Transactions Volume 34, November 2006, pp. 633-645, doi: 10.1042 / BST0340633 . PMID 17052168 . (Review).
- ↑ genome.ucsc.edu: Human chr17: 41,196,312-41,277,500 - UCSC Genome Browser v307
- ↑ ensemble.org: Ensemble Browser release 54
- ↑ JM Hall, MK Lee, B. Newman, JE Morrow, LA Anderson, B. Huey, MC King: Linkage of early-onset familial breast cancer to chromosome 17q21. In: Science Volume 250, Number 4988, December 1990, pp. 1684-1689, PMID 2270482 .
- ↑ mit.edu: MARY-CLAIRE KING - Genetic breast cancer detection. Retrieved November 22, 2007
- ↑ K. Hemminki, X. Li, K. Czene: Familial risk of cancer: data for clinical counseling and cancer genetics. In: International journal of cancer Volume 108, Number 1, January 2004, pp. 109-114, doi: 10.1002 / ijc.11478 . PMID 14618624 .
- ↑ a b c d Interdisciplinary S3 guideline for the diagnosis, therapy and follow-up care of breast cancer. Long version 3.0, update 2012. (PDF; 4.7 MB) (No longer available online.) DKG / Deutsche Krebshilfe | AWMF, archived from the original on May 12, 2013 ; Retrieved on May 14, 2013 (page 42 ff, section 3.3 .: Women at an increased risk of breast cancer, 3.3.1. Familial breast cancer). Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice.
- ^ National Cancer Institute: BRCA1 and BRCA2: Cancer Risk and Genetic Testing
- ↑ a b C. Berndt: Breast cancer genetic test released - patent office revokes rights of a US company to the cancer gene BRCA1. In: Süddeutsche Zeitung edition of May 19, 2004, Wissen, p. 12.
- ↑ a b Patent protection for the cancer gene BRCA1. ( Memento of the original from December 7, 2008 in the Internet Archive ) Info: The archive link was automatically inserted and not yet checked. Please check the original and archive link according to the instructions and then remove this notice. In: Aerzteblatt.de of December 3, 2008
- ↑ K. Ullrich: BRCA1 / 2 testing: criteria were modified. In: Medical Tribune . No. 2, April 2008, p. 7.
- ^ H. Keßler: Breast cancer: early detection by genetic test - redemption or stroke of fate: how a genetic test changes the life of women . In: Die Zeit , No. 12/1996
- ↑ Beckmann MW, High-Risk Families with Breast and Ovarian Cancer: Options for Counseling, Genetic Analysis and Early Detection. , In Deutsches Ärzteblatt , 94, 1997, pp. A161-A167
- ↑ unknown: First baby born in London without a breast cancer gene. In: Sächsische Zeitung , January 10, 2009
- ↑ First baby without breast cancer gene expected in London. In: Neue Zürcher Zeitung , December 20, 2008
- ↑ a b c H. Eggemann: Hereditary breast cancer - how many women are at risk and what is recommended for prophylaxis / therapy? In: Journal Onkologie , Edition 08/2005, Zeitschrift Online
- ↑ Fisher B et al., Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study . In: J Natl Cancer Inst , 90/1998, pp. 1371-88.
- ↑ T. Powles, R. Eeles, S. Ashley, D. Easton, J. Chang, M. Dowsett, A. Tidy, J. Viggers, J. Davey: Interim analysis of the incidence of breast cancer in the Royal Marsden Hospital tamoxifen randomized chemoprevention trial. In: The Lancet Volume 352, Number 9122, July 1998, pp. 98-101, doi: 10.1016 / S0140-6736 (98) 85012-5 . PMID 9672274 .
- ↑ U. Veronesi, P. Maisonneuve, A. Costa, V. Sacchini, C. Maltoni, C. Robertson, N. Rotmensz, P. Boyle: Prevention of breast cancer with tamoxifen: preliminary findings from the Italian randomized trial among hysterectomized women . Italian Tamoxifen Prevention Study. In: Lancet Volume 352, Number 9122, July 1998, pp. 93-97, PMID 9672273 .
- ^ TR Rebbeck, AM Levin, A. Eisen, C. Snyder, P. Watson, L. Cannon-Albright, C. Isaacs, O. Olopade, JE Garber, AK Godwin, MB Daly, SA Narod, SL Neuhausen, HT Lynch , BL Weber: Breast cancer risk after bilateral prophylactic oophorectomy in BRCA1 mutation carriers. In: Journal of the National Cancer Institute Volume 91, Number 17, September 1999, pp. 1475-1479, PMID 10469748 .
- ↑ a b A. W. Kurian, BM Sigal, SK Plevritis: Survival analysis of cancer risk reduction strategies for BRCA1 / 2 mutation carriers. In: Journal of clinical oncology Volume 28, Number 2, January 2010, pp. 222-231, doi: 10.1200 / JCO.2009.22.7991 . PMID 19996031 . PMC 2815712 (free full text).
- ↑ H. Meijers-Heijboer, B. van Geel, WL van Putten, SC Henzen-Logmans, C. Seynaeve, MB Menke-Pluymers, CC Bartels, LC Verhoog, AM van den Ouweland, MF Niermeijer, CT Brekelmans, JG Klijn: Breast cancer after prophylactic bilateral mastectomy in women with a BRCA1 or BRCA2 mutation. In: The New England Journal of Medicine Volume 345, Number 3, July 2001, pp. 159-164, doi: 10.1056 / NEJM200107193450301 . PMID 11463009 .
- ^ TR Rebbeck, T. Friebel, HT Lynch, SL Neuhausen, L. van 't Veer, JE Garber, GR Evans, SA Narod, C. Isaacs, E. Matloff, MB Daly, OI Olopade, BL Weber: Bilateral prophylactic mastectomy reduces breast cancer risk in BRCA1 and BRCA2 mutation carriers: the PROSE Study Group. In: Journal of clinical oncology Volume 22, Number 6, March 2004, pp. 1055-1062, doi: 10.1200 / JCO.2004.04.188 . PMID 14981104 .
- ↑ LC Hartmann, DJ Schaid, JE Woods, TP Crotty, JL Myers, PG Arnold, PM Petty, TA Sellers, JL Johnson, SK McDonnell, MH Frost, RB Jenkins: Efficacy of bilateral prophylactic mastectomy in women with a family history of breast cancer. In: The New England journal of medicine Volume 340, Number 2, January 1999, pp. 77-84, doi: 10.1056 / NEJM199901143400201 . PMID 9887158 .
- ↑ LC Hartmann, TA Sellers, DJ Schaid, TS Frank, CL Soderberg, DL Sitta, MH Frost, CS Grant, JH Donohue, JE Woods, SK McDonnell, CW Vockley, A. Deffenbaugh, FJ Couch, RB Jenkins: Efficacy of bilateral prophylactic mastectomy in BRCA1 and BRCA2 gene mutation carriers. In: Journal of the National Cancer Institute Volume 93, Number 21, November 2001, pp. 1633-1637, PMID 11698567 .
- ↑ G. Pichert, B. Bolliger, K. Buser, O. Pagani: Evidence-based management options for women at increased breast / ovarian cancer risk. In: Annals of Oncology Volume 14, Number 1, January 2003, pp. 9-19, PMID 12488287 . (Review).
- ^ I. Schreer: Breast cancer state of knowledge for early detection. In: Forum DKG 13, 1998, pp. 546-550.
- ↑ Pathology of familial breast cancer: differences between breast cancers in carriers of BRCA1 or BRCA2 mutations and sporadic cases. Breast Cancer Linkage Consortium. In: Lancet Volume 349, Number 9064, May 1997, pp. 1505-1510, PMID 9167459 .
- ↑ E. Warner, DB Plewes, RS Shumak, GC Catzavelos, LS Di Prospero, MJ Yaffe, V. Goel, E. Ramsay, PL chart, DE Cole, GA Taylor, M. Cutrara, TH Samuels, JP Murphy, JM Murphy , SA Narod: Comparison of breast magnetic resonance imaging, mammography, and ultrasound for surveillance of women at high risk for hereditary breast cancer. In: Journal of clinical oncology: official journal of the American Society of Clinical Oncology Volume 19, Number 15, August 2001, pp. 3524-3531, PMID 11481359 .
- ↑ a b Chest X-ray increases breast cancer risk in BRCA-1/2 gene carriers. In: Ärzteblatt study dated June 27, 2006 ( Memento of the original dated September 3, 2007 in the Internet Archive ) Info: The archive link was automatically inserted and not yet checked. Please check the original and archive link according to the instructions and then remove this notice.
- ↑ D. Goldfrank, S. Chuai, JL Bernstein, T. Ramon Y Cajal, JB Lee, MC Alonso, O. Diez, M. Baiget, ND Kauff, K. Offit, M. Robson: Effect of mammography on breast cancer risk in women with mutations in BRCA1 or BRCA2. In: Cancer Epidemiology, Biomarkers & Prevention Volume 15, Number 11, November 2006, pp. 2311-2313, doi: 10.1158 / 1055-9965.EPI-06-0176 . PMID 17119064 .
- ↑ JM Hall, MK Lee, B. Newman, JE Morrow, LA Anderson, B. Huey, MC King: Linkage of early-onset familial breast cancer to chromosome 17q21. In: Science Volume 250, number 4988, December 1990, pp 1684-1689, PMID 2270482 , see also H. Pidde: Physical Mapping and Genomic Structure of the Cariopherin Alpha 2 Gene. Dissertation, FU Berlin, 2000.
- ↑ Y. Miki, J. Swensen, D. Shattuck-Eidens, PA Futreal, K. Harshman, S. Tavtigian, Q. Liu, C. Cochran, LM Bennett, W. Ding: A strong candidate for the breast and ovarian cancer susceptibility gene BRCA1. In: Science Volume 266, Number 5182, October 1994, pp. 66-71, PMID 7545954 .
- ^ R. Wooster, SL Neuhausen, J. Mangion, Y. Quirk, D. Ford, N. Collins, K. Nguyen, S. Seal, T. Tran, D. Averill: Localization of a breast cancer susceptibility gene, BRCA2, to chromosome 13q12-13. In: Science Volume 265, Number 5181, September 1994, pp. 2088-2090, PMID 8091231 .
- ^ CI Szabo, MC King: Inherited breast and ovarian cancer. In: Human molecular genetics Volume 4 Spec No, 1995, pp. 1811-1817, PMID 8541881 . (Review).
- ↑ J. Feunteun, GM Lenoir: BRCA1, a gene Involved in inherited predisposition to breast and ovarian cancer. In: Biochimica et biophysica acta Volume 1242, Number 3, March 1996, pp. 177-180, PMID 8603070 . (Review).
- ^ SL Neuhausen, S. Mazoyer, L. Friedman, M. Stratton, K. Offit, A. Caligo, G. Tomlinson, L. Cannon-Albright, T. Bishop, D. Kelsell, E. Solomon, B. Weber, F. Couch, J. Struewing, P. Tonin, F. Durocher, S. Narod, MH Skolnick, G. Lenoir, O. Serova, B. Ponder, D. Stoppa-Lyonnet, D. Easton, MC King, DE Goldgar : Haplotype and phenotype analysis of six recurrent BRCA1 mutations in 61 families: results of an international study. In: American Journal of Human Genetics Volume 58, Number 2, February 1996, pp. 271-280, PMID 8571953 . PMC 1914544 (free full text).
- ^ Munich: New patent granted on breast cancer gene . In: Welt Online , December 1, 2001
- ↑ No comprehensive patent on the breast cancer gene. Greenpeace , September 28, 2007, accessed February 15, 2017 .